Abstract
Background
Early identification is crucial for children with autism. However, many children are diagnosed later due to the lack of specific assessment tools in primary care settings. The study aims to evaluate the effectiveness of the STAT in screening autism across different age groups while assessing its advantages and limitations.
Methods
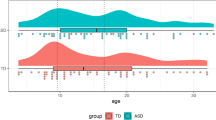
In total, 434 children aged 14–48 months visiting autism clinics from March to December 2021 were included. Subjects were grouped by age (14–23, 24–36, and 37–48 months) and categorized based on clinical evaluations and STAT results.
Results
In the age groups of 14–23 and 24–36 months, STAT results demonstrated high sensitivity and specificity compared to DSM-5 diagnoses and exhibited better consistency with ADOS-2 results. However, its performance was weaker in the 37–48 months group. False-negative results were associated with less pronounced autistic traits and higher developmental quotients.
Conclusion
STAT presents as a promising level 2 screening tool for early autism identification in China, but its accuracy diminishes in older children with less pronounced autistic traits. These findings emphasize the need for comprehensive assessment strategies for autism diagnosis across different age groups and varying levels of support needs.
Impact
-
This study evaluates the effectiveness of the Screening Tool for Autism in Toddlers (STAT) for early screening of autism across different age groups.
-
It highlights STAT’s effectiveness in younger age groups but emphasizes its limitations with older children and those with less pronounced autistic traits.
-
The findings supplement existing literature by providing insights into STAT’s utility in diverse populations.
-
The impact lies in guiding clinical practice to improve the identification of autistic characteristics, particularly in resource-limited settings, potentially enhancing early support and outcomes for autistic children.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All the data and materials are available. The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
References
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition [Internet]. American Psychiatric Association; Available from: https://doi.org/10.1176/appi.books.9780890425596 (2013).
Maenner, M. J. et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years — autism and developmental disabilities monitoring network, 11 sites, United States, 2020. MMWR Surveill. Summ. 72, 1–14 (2023).
Lavelle, T. A. et al. Economic burden of childhood autism spectrum disorders. Pediatrics 133, e520–e529 (2014).
Rogge, N. & Janssen, J. The economic costs of autism spectrum disorder: A literature review. J. Autism Dev. Disord. 49, 2873–2900 (2019).
Zhou, W. et al. Effect of time interval from diagnosis to treatment on economic burden in families of children with autism spectrum disorder. Front Psychiatry 12, 679542 (2021).
Landa, R. J. Efficacy of early interventions for infants and young children with, and at risk for, autism spectrum disorders. Int. Rev. Psychiatry 30, 25–39 (2018).
Kodak, T. & Bergmann, S. Autism spectrum disorder: Associated behaviors, and early intervention. Pediatr. Clin. North Am. 67, 525–535 (2020).
Lord, C. et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J. Autism Dev. Disord. 30, 205–223 (2000).
Weitlauf, A. S., et al. Therapies for children with autism spectrum disorder: behavioral interventions update. agency for healthcare research and quality (US) [Internet]. 2014; Available from: https://pubmed.ncbi.nlm.nih.gov/25210724/.
Lord, C., Elsabbagh, M., Baird, G. & Veenstra-Vanderweele, J. Autism spectrum disorder. Lancet 392, 508–520 (2018).
McConachie, H. et al. Systematic review of tools to measure outcomes for young children with autism spectrum disorder. Health Technol. Assess. 19, 1–506 (2015).
Guo, C. et al. Reliability and validity of the chinese version of modified checklist for autism in toddlers, revised, with follow-up (M-CHAT-R/F). J. Autism Dev. Disord. 49, 185–196 (2019).
Stone, W. L., Coonrod, E. E. & Ousley, O. Y. Brief report: screening tool for autism in two-year-olds (STAT): development and preliminary data. J. Autism Developmental Disord. 30, 607–612 (2000).
Stone, W. L., Coonrod, E. E., Turner, L. M. & Pozdol, S. L. Psychometric properties of the STAT for early autism screening. J. Autism Dev. Disord. 34, 691–701 (2004).
Stone, W. L., McMahon, C. R. & Henderson, L. M. Use of the screening tool for autism in two-year-olds (STAT) for children under 24 months: An exploratory study. Autism 12, 557–573 (2008).
