Abstract
Objective
This cross-sectional study examined depression and associated impairment in youth presenting to a pediatric emergency department (PED) with abdominal pain.
Methods
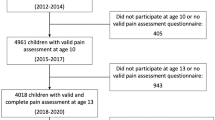
Participants were 11–17 years old, presenting to a PED with idiopathic abdominal pain. Participants completed demographics, pain, pain-related impairment, and depression surveys. Depression was assessed using the Patient Health Questionnaire (PHQ-9A). Scores ≥10 met depression threshold and ≥1 on item 9 indicated self-harm ideation. Mean difference and logistic regression analyses were conducted.
Results
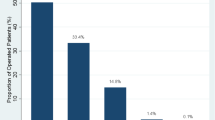
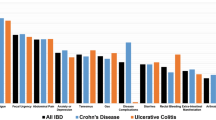
Among 169 participants, 29.6% reported depression and 9.4% endorsed self-harm ideation. Depression was associated with Latinx ethnicity (X2 = 4.02, p = 0.045), higher pain intensity (Z = −3.09, p = 0.002), and higher pain-related impairment (Z = −4.86, p < 0.001). In regression analyses, pain-related impairment and Latinx ethnicity were independently associated with depression (OR = 3.89 [95%CI, 1.22–12.40]; OR = 1.13 [95%CI, 1.06–1.21]). Self-harm ideation was not associated with study variables.
Conclusions
Results highlight the need for enhanced mental health screening for youth presenting with idiopathic abdominal pain in the ED, particularly for Latinx youth. Early identification of depression and high pain-related impairment may inform interventions and improve outcomes.
Impact
-
Nearly 30% of youth, 11–17 years old, presenting to the ED with idiopathic abdominal pain screened positive for depression and 9.4% reported self-harm ideation.
-
The higher likelihood of depression among Latinx youth experiencing pain emphasizes the importance of including diverse samples in future ED research to explore mechanisms contributing to poorer mental health in minoritized populations.
-
Results highlight the need for enhanced mental health screening in youth presenting to the emergency department with idiopathic abdominal pain.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The de-identified dataset analyzed during the current study are available from the corresponding author upon reasonable request.
References
Soltani, S., Kopala-Sibley, D. C. & Noel, M. The co-occurrence of pediatric chronic pain and depression. Clinical Journal of Pain 35, 633–643 (2019).
Campo, J. V. et al. Recurrent Abdominal Pain, Anxiety, and Depression in Primary Care. Pediatrics 113, 817–824 (2004).
Hyams, J. S., Burke, G., Davis, P. M., Rzepski, B. & Andrulonis, P. A. Abdominal pain and irritable bowel syndrome in adolescents: a community-based study. The Journal of Pediatrics 129, 220–226 (1996).
Youssef, N. N., Atienza, K., Langseder, A. L. & Strauss, R. S. Chronic Abdominal Pain and Depressive Symptoms: Analysis of the National Longitudinal Study of Adolescent Health. Clinical Gastroenterology and Hepatology 6, 329–332 (2008).
Cunningham, N. R. et al. Risk categorization predicts disability in pain-associated functional gastrointestinal disorders (FGIDs) after 6 months. J Pediatr Gastroenterol Nutr 64, 685–690 (2017).
Mulvaney, S., Lambert, E. W., Garber, J. & Walker, L. S. Trajectories of symptoms and impairment for pediatric patients with functional abdominal pain: a 5-year longitudinal study. Journal of the American Academy of Child & Adolescent Psychiatry 45, 737–744 (2006).
Stone, A. L. et al. Subgroups of Pediatric Patients With Functional Abdominal Pain: Replication, Parental Characteristics, and Health Service Use. The Clinical Journal of Pain 36, 897–906 (2020).
Caperell, K., Pitetti, R. & Cross, K. P. Race and Acute Abdominal Pain in a Pediatric Emergency Department. Pediatrics 131, 1098–1106 (2013).
Pollack, E. S. Pediatric abdominal surgical emergencies. Pediatric Annals 25, 448–457 (1996).
Smith, J. & Fox, S. M. Pediatric abdominal pain: an emergency medicine perspective. Emergency Medicine Clinics 34, 341–361 (2016).
Lee, W. H. et al. Pediatric Abdominal Pain in Children Presenting to the Emergency Department. Pediatr Emerg Care 37, 593–598 (2021).
Pennel, D. J. L., Goergen, N. & Driver, C. P. Nonspecific abdominal pain is a safe diagnosis. Journal of Pediatric Surgery 49, 1602–1604 (2014).
Loening-Baucke, V. & Swidsinski, A. Constipation as Cause of Acute Abdominal Pain in Children. The Journal of Pediatrics 151, 666–669 (2007).
Rinderknecht, A. S., Ho, M., Matykiewicz, P. & Grupp-Phelan, J. M. Referral to the Emergency Department by a Primary Care Provider Predicts Severity of Illness. Pediatrics 126, 917–924 (2010).
Doan, Q. et al. Utility of MyHEARTSMAP for Universal Psychosocial Screening in the Emergency Department. The Journal of Pediatrics 219, 54–61.e1 (2020).
Lipsitz, J. D. et al. Psychopathology and disability in children with unexplained chest pain presenting to the pediatric emergency department. Pediatr Emerg Care 26, 830–836 (2010).
Scott, E. G., Luxmore, B., Alexander, H., Fenn, R. L. & Christopher, N. C. Screening for Adolescent Depression in a Pediatric Emergency Department. Academic Emergency Medicine 13, 537–542 (2006).
Walker, L. S., Sherman, A. L., Bruehl, S., Garber, J. & Smith, C. A. Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric comorbidities in adolescence and adulthood. PAIN 153, 1798–1806 (2012).
