Abstract
Background
Given the knowledge of the damage caused by prolonged invasive mechanical ventilation in premature newborns, withdrawing this support as quickly as possible is important to minimize morbidity. The aim of this study was to analyze the variables associated with extubation outcomes and to develop a predictive model for successful extubation in premature newborns.
Methods
Data were obtained from a multicenter study involving six public maternity hospitals. The variables with the highest correlation to the extubation outcome were used to construct the predictive model through data analysis and machine learning methods, followed by training and testing of algorithms.
Results
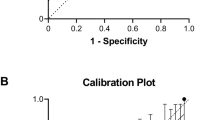
Data were collected from 405 premature newborns. The predictive model with the best metrics was trained and tested using the variables of gestational age, birth weight, weight at extubation, congenital infections, and time on invasive mechanical ventilation, based on 393 samples according to the extubation outcome (12 were discarded due to irretrievable missing data in important attributes). The model exhibited an accuracy of 77.78%, sensitivity of 79.41%, and specificity of 60%.
Conclusion
These variables generated a predictive model capable of estimating the probability of successful extubation in premature newborns.
Impact
-
Prolonged use of invasive mechanical ventilation in preterm newborns increases morbidity/mortality rates, emphasizing the importance of early withdrawal from invasive ventilatory support. However, the decision to extubate lacks tools with higher extubation outcome precision.
-
The use of artificial intelligence through the construction of a predictive model can assist in the decision-making process for extubating preterm newborns based on real-world data.
-
The implementation of this tool can optimize the decision to extubate preterm newborns, promoting successful extubation and reducing preterm newborns exposure to adverse events associated with extubation failure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Stoll, B. J. et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA 314, 103951 (2015).
Chawla, S. et al. Markers of successful extubation in extremely preterm infants, and morbidity after failed extubation. J. Pediatr. 189, 113–119 (2017).
Espíndola C. S. et al. Factors associated with the use of oxygen therapy and ventilatory support in premature newborns. Rev Pesqui Fisioter 12, https://doi.org/10.17267/2238-2704rpf.2022.e4921 (2022).
Vliegenthart, R. J. S., van Kaan, A. H., Aarnoudse-Moens, C. S. H., van Wassenaer, A. G. & Onland, W. Duration of mechanical ventilation and neurodevelopment in preterm infants. Arch. Dis. Child Fetal Neonatal Ed. 104, 631–635 (2019).
Choi, Y. B., Lee, J., Park, J. & Jun, Y. H. Impact of prolonged mechanical ventilation in very low birth weight infants: results from a national cohort study. J. Pediatr. 194, 34–39 (2018).
Gupta, D. et al. Respiratory setback associated with extubation failure in extremely preterm infants. Pediatr. Pulmonol. 56, 2081–2086 (2021).
Kidman, A. M., Manley, B. J., Boland, R. A., Davis, P. G. & Bhatia, R. Predictor and outcomes of extubation failure in extremely preterm infants. J. Paediatr. Child Health 57, 913–919 (2021).
Ministry of Health of Brazil.Maternal and Neonatal care: NHA provides important data in supplementary health. National Supplementary Health Agency, 2022. Available in: https://www.gov.br/ans/pt-br/assuntos/noticias/sobre-ans/atencao-materna-e-neonatal-ans-disponibiliza-dados-importantes-na-saude-suplementar
Kwok, T. C. et al. Application and potential of artificial intelligence in neonatal medicine. Semin Fetal Neonatal Med 27, 101346 (2022).
Dai D. et al. Bronchopulmonary dysplasia predicted by developing a machine learning model of genetic and clinical information. Front Genet. 12, https://doi.org/10.3389/fgene.2021.689071 (2021).
Cabrera-Quiros, L., kommers, D., Wolvers, M. K. & Oosterwijk, L. Prediction of late-onset sepsis in preterm infants using monitoring signals and machine learning. Crit. Care Explor 3, e0302 (2021).
Jin, Y. et al. Identification of infants at high-risk for autism spectrum disorder using multiparameter multiscale White matter connectivity networks. Hum. Brain Mapp. 36, 4880–4896 (2015).
Mueller, M. et al. Predicting extubations outcome in preterm newborns: a comparison of neural networks with clinical expertise and statistical modeling. Pediatr. Res. 56, 11–18 (2004).
