Abstract
Background
Congenital nephrotic syndrome (CNS) and infantile nephrotic syndrome (INS) are disorders of podocytes in the slit diaphragm. CNS manifests during the first three months of life, and INS between 3–12 months, with severe proteinuria due to mutations in the NPHS1 and NPHS2 genes. This study aimed to establish specific genotype-phenotype characteristics of CNS and INS in the North American population.
Methods
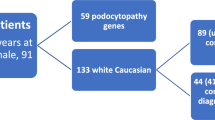
Eleven Pediatric Nephrology Research Consortium (PNRC) sites retrospectively reviewed charts of 36 patients born between 1998–2019 who had CNS or INS and underwent genetic testing. The genetic database confirmed the variant’s pathogenicity.
Results
NPHS1 mutations were more frequently seen in CNS patients, while variant mutations in the WT1 and NPHS2 genes were more common in the INS group. Like c.2335-1 G > A splice mutation, the frequent compound heterozygous mutations of the NPHS1 gene were associated with more severe proteinuria (112.4 ± 135.6 vs. 53.9 ± 57.3). Additionally, NPHS1/WT1 and NPHS1/NPHS2 digenic inheritance featuring biallelic or tri-allelic hits were associated with patient transplantation, regardless of the disease onset.
Conclusion
Identification of compound heterozygous mutations in the NPHS1 gene as an indicator of an aggressive course of CNS in infants. This finding could lead to earlier and targeted interventions of patients, through a precision therapeutic approach
Impact
-
Variations at splice sites, particularly the c.2335-1 G > A mutation, alongside compound heterozygous mutations in the gene NPHS1 and digenic inheritance involving both NPHS1/WT1 or NPHS1/ NPHS2 with a triallelic hit, have been linked to a more severe progression of Congenital Nephrotic Syndrome (CNS) in infants.
-
The presence of a variant involving the digenic inheritance of the NPHS1 gene among children in North America suggests earlier indicators for the severity of the kidney disease.
-
This knowledge can transform the management of Congenital Nephrotic Syndrome in children’s healthcare settings, and lead to the development of early diagnosis biomarkers for the disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The genetic data are available in the ClinVar Database (SCV004123127 - SCV004123153). Apart from this, all other data generated and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Zuo C., Z. J. Congenital Nephrotic Syndrome, https://www.pathologyoutlines.com/topic/kidneycongenitalnephroticsyndrome.html (2023).
Hamasaki, Y. et al. A Cross-Sectional Nationwide Survey of Congenital and Infantile Nephrotic Syndrome in Japan. BMC Nephrol. 21, 363 (2020).
Niaudet, P. Congenital and Infantile Nephrotic Syndrome. Nephrol. Ther. 1, 63–70 (2005).
Bassanese, G. et al. The European Rare Kidney Disease Registry (ERKREG): Objectives, Design and Initial Results. Orphanet J. Rare Dis. 16, 251 (2021).
Bolk, S., Puffenberger, E. G., Hudson, J., Morton, D. H. & Chakravarti, A. Elevated Frequency and Allelic Heterogeneity of Congenital Nephrotic Syndrome, Finnish Type, in the Old Order Mennonites. Am. J. Hum. Genet. 65, 1785–1790 (1999).
Kestila, M. et al. Positionally Cloned Gene for a Novel Glomerular Protein-Nephrin-Is Mutated in Congenital Nephrotic Syndrome. Mol. Cell 1, 575–582 (1998).
Toubiana, J. et al. Therapy-resistant anaemia in congenital nephrotic syndrome of the finnish type-implication of Epo, Transferrin and Transcobalamin losses. Nephrol. Dial. Transpl. 24, 1338–1340 (2009).
Kandasamy, Y., Smith, R., Lumbers, E. R. & Rudd, D. Nephrin - a biomarker of early glomerular injury. Biomark. Res 2, 21 (2014).
Donoviel, D. B. et al. Proteinuria and perinatal lethality in mice lacking Neph1, a novel protein with homology to nephrin. Mol. Cell Biol. 21, 4829–4836 (2001).
Machuca, E. et al. Genotype-phenotype correlations in non-Finnish congenital nephrotic syndrome. J. Am. Soc. Nephrol. 21, 1209–1217 (2010).
Ovunc, B. et al. Mutation analysis of Nphs1 in a worldwide cohort of congenital nephrotic syndrome patients. Nephron. Clin. Pr. 120, c139–c146 (2012).
Schoeb, D. S. et al. Nineteen Novel Nphs1 mutations in a worldwide cohort of patients with congenital nephrotic syndrome (CNS). Nephrol. Dial. Transpl. 25, 2970–2976 (2010).
