Abstract
Background
Neonatal Opioid Withdrawal Syndrome (NOWS) continues to be a major public health burden. Our objective was to assess the efficacy of a stochastic vibro-tactile stimulation (SVS) mattress in reducing initiation of pharmacotherapy in neonates at risk for NOWS.
Methods
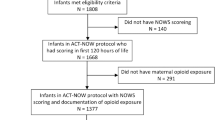
A multicenter, prospective, non-blinded, randomized clinical trial of neonates born ≥ 35 weeks gestation. Neonates randomized to either SVS mattress or standard crib mattress The outcomes examined were initiation of pharmacotherapy, readiness for discharge, NOWS monitoring scores, cry quality and mattress acceptability surveys.
Results
Of 62 infants enrolled, 4 infants (10.0%) in the SVS group and 4 infants (18.2%) in the standard group were initiated on pharmacotherapy. Infants in SVS group demonstrated early readiness for discharge, with no differences between the two groups for NOWS scoring or cry quality. Overall, 60% of nurses and 80% of parents found the SVS mattress helped calm the neonate.
Conclusion
Although the SVS mattress demonstrated a trend towards lower initiation of pharmacotherapy and earlier readiness for discharge, the results were not statistically significant due to fewer neonates being enrolled than expected. The mattress was highly acceptable to parents and nurses.
Clinical trial
Registered at ClinicalTrials.gov ID # NCT04834297; https://clinicaltrials.gov/study/NCT04834297
Impact
-
Improving on current non-pharmacologic interventions for the prevention and treatment of Neonatal Opioid Withdrawal Syndrome (NOWS) is critically important.
-
Our study focused on assessing the efficacy of a stochastic vibro-tactile stimulation (SVS) mattress in reducing the use of pharmacotherapy in neonates at risk for NOWS within the first 5 days after birth.
-
In neonates at risk for NOWS, the SVS mattress may reduce the need for pharmacotherapy and improve readiness for discharge while being acceptable to parents and nurses.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The de-identified dataset used for this study will be available from the corresponding author on reasonable request.
References
NIDA. Drug Overdose Deaths: Facts and Figures. Retrieved from https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates (2024). (Accessed May 16th 2025).
Keyes, K. M. et al. What is the prevalence of and trend in opioid use disorder in the United States from 2010 to 2019? Using multiplier approaches to estimate prevalence for an unknown population size. Drug Alcohol Depend. Rep. 3, 100052 (2022).
Hirai, A. H., Ko, J. Y., Owens, P. L., Stocks, C. & Patrick, S. W. Neonatal abstinence syndrome and maternal opioid-related diagnoses in the US, 2010-2017. JAMA 325, 146–155 (2021).
Patrick, S. W., Barfield, W. D., Poindexter, B. & Committee on Fetus and Newborn, Committee on Substance Use and Prevention Neonatal opioid withdrawal syndrome. Pediatrics 146, e2020029074 (2020).
Strahan, A. E., Guy, G. P., Bohm, M., Frey, M. & Ko, J. Y. Neonatal abstinence syndrome incidence and health care costs in the United States, 2016. JAMA Pediatr. 174, 200–202 (2020).
Singh, R. et al. Partnering with parents to improve outcomes for substance exposed newborns-a pilot program. J. Perinatol. 40, 1041–1049 (2020).
Singh, R. et al. Short term outcomes of neonatal opioid withdrawal syndrome (NOWS) – a comparison of two approaches. PNQIN Collaborative of Massachusetts. J. Perinatol. 44, 1137–1145 (2024).
Singh, R. et al. for PNQIN Collaborative of Massachusetts. Predictors of pharmacologic therapy for neonatal opioid withdrawal syndrome: a retrospective analysis of a statewide database. J. Perinatol. 41, 1381–1388 (2021).
Young, L. W. et al. ACT NOW Collaborative. Eat, sleep, console approach or usual care for neonatal opioid withdrawal. N. Engl. J. Med. 388, 2326–2337 (2023).
Zuzarte, I. et al. Vibrotactile stimulation: A non-pharmacological intervention for opioid-exposed newborns. PLoS One 12, e0175981 (2017).
Bloch-Salisbury, E. et al. Efficacy of a vibrating crib mattress to reduce pharmacologic treatment in opioid-exposed newborns: a randomized clinical trial. JAMA Pediatr. 177, 665–674 (2023).
DʼApolito, K. C. Assessing neonates for neonatal abstinence: are you reliable?. J. Perinat. Neonatal Nurs. 28, 220–231 (2014).
Wachman, E. M. et al. A quality improvement initiative to implement the eat, sleep, console neonatal opioid withdrawal syndrome care tool in Massachusetts’ PNQIN collaborative. J. Perinatol. 40, 1560–1569 (2020).
Newcombe, R. G. Interval estimation for the difference between independent proportions: comparison of eleven methods. Stat. Med. 17, 873–890 (1998). Erratum in: Stat Med. 18, 1293 (1999).
Bender, R., Kuss, O., Hildebrandt, M. & Gehrmann, U. Estimating adjusted NNT measures in logistic regression analysis. Stat. Med 26, 5586–5595 (2007).
Gehrmann, U., Kuss, O., Wellmann, J. & Bender, R. Logistic regression was preferred to estimate risk differences and numbers needed to be exposed adjusted for covariates. J. Clin. Epidemiol. 63, 1223–1231 (2010).
Hahn, P. D., Graham, D. A., Ozonoff, A. & Milliren, C. E. Neonatal opioid withdrawal syndrome treatment guidelines and birth hospital utilization. Pediatrics 154, e2023063635 (2024).
Nagaraj, U. D. et al. MRI findings in third-trimester opioid-exposed fetuses, with focus on brain measurements: a prospective multicenter case-control study. AJR Am. J. Roentgenol. 220, 418–427 (2023).
Merhar, S. L. et al. White matter injury and structural anomalies in infants with prenatal opioid exposure. AJNR Am. J. Neuroradiol. 40, 2161–2165 (2019).
Yen, E. et al. Sex-specific inflammatory and white matter effects of prenatal opioid exposure: a pilot study. Pediatr. Res 93, 604–611 (2023).
Gowen, A. M. et al. In utero and post-natal opioid exposure followed by mild traumatic brain injury contributes to cortical neuroinflammation, mitochondrial dysfunction, and behavioral deficits in juvenile rats. Brain Behav. Immun. Health 32, 100669 (2023).
Mahabee-Gittens, E. M. et al. Prenatal opioid exposure and risk for adverse brain and motor outcomes in infants born premature. J. Pediatr. 267, 113908 (2024).
Bann, C. M. et al. Correction To: Outcomes of Babies with Opioid Exposure (OBOE): protocol of a prospective longitudinal cohort study. Pediatr. Res. 94, 1581 (2023).
Jenkins, C., Hudnall, M., Hanson, C., Lewis, D. & Parton, J. M. Cost of care for newborns with neonatal abstinence syndrome in a state medicaid program. JAMA Netw. Open 7, e240295 (2024).
Sweigart, E. Compassion fatigue, burnout, and neonatal abstinence syndrome. Neonatal Netