Abstract
Background
Newborns with Neonatal Opioid Withdrawal Syndrome (NOWS) are at risk for smaller size at birth, including weight, length, and head circumference. We hypothesized that children with a history of prenatal opioid exposure and NOWS would have smaller size as infants and toddlers.
Methods
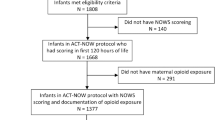
This retrospective cohort study analyzed a cohort developed from the electronic medical records of all patients who were seen in the NOWS Clinic at a free-standing children’s hospital system through age two years. Anthropometric measurements, demographics, substance and pharmacologic exposures, custodian status and nutritional data were extracted.
Results
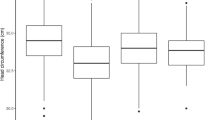
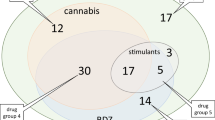
The final sample size included 1190 subjects with 7700 patient encounters. 1153 (97%) had four or more visits in the first two years of life. Forty-four percent of height measurements were below the tenth percentile. Prenatal methadone exposure was negatively associated with later growth. Infants with lower weight, height, and head circumference were prescribed higher caloric density infant formula. Forty percent of the weight measurements were less than the tenth percentile before 6 months, and this improved to 9.3% at 18–25-month visits.
Conclusion
Children with a history of prenatal opioid exposure are at risk for later short stature. Prenatal methadone exposure specifically is associated with decreased height.
Impact
-
This large retrospective cohort study found that toddlers with a history of prenatal opioid exposure and Neonatal Opioid Withdrawal Syndrome are at risk for short stature.
-
Prenatal methadone, but not buprenorphine, exposure is negatively associated with later growth in children with a history of prenatal opioid exposure.
-
The proportion of weight under the tenth percentile improved from infant to toddler ages in children with a history of prenatal opioid exposure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Jansson, L. M. & Patrick, S. W. Neonatal Abstinence Syndrome. Pediatr. Clin. North Am. 66, 353–367 (2019).
Benninger, K. L., McAllister, J. M. & Merhar, S. L. Neonatal Opioid Withdrawal Syndrome: An Update on Developmental Outcomes. Clin. Perinatol. 50, 17–29 (2023).
Weller, A. E., Crist, R. C., Reiner, B. C., Doyle, G. A. & Berrettini, W. H. Neonatal Opioid Withdrawal Syndrome (NOWS): A Transgenerational Echo of the Opioid Crisis. Cold Spring Harb. Perspect. Med. 11, a039669 (2021).
Kaplan, H. C. et al. Orchestrated Testing of Formula Type to Reduce Length of Stay in Neonatal Abstinence Syndrome. Pediatrics 146, e20190914 (2020).
Kanervo, M. et al. Intrauterine exposure to maternal opioid maintenance treatment and associated risk factors may impair child growth. Acta Paediatr. 113, 1579–1591 (2024).
Welle-Strand, G. K. et al. Neonatal outcomes following in utero exposure to methadone or buprenorphine: a National Cohort Study of opioid-agonist treatment of Pregnant Women in Norway from 1996 to 2009. Drug Alcohol Depend. 127, 200–206 (2013).
Corr, T. E., Schaefer, E. W. & Paul, I. M. Growth during the first year in infants affected by neonatal abstinence syndrome. BMC Pediatrics 18, 343 (2018).
Nathan, A. T. et al. A quality improvement initiative to reduce necrotizing enterocolitis across hospital systems. J. Perinatol. 38, 742–750 (2018).
Chou, J. H., Roumiantsev, S. & Singh, R. PediTools Electronic Growth Chart Calculators: Applications in Clinical Care, Research, and Quality Improvement. J. Med. Internet Res. 22, e16204 (2020).
Cutler, A. J., Cox, D. F., Gabrielson, S. M. B., Picarillo, A. P. & Craig, A. K. Association of medication-assisted treatment and short acting opioids with newborn head circumference and birth weight. J. Perinatol. 43, 277–282 (2023).
Leroy, J. L. & Frongillo, E. A. Perspective: What Does Stunting Really Mean? A Critical Review of the Evidence. Adv. Nutr. 10, 196–204 (2019).
Grummer-Strawn, L. M., Reinold, C. & Krebs, N. F. Use of World Health Organization and CDC growth charts for children aged 0-59 months in the United States. MMWR Recomm. Rep. 59, 1–15 (2010).
WHO Child Growth. Standards based on length/height, weight and age. Acta Paediatr. Suppl. 450, 76–85 (2006).
Lembeck, A. L. et al. Breastfeeding and Formula Selection in Neonatal Abstinence Syndrome. Am. J. Perinatol. 38, 1488–1493 (2021).