Heeringa, S. F. et al. Thirteen Novel Nphs1 mutations in a large cohort of children with congenital nephrotic syndrome. Nephrol. Dial. Transpl. 23, 3527–3533 (2008).
Yoshida, S. et al. Endoplasmic Reticulum-Associated Degradation Is Required for Nephrin Maturation and Kidney Glomerular Filtration Function. J. Clin. Invest. 131 (2021).
Fu, R. et al. Novel Nphs1 splice site mutations in a Chinese child with congenital nephrotic syndrome. Genet Mol. Res 14, 433–439 (2015).
Abid, A. et al. Screening of the Lamb2, Wt1, Nphs1, and Nphs2 genes in pediatric nephrotic syndrome. Front Genet 9, 214 (2018).
Koziell, A. et al. Genotype/phenotype correlations of Nphs1 and Nphs2 mutations in nephrotic syndrome advocate a functional inter-relationship in glomerular filtration. Hum. Mol. Genet. 11, 379–388 (2002).
Martin, C. E. & Jones, N. Nephrin signaling in the podocyte: an updated view of signal regulation at the slit diaphragm and beyond. Front Endocrinol. 9, 302 (2018).
Gigante, M., Piemontese, M., Gesualdo, L., Iolascon, A. & Aucella, F. Molecular and genetic basis of inherited nephrotic syndrome. Int J. Nephrol. 2011, 792195 (2011).
Ettou, S. et al. Epigenetic transcriptional reprogramming by Wt1 mediates a repair response during podocyte injury. Sci. Adv. 6, eabb5460 (2020).
Guo, G., Morrison, D. J., Licht, J. D. & Quaggin, S. E. Wt1 activates a glomerular-specific enhancer identified from the human nephrin gene. J. Am. Soc. Nephrol. 15, 2851–2856 (2004).
Jeanpierre, C. et al. Identification of constitutional Wt1 mutations, in patients with isolated diffuse mesangial sclerosis, and analysis of genotype/phenotype correlations by use of a computerized mutation database. Am. J. Hum. Genet 62, 824–833 (1998).
Schumacher, V. et al. Spectrum of early onset nephrotic syndrome associated with Wt1 Missense mutations. Kidney Int. 53, 1594–1600 (1998).
Lee, J. H. et al. Genetic basis of congenital and infantile nephrotic syndromes. Am. J. Kidney Dis. 58, 1042–1043 (2011).
Hinkes, B. G. et al. Nephrotic syndrome in the first year of life: two thirds of cases are caused by mutations in 4 Genes (Nphs1, Nphs2, Wt1, and Lamb2). Pediatrics 119, e907–e919 (2007).
Vazquez Fonseca, L. et al. Mutations in Coq8b (Adck4) found in patients with steroid-resistant nephrotic syndrome alter Coq8b function. Hum. Mutat. 39, 406–414 (2018).
Liu, Y. et al. Clinical diagnosis of genetic disorders at both single-nucleotide and chromosomal levels based on the BGI Seq-500 Platform. Hum. Genome Var. 10, 15 (2023).
Braun, D. A. et al. Mutations in nuclear Pore Genes Nup93, Nup205, and Xpo5 cause steroid-resistant nephrotic syndrome. Nat. Genet. 48, 457–465 (2016).
Li, Y., Tian, C., Wang, Y., Ma, G. & Chen, R. Isolated steroid-resistant nephrotic syndrome in a Chinese child carrying a De Novo mutation in Wt1 Gene: A case report and literature review. BMC Pediatr. 22, 349 (2022).
Boyer, O. et al. Publisher correction: management of congenital nephrotic syndrome: consensus recommendations of the Erknet-Espn Working Group. Nat. Rev. Nephrol. 17, 434 (2021).
Constantinescu, A. R. et al. Clinical presentation and management of nephrotic syndrome in the first year of life: a report from the Pediatric Nephrology Research Consortium. Front Pediatr. 10, 988945 (2022).
UniProt, C. Uniprot: The Universal Protein Knowledgebase in 2023. Nucleic Acids Res. 51, D523–D531 (2023).
Konc, J., Skrlj, B., Erzen, N., Kunej, T. & Janezic, D. Genprobis: web server for mapping of sequence variants to protein binding sites. Nucleic Acids Res. 45, W253–W259 (2017).
Hampel, H. et al. A Practice Guideline from the American College of Medical Genetics and Genomics and the National Society of Genetic Counselors: Referral Indications for Cancer Predisposition Assessment. Genet Med 17, 70–87 (2015).
Genomes Project, C. et al. A global reference for human genetic variation. Nature 526, 68–74 (2015).
Stenson, P. D. et al. The Human Gene Mutation Database: Towards a comprehensive repository of inherited mutation data for medical research, genetic diagnosis and next-generation sequencing studies. Hum. Genet. 136, 665–677 (2017).
