Abstract
Background
Outcome prediction after preterm birth is important for long-term neonatal care, but has proven notoriously challenging for neurocognitive outcome. This study investigated the potential of machine learning to improve neurocognitive outcome prediction at two and five years of corrected age in preterm infants, using readily available predictors from the neonatal setting.
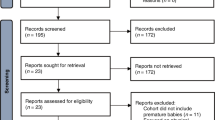
Methods
Predictors originating from the antenatal and neonatal period of preterm infants born <30 weeks gestation were used to predict adverse neurocognitive outcome on the Bayley Scale and Wechsler Preschool and Primary Scale of Intelligence. Machine learning models were compared to conventional logistic regression and validated using internal cross-validation.
Results
Best performing models were a random forest (two-year outcome) and a support vector machine (five-year outcome) with an area under the receiver operating characteristic curve (AUC) of 0.682 and 0.695 respectively, reaching high negative predictive values (95% and 91%, respectively). These models performed significantly better than the conventional models.
Conclusions
The models reached moderate overall predictive performance, yet with promising potential for early identification of children without adverse neurocognitive outcome. Machine learning modestly improved neurocognitive outcome prediction. Future research may harvest the predictive potential of a wider variety of routine (clinical) data, such as vital sign time series.
Impact
-
Early prediction of neurocognitive outcome in preterm infants will enable targeted follow-up and deployment of early (preventative) interventions to improve outcome.
-
Neurocognitive outcome remains notoriously challenging using conventional models, while existing machine learning models depend on advanced MRI-derived predictors with limited potential for implementation into daily clinical practice.
-
This study developed machine learning models for neurocognitive outcome prediction using predictors that are readily available in neonatal settings.
-
Neurocognitive outcome prediction remains challenging due to low AUC and PPV, however, the models demonstrate high NPV, indicating potential for identifying children at low risk for adverse outcome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets analyzed during the current study are not publicly available due to privacy restrictions on the medical data. However, they are available from the corresponding author on reasonable request, subject to compliance with privacy regulations.
References
Allotey, J. et al. Cognitive, Motor, Behavioural and Academic Performances of Children Born Preterm: A Meta-Analysis and Systematic Review Involving 64 061 Children. BJOG 125, 16–25 (2018).
Stoll, B. J. et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993-2012. JAMA 314, 1039–1051 (2015).
Twilhaar, E. S. et al. Cognitive Outcomes of Children Born Extremely or Very Preterm since the 1990s and Associated Risk Factors: A Meta-Analysis and Meta-Regression. JAMA Pediatr. 172, 361–367 (2018).
Gottfredson, L. S. Intelligence: Is It the Epidemiologists’ Elusive “Fundamental Cause” of Social Class Inequalities in Health? J. Pers. Soc. Psychol. 86, 174–199 (2004).
Koenen, K. C. et al. Childhood Iq and Adult Mental Disorders: A Test of the Cognitive Reserve Hypothesis. Am. J. Psychiatry 166, 50–57 (2009).
Petrill, S. A. & Wilkerson, B. Intelligence and Achievement: A Behavioral Genetic Perspective. Educ. Psychol. Rev. 12, 185–199 (2000).
Strenze, T. Intelligence and Socioeconomic Success: A Meta-Analytic Review of Longitudinal Research. Intelligence 35, 401–426 (2007).
van Beek, P. E. et al. Two-Year Neurodevelopmental Outcome in Children Born Extremely Preterm: The Epi-Daf Study. Arch. Dis. Child Fetal Neonatal Ed. 107, 467–474 (2022).
Johnson, K. B. et al. Precision Medicine, Ai, and the Future of Personalized Health Care. Clin. Transl. Sci. 14, 86–93 (2021).
Hadders-Algra, M. Early Diagnosis and Early Intervention in Cerebral Palsy. Front. Neurol. 5, 185 (2014).
Jeukens-Visser, M. et al. Development and Nationwide Implementation of a Postdischarge Responsive Parenting Intervention Program for Very Preterm Born Children: The Top Program. Infant Ment. Health J. 42, 423–437 (2021).