Merhar, S. L. et al. Infant Feeding and Weight Trajectories in the Eat, Sleep, Console Trial: A Secondary Analysis of a Randomized Clinical Trial. JAMA Pediatr. 178, 976–984 (2024).
Beck, A. F. et al. Forging a pediatric primary care-community partnership to support food-insecure families. Pediatrics 134, e564–e571 (2014).
Brogly, S. B., Saia, K. A., Walley, A. Y., Du, H. M. & Sebastiani, P. Prenatal buprenorphine versus methadone exposure and neonatal outcomes: systematic review and meta-analysis. Am. J. Epidemiol. 180, 673–686 (2014).
Minozzi, S., Amato, L., Bellisario, C., Ferri, M. & Davoli, M. Maintenance agonist treatments for opiate-dependent pregnant women. Cochrane Database Syst. Rev., 11, Cd006318 (2013).
Newman, R. G. & Gevertz, S. G. Efficacy versus effectiveness of buprenorphine and methadone maintenance in pregnancy. J. Addict. Dis. 30, 318–322 (2011).
Taleghani, A. A. et al. Buprenorphine pharmacotherapy for the management of neonatal abstinence syndrome in methadone-exposed neonates. Paediatr. Neonatal Pain. 1, 33–38 (2019).
Robinson, N., et al. The biological and social determinants of childhood obesity: comparison of two cohorts 50 years apart. J. Pediatr. 228, 138–146.e5 (2021).
March, M. et al. A retrospective observational study - exploring food pantry referral as a clinical proxy for residents’ ability to address unmet health-related social needs. Med Educ. Online 29, 2404295 (2024).
Randolph, A. et al. Improving Screening for Social Determinants of Health in an Outpatient Complex Care Clinic. Pediatrics 154, e2023063086 (2024).
Banderali, G. et al. Short and long term health effects of parental tobacco smoking during pregnancy and lactation: a descriptive review. J. Transl. Med. 13, 327 (2015).
Young, L. W. et al. Eat, Sleep, Console Approach or Usual Care for Neonatal Opioid Withdrawal. N. Engl. J. Med. 388, 2326–2337 (2023).
Patrick, S. W., Barfield, W. D. & Poindexter, B. B. Neonatal Opioid Withdrawal Syndrome. Pediatrics 146, a039669 (2020).
Trammel, C. J., Whitley, J. & Kelly, J. C. Pharmacotherapy for opioid use disorder in pregnancy. Curr. Opin. Obstet. Gynecol. 36, 74–80 (2024).
Christianson, H. L. et al. Outcomes of Neonates Exposed to Buprenorphine versus Methadone in Utero: A Systematic Review and Meta-Analysis of Safety in the Fetus and Neonate. Reprod. Med. 2, 185–194 (2021).
Suarez, E. A. et al. Buprenorphine versus Methadone for Opioid Use Disorder in Pregnancy. N. Engl. J. Med. 387, 2033–2044 (2022).
Cho, H. et al. Head growth during neonatal intensive care unit stay is related to the neurodevelopmental outcomes of preterm small for gestational age infants. Pediatr. Neonatol. 62, 606–611 (2021).
Connery, A. K. et al. A prospective cohort study of head circumference and its association with neurodevelopmental outcomes in infants and young children in rural Guatemala. J. Dev. Orig. Health Dis. 13, 779–786 (2022).
Lamb, M. M. et al. Anthropometric proxies for child neurodevelopment in low-resource settings: length- or height-for-age, head circumference or both? J. Dev. Orig. Health Dis. 14, 61–69 (2023).
Yen, E. & Maron, J. L. Aberrant Feeding and Growth in Neonates With Prenatal Opioid Exposure: Evidence of Neuromodulation and Behavioral Changes. Front. Pediatr. 9, 805763 (2021).
Acknowledgements
The authors would like to acknowledge and thank Dr. Nichole Nidey for her advice and support of this study.
Author information
Authors and Affiliations
Contributions
K.M. conceptualized and designed the study, curated data, and drafted the initial manuscript. G.G. performed the formal analysis of the data and critically reviewed the manuscript. M.K. acquired the data and critically reviewed the manuscript. J.M. conceptualized and designed the study, curated data, and critically reviewed the manuscript. All authors approve of the final version of the manuscript and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Institutional review board approval was obtained for this study, CCHMC 2022:1065, and determined that patient consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McNelis, K., Gerdts, G., Khan, M. et al. Early childhood growth following prenatal opioid exposure and Neonatal Opioid Withdrawal Syndrome. Pediatr Res 98, 1395–1402 (2025). https://doi.org/10.1038/s41390-025-04006-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-025-04006-z
This article is cited by
-
Growth patterns in children with prenatal methadone or buprenorphine exposure
Pediatric Research (2025)