Landrum, M. J. et al. Clinvar: public archive of relationships among sequence variation and human phenotype. Nucleic Acids Res. 42, D980–D985 (2014).
Schwarz, J. M., Cooper, D. N., Schuelke, M. & Seelow, D. Mutationtaster2: Mutation prediction for the deep-sequencing age. Nat. Methods 11, 361–362 (2014).
Jaganathan, K. et al. Predicting splicing from primary sequence with deep learning. Cell 176, 535–548 e524 (2019).
Berody, S. et al. Treatment and outcome of congenital nephrotic syndrome. Nephrol. Dial. Transpl. 34, 458–467 (2019).
Sharief, S. N. et al. Genetics of congenital and infantile nephrotic syndrome. World J. Pediatr. 15, 198–203 (2019).
Vachvanichsanong, P., Mitarnun, W., Tungsinmunkong, K. & Dissaneewate, P. Congenital and Infantile Nephrotic Syndrome in Thai Infants. Clin. Pediatr. 44, 169–174 (2005).
Patrakka, J. et al. Congenital Nephrotic Syndrome (Nphs1): Features resulting from different mutations in Finnish Patients. Kidney Int. 58, 972–980 (2000).
Xia, Z. J. et al. A dominant heterozygous mutation in Cog4 causes Saul-Wilson Syndrome, a primordial dwarfism, and disrupts Zebrafish development Via Wnt signaling. Front. Cell Dev. Biol. 9, 720688 (2021).
New, L. A., Keyvani Chahi, A. & Jones, N. Direct regulation of Nephrin Tyrosine phosphorylation by Nck adaptor proteins. J. Biol. Chem. 288, 1500–1510 (2013).
Guaragna, M. S. et al. Nphs2 mutations account for only 15% of nephrotic syndrome cases. BMC Med. Genet. 16, 88 (2015).
Al-Hamed, M. Sayer, J.A., Al-Hassoun, I., Aldahmesh, M.A. & Meyer, B. A novel mutation in Nphs2 causing nephrotic Syndrome in a Saudi Arabian family. NDT Plus 3, 545–548 (2010).
Zlotogora, J. Multiple mutations responsible for frequent genetic diseases in isolated populations. Eur. J. Hum. Genet. 15, 272–278 (2007).
Schaffer, A. A. Digenic inheritance in medical genetics. J. Med. Genet. 50, 641–652 (2013).
Reynolds, B. C. & Oswald, R. J. A. Diagnostic and management challenges in congenital nephrotic syndrome. Pediatr. Health Med. Ther. 10, 157–167 (2019).
Rong, L. et al. Genetic variations and clinical features of Nphs1-related nephrotic syndrome in Chinese Children: A multicenter, retrospective study. Front. Med. 8, 771227 (2021).
Baumgartner-Parzer, S., Witsch-Baumgartner, M. & Hoeppner, W. Emqn best practice guidelines for molecular genetic testing and reporting of 21-Hydroxylase Deficiency. Eur. J. Hum. Genet. 28, 1341–1367 (2020).
Karamyshev, A. L. et al. Inefficient SRP interaction with a nascent chain triggers an mRNA quality control pathway. Cell 156, 146–157 (2014).
Anna, A. & Monika, G. Splicing mutations in human genetic disorders: examples, detection, and confirmation. J. Appl. Genet. 59, 253–268 (2018).
Bullich, G. et al. A kidney-disease gene panel allows a comprehensive genetic diagnosis of cystic and glomerular inherited kidney diseases. Kidney Int. 94, 363–371 (2018).
Acknowledgements
The authors would like to thank the member of the Pediatric Nephrology Research Consortium for approval of this manuscript. The authors also appreciated Dr. Stephanie Stroever for her support of statistical analysis.
Funding
This research was funded by an institutional seed grant from Texas Tech University Health Sciences Center, TX, USA (Grant No. 182169 - 402611 - 20)
Author information
Authors and Affiliations
Contributions
M.I. & T.V.: Conceived the idea and wrote the manuscript; A.C.: Collected and organized the patient’s data; M.N.R., W.S., T.M., A.A., E.P., B.R., L.B., R.M., M.K., S.W. & K.T.: Collected patient data; M.N.R., M.M., M.I. & Y.K.: carried out all data analysis; M.I., Y.K., M.M.; Wrote original draft, T.V., W.S., Y.K., A.R., T.M., S.W. & R.M.: Reviewed and made modifications to the article, T.V.: Supervised and acquired funding. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
All the patients give written consent for this study as per local IRB of each institute.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Islam, M.S., Constantinescu, A.R., Smoyer, W.E. et al. Congenital and infantile nephrotic syndrome: genotype-phenotype associations. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04095-w
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04095-w