Kitsios, G. D. & Kent, D. M. Personalised Medicine: Not Just in Our Genes. BMJ 344, e2161 (2012).
Statline. Zorguitgaven; Kerncijfers, (2023). https://opendata.cbs.nl/#/CBS/nl/dataset/84047NED/table.
Crilly, C. J., Haneuse, S. & Litt, J. S. Predicting the Outcomes of Preterm Neonates Beyond the Neonatal Intensive Care Unit: What Are We Missing? Pediatr. Res. 89, 426–445 (2021).
Lodha, A., Sauve, R., Chen, S., Tang, S. & Christianson, H. Clinical Risk Index for Babies Score for the Prediction of Neurodevelopmental Outcomes at 3 Years of Age in Infants of Very Low Birthweight. Dev. Med. Child Neurol. 51, 895–900 (2009).
Greenwood, S. et al. Can the Early Condition at Admission of a High-Risk Infant Aid in the Prediction of Mortality and Poor Neurodevelopmental Outcome? A Population Study in Australia. J. Paediatr. Child Health 48, 588–595 (2012).
Van’t Hooft, J. et al. Predicting Developmental Outcomes in Premature Infants by Term Equivalent Mri: Systematic Review and Meta-Analysis. Syst. Rev. 4, 71 (2015).
van Boven, M. R. et al. Machine Learning Prediction Models for Neurodevelopmental Outcome after Preterm Birth: A Scoping Review and New Machine Learning Evaluation Framework. Pediatrics 150, e2021056052 (2022).
Lonsdale, H., Jalali, A., Ahumada, L. & Matava, C. Machine Learning and Artificial Intelligence in Pediatric Research: Current State, Future Prospects, and Examples in Perioperative and Critical Care. J. Pediatr. 221S, S3–S10 (2020).
Girault, J. B. et al. White Matter Connectomes at Birth Accurately Predict Cognitive Abilities at Age 2. Neuroimage 192, 145–155 (2019).
Saha, S. et al. Predicting Motor Outcome in Preterm Infants from Very Early Brain Diffusion Mri Using a Deep Learning Convolutional Neural Network (Cnn) Model. Neuroimage 215, 116807 (2020).
FDA Drug Safety Communication: FDA Review Results in New Warnings About Using General Anesthetics and Sedation Drugs in Young Children and Pregnant Women, https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-review-results-new-warnings-about-using-general-anesthetics-and (2016).
Juul, S. E. et al. Predicting 2-Year Neurodevelopmental Outcomes in Extremely Preterm Infants Using Graphical Network and Machine Learning Approaches. EClinicalMedicine 56, 101782 (2023).
Ambalavanan, N. et al. Early Prediction of Poor Outcome in Extremely Low Birth Weight Infants by Classification Tree Analysis. J. Pediatr. 148, 438–444 (2006).
Ambalavanan, N. et al. Prediction of Neurologic Morbidity in Extremely Low Birth Weight Infants. J. Perinatol. 20, 496–503 (2000).
Luttikhuizen dos Santos, E. S., de Kieviet, J. F., Konigs, M., van Elburg, R. M. & Oosterlaan, J. Predictive Value of the Bayley Scales of Infant Development on Development of Very Preterm/Very Low Birth Weight Children: A Meta-Analysis. Early Hum. Dev. 89, 487–496 (2013).
Luo, W. et al. Guidelines for Developing and Reporting Machine Learning Predictive Models in Biomedical Research: A Multidisciplinary View. J. Med Internet Res 18, e323 (2016).
Collins, G. S., Reitsma, J. B., Altman, D. G. & Moons, K. G. Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (Tripod): The Tripod Statement. BMJ 350, g7594 (2015).
Bayley, N. Bayley Scales of Infant and Toddler Development, Third Edition, San Antonio, TX: Harcourt Assessment, 2006.