Mueller, M., Almeida, J. S., Stanislaus, R. & Wagner, C. L. Can machine learning methods predict extubation outcome in premature infants as well as cliniciams? J. Neonatal Biol. 2, 1000118 (2013).
Kanbar, L. J. et al. Automated prediction of extubation success in extremely preterm infants: the APEX multicenter study. Pediatr. Res 93, 1041–1049 (2023).
Portney, L. G. Foundations of Clinical Research: Applications to Evidence-Based Practice. 4th edn (ed. Davis, F. A.) (2020).
Rossum, G. V. Python reference manual. Department of Computer Science, CWI (1995).
Chollet, F. Keras. GitHub, 2015. Available: https://github.com/keras-team/keras.
Ohnstad, M. O., Stensvold, H. J., Tvedt, C. R. & Ronnestad, A. E. Duration of mechanical ventilation and extubation success among extremely premature infants. Neonatology 118, 90–97 (2021).
He, F. et al. Predictors of extubation outcomes among extremely and very preterm infants: a retrospective cohort study. J. Pediatr. 98, 648–654 (2022).
Shalish, W., Latremouille, S., Papenburg, J. & Sant’Anna, G. M. ’ Predictors of extubation readiness in preterm infants: a systematic review and meta-analysis. Arch. Dis. Child Fetal Neonatal 104, F89–F97 (2019).
Shalish, W. et al. The impact of time interval between extubation and reintubation on death or bronchopulmonary dysplasia in extremely preterm infants. J. Pediatr. 205, 70–76 (2018).
Ohnstad, M. O. et al. Predictors of extubation success: a population-based study of neonates below a gestacional age of 26 weeks. BMJ Paediatrics Open 6, e001542 (2022).
Manley, B., Doyle, L. W., Owen, L. S. & Davis, P. G. Extubating extremely preterm infants: predictors of success and outcomes following failure. J. Pediatr. 173, 45–49 (2016). 2016.
World Health Organization. Preterm birth [internet]. Geneva: WHO, up date Feb 2018. Disponível em: http://www.who.int/mediacenter/factsheets/fs363/en/
Teixeira, R. F. et al. Factors associated with extubation failure in very low birth weight infants: a cohort study in the northeast Brazil. J. Perinat. Med 49, 506–513 (2021).
Oswaldo Cruz Foundation.National Institute of health for women, children and adolescents Fernandes Figueira. Portal of best practices in Women’s, Children’s, and Adolescent Health: minimal handling of the newborn, 2018. Available: http://portaldeboaspraticas.iff.fiocruz.br/atencao/recem-nascido/manuseio-minimo-do-recem-nascido/.
Lourenço, A. F. E. et al. TORCH group infections: epidemiological and laboratory analysis of a high-risk pregnancy group enphasis no toxoplasma gondii infections. Rev Goiana de Medicina 45, 11–16 (2014).
Gupta, D. et al. A predictive model for extubation readiness in extremely preterm infants. J. Perinatol. 39, 1663–1669 (2019).
Patino, C. M. & Ferreira, J. C. Internal and external validity: can you apply research study results to your patinete? J. Bras. Pneumol. 44, 183–183 (2018).
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: Camila S. Espíndola, Yuri K Lopes, Grasiela S Ferreira, Emanuella C Cordeiro, Silvana A Pereira, Dayane Montemezzo. Drafting the article or revising it critically for important intellectual content: Camila S. Espíndola, Yuri K Lopes, Grasiela S Ferreira, Dayane Montemezzo. Final approval of the version to be published: Camila S. Espíndola, Yuri K Lopes, Grasiela S Ferreira, Emanuella C Cordeiro, Silvana A Pereira, Dayane Montemezzo.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Patient consente was not required. This study was approved by the Human Research Ethics Committee of UDESC - CAAE 36371320.5.1001.0118. In accordance with the Brazilian resolution (CNS N° 510/2016), this study did not require consente term as it involved secondary data without identifying participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Espíndola, C.S., Lopes, Y.K., Ferreira, G.S. et al. Predictive model development for premature infant extubation outcomes: development and analysis. Pediatr Res 97, 2423–2430 (2025). https://doi.org/10.1038/s41390-024-03643-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-024-03643-0