Wuerz, R. C., Milne, L. W., Eitel, D. R., Travers, D. & Gilboy, N. Reliability and Validity of a New Five-level Triage Instrument. Academic Emergency Medicine 7, 236–242 (2000).
Williamson, A. & Hoggart, B. Pain: a review of three commonly used pain rating scales. Journal of Clinical Nursing 14, 798–804 (2005).
Dworkin, R. H. et al. Considerations for extrapolating evidence of acute and chronic pain analgesic efficacy. PAIN® 152, 1705–1708 (2011).
Treede, R.-D. et al. A classification of chronic pain for ICD-11. Pain 156, 1003–1007 (2015).
Kent, M. L. et al. The ACTTION–APS–AAPM Pain Taxonomy (AAAPT) Multidimensional Approach to Classifying Acute Pain Conditions. Journal of Pain 18, 479–489 (2017).
Varni, J. W. et al. PROMIS Pediatric Pain Interference Scale: an item response theory analysis of the pediatric pain item bank. Journal of Pain 11, 1109–1119 (2010).
Varni, J. W. et al. Psychometric properties of the PROMIS® pediatric scales: precision, stability, and comparison of different scoring and administration options. Quality of Life Research 23, 1233–1243 (2014).
Johnson, J. G., Harris, E. S., Spitzer, R. L. & Williams, J. B. The patient health questionnaire for adolescents: validation of an instrument for the assessment of mental disorders among adolescent primary care patients. Journal of Adolescent Health 30, 196–204 (2002).
Kroenke, K., Spitzer, R. L. & Williams, J. B. W. The PHQ-9. Journal of General Internal Medicine 16, 606–613 (2001).
Manea, L., Gilbody, S. & McMillan, D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ 184, E191–E196 (2012).
Gilbody, S., Richards, D., Brealey, S. & Hewitt, C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. Journal of General Internal Medicine 22, 1596–1602 (2007).
Gamwell, K. L., Mara, C. A., Hommel, K. A., Kashikar-Zuck, S. & Cunningham, N. R. Establishing Clinical Cut-points on the Pediatric PROMIS-Pain Interference Scale in Youth With Abdominal Pain. Clinical Journal of Pain 38, 173–181 (2022).
Falla, K. et al. Anxiety and Depressive Symptoms and Disorders in Children and Adolescents with Migraine: A Systematic Review and Meta-analysis. JAMA Pediatrics 176, 1176–1187 (2022).
Spatuzzo, M. et al. Abdominal pain in children: the role of possible psychosocial disorders. Eur Rev Med Pharmacol Sci 25, 1967–1973 (2021).
Tegethoff, M., Belardi, A., Stalujanis, E. & Meinlschmidt, G. Comorbidity of Mental Disorders and Chronic Pain: Chronology of Onset in Adolescents of a National Representative Cohort. The Journal of Pain 16, 1054–1064 (2015).
Wrona, S. K., Melnyk, B. M. & Hoying, J. Chronic Pain and Mental Health Co-Morbidity in Adolescents: An Urgent Call for Assessment and Evidence-Based Intervention. Pain Management Nursing 22, 252–259 (2021).
Anderson, K. O., Green, C. R. & Payne, R. Racial and ethnic disparities in pain: causes and consequences of unequal care. Journal of Pain 10, 1187 (2009).
Green, C. R. et al. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Medicine 4, 277–294 (2003).
Hooper, L. M., Mier-Chairez, J., Mugoya, G. C. T. & Arellano, B. Depressive symptoms, assessment, and treatment in Latino/a adolescents: A brief review. Current Psychiatry Reviews 12, 150–162 (2016).
Garcia, C., Skay, C., Sieving, R., Naughton, S. & Bearinger, L. H. Family and Racial Factors Associated With Suicide and Emotional Distress Among Latino Students. Journal of School Health 78, 487–495 (2008).
Flores, G. et al. The health of Latino children: urgent priorities, unanswered questions, and a research agenda. Jama 288, 82–90 (2002).
Kemper, A. R., Hostutler, C. A., Beck, K., Fontanella, C. A. & Bridge, J. A. Depression and Suicide-Risk Screening Results in Pediatric Primary Care. Pediatrics 148, e2021049999 (2021).
Shain, B. et al. Suicide and suicide attempts in adolescents. Pediatrics 138, e20161420 (2016).
Acknowledgements
Dr. Sarah R. Martin is supported by the National Institutes of Health National Institute for Child Health and Human Development [K23HD105042, PI: Martin].
Author information
Authors and Affiliations
Contributions
Each author has met the Pediatric Research authorship requirements. The authors that met each criterion are listed below. Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: Drs. Martin, Heyming, Fortier, Huszti, Dennis, Kain, and Mr. Salas Drafting the article or revising it critically for important intellectual content: Drs. Martin, Heyming, Fortier, Huszti, Dennis, Kain, and Mr. Salas. Final approval of the version to be published: Drs. Martin, Heyming, Fortier, Huszti, Dennis, Kain, and Mr. Salas.
Corresponding author
Ethics declarations
Competing interests
Dr. Zeev N. Kain serves as a consultant for Edwards Life Sciences and Pacira and is the President of the American College of Perioperative Medicine. All other authors have no conflicts of interest to report.
Ethical approval and consent to participate
Parents provided informed consent and children provided assent prior to participating in the study. Ethical approval for all study procedures was obtained from the Children’s Hospital of Orange County Institutional Review Board (#220577).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Martin, S.R., Heyming, T.W., Fortier, M.A. et al. Depression in children with abdominal pain in the emergency department. Pediatr Res 98, 1033–1038 (2025). https://doi.org/10.1038/s41390-025-03871-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-025-03871-y