Hendriksen, J. & Hurks, P. WPPSI III Wechsler Preschool and Primary Scale of Intelligence Nederlandse bewerking (3rd ed), Pearson Assessment and Information BV. Amsterdam 2009.
Davison, A. C. & Hinkley, D. V. Bootstrap Methods and Their Application (Cambridge University Press, 1997).
Kelly, C. J., Karthikesalingam, A., Suleyman, M., Corrado, G. & King, D. Key Challenges for Delivering Clinical Impact with Artificial Intelligence. BMC Med. 17, 195 (2019).
Menze, B. H. et al. A Comparison of Random Forest and Its Gini Importance with Standard Chemometric Methods for the Feature Selection and Classification of Spectral Data. BMC Bioinforma. 10, 213 (2009).
Molnar, C. Interpretable Machine Learning, 2 edn (2022). https://christophm.github.io/interpretable-ml-book.
Mandrekar, J. N. Receiver Operating Characteristic Curve in Diagnostic Test Assessment. J. Thorac. Oncol. 5, 1315–1316 (2010).
EFCNI, Wolke, D. & Leemhuis, A. G. European Standards of Care for Newborn Health: Cognitive development. (2018).
He, L. et al. A Multi-Task, Multi-Stage Deep Transfer Learning Model for Early Prediction of Neurodevelopment in Very Preterm Infants. Sci. Rep. 10, 15072 (2020).
Poldrack, R. A., Huckins, G. & Varoquaux, G. Establishment of Best Practices for Evidence for Prediction: A Review. JAMA Psychiatry 77, 534–540 (2020).
Rajput, D., Wang, W. J. & Chen, C. C. Evaluation of a Decided Sample Size in Machine Learning Applications. BMC Bioinforma. 24, 48 (2023).
Flynn, R. S., Huber, M. D. & DeMauro, S. B. Predictive Value of the Bsid-Ii and the Bayley-Iii for Early School Age Cognitive Function in Very Preterm Infants. Glob Pediatr Health 7, 2333794X20973146 (2020).
Anderson, P. J. et al. Underestimation of Developmental Delay by the New Bayley-Iii Scale. Arch. Pediatr. Adolesc. Med. 164, 352–356 (2010).
Bancalari, E. & del Moral, T. Bronchopulmonary Dysplasia and Surfactant. Biol. Neonate 80, 7–13 (2001).
Jobe, A. H. & Bancalari, E. Bronchopulmonary Dysplasia. Am. J. Respir. Crit. Care Med 163, 1723–1729 (2001).
Author information
Authors and Affiliations
Contributions
Van Boven: Conceptualization, Methodology, Validation, Formal analysis, Data Curation, Writing – Original Draft, Visualization, Project administration. Bennis: Methodology, Software, Validation, Formal analysis, Data Curation, Writing – Review & Editing. Frings, Tran: Methodology, Software, Validation, Writing: Review & Editing. Onland, Aarnoudse-Moens, Katz, Romijn: Resources, Data Curation, Writing – Review & Editing. Leemhuis, Van Kaam: Conceptualization, Methodology, Resources, Writing – Review & Editing. Hoogendoorn: Methodology, Writing- Review & Editing, Supervision. Oosterlaan, Königs: Conceptualization, Methodology, Writing – Review & Editing, Supervision, Project administration.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
All procedures and data-gathering was part of the routine care. The re-use of the data for this study was approved by the medical ethical committee of the Academic Medical Centre (registration-number: W21_516 # 21.569), and in accordance with the 1964 Declaration of Helsinki and its later amendments. Parents of the included infants provided informed consent to re-use their data for scientific purpose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
van Boven, M.R., Bennis, F.C., Onland, W. et al. Machine learning models for neurocognitive outcome prediction in preterm born infants. Pediatr Res 98, 942–949 (2025). https://doi.org/10.1038/s41390-025-03815-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-025-03815-6
This article is cited by
-
Machine learning for outcome prediction in preterm infants: opportunities and challenges
Pediatric Research (2025)