Zwaigenbaum, L. The Screening Tool for Autism in Two Year Olds can identify children at risk of autism. Evid.-Based Ment. Health 8, 69–69 (2005).
Butler S., Lord C. Autism Screening Instrument for Educational Planning (ASIEP-2). Springer New York. 2013.
Dawkins, T., Meyer, A. T. & Van Bourgondien, M. E. The relationship between the childhood autism rating scale: Second edition and clinical diagnosis utilizing the DSM-IV-TR and the DSM-5. J. Autism Dev. Disord. 46, 3361–3368 (2016).
Tso, W. W. Y. et al. The Griffiths Development Scales-Chinese (GDS-C): A cross-cultural comparison of developmental trajectories between Chinese and British children. Child 44, 378–383 (2018).
Wu, C.-C., Chiang, C.-H., Chu, C.-L., Iao, L.-S. & Hou, Y.-M. T-STAT for detecting autism spectrum disorder in toddlers aged 18–24 months. Autism 25, 911–920 (2021).
Chiang, C.-H. et al. Development of T-STAT for early autism screening. J. Autism Dev. Disord. 43, 1028–1037 (2013).
Hosozawa, M. et al. Determinants of an autism spectrum disorder diagnosis in childhood and adolescence: Evidence from the UK Millennium Cohort Study. Autism 24, 1557–1565 (2020).
Mandell, D. S., Novak, M. M. & Zubritsky, C. D. Factors associated with age of diagnosis among children with autism spectrum disorders. Pediatrics 116, 1480–1486 (2005).
Turner, L. M. & Stone, W. L. Variability in outcome for children with an ASD diagnosis at age 2. Child Psychol. Psychiatry 48, 793–802 (2007).
Mazurek, M. O. et al. Age at first autism spectrum disorder diagnosis: The role of birth cohort, demographic factors, and clinical features. J. Dev. Behav. Pediatrics 35, 561–569 (2014).
Wu, C.-C., Chiang, C.-H., Hou, Y.-M., Chu, C.-L. & Liu, J.-H. Utility of the Taiwan version of the Screening Tool for Autism in Two-Year-Olds to detect autism in children aged three years. J. Intellect. Dev. Disabil. 44, 337–345 (2019).
Fountain, C., King, M. D. & Bearman, P. S. Age of diagnosis for autism: individual and community factors across 10 birth cohorts. J. Epidemiol. Community Health 65, 503–510 (2011).
Sheldrick, R. C., Maye, M. P. & Carter, A. S. Age at first identification of autism spectrum disorder: An analysis of Two US surveys. J. Am. Acad. Child Adolesc. Psychiatry 56, 313–320 (2017).
Zwaigenbaum, L. et al. Developmental functioning and symptom severity influence age of diagnosis in Canadian preschool children with autism. Paediatr. Child Health 24, e57–e65 (2019).
Wu, C.-C. & Chiang, C.-H. The developmental sequence of social-communicative skills in young children with autism: A longitudinal study. Autism 18, 385–392 (2014).
Hepburn, S. & Stone, W. L. Longitudinal Research on Motor Imitation in Autism https://www.researchgate.net/publication/232489616_Longitudinal_Research_on_Motor_Imitation_in_Autism Available from.
Stone, W. L., Ousley, O. Y. & Littleford le, C. D. Motor imitation in young children with autism: What’s the object? J. Abnorm. Child Psychol. 25, 475–485 (1997).
Acknowledgements
This study was supported by the Science and Technology Department of Jilin Province (Grant No.: 20230203067SF), The Health Science and Technology Capacity Improvement Project of Jilin Province (Grant Number: 2022LC104), and Tianhua Health Foundation of Jilin Province(Grant Number: J2022JKJ019).
Author information
Authors and Affiliations
Contributions
F.-Y.J., M.S.B., and Y.X. significantly contribute to concept and design, data acquisition, and data analysis and interpretation. H.Y.D. and Z.A.M. critically revise articles and provide important intellectual content. All authors contributed to and have approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of the Kunming Changhe Tiancheng Rehabilitation Hospital. Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bai, M., Xue, Y., Dong, H. et al. Autism screening tool validation for toddlers and young children: advantages and limitations. Pediatr Res 98, 1039–1045 (2025). https://doi.org/10.1038/s41390-025-03848-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-025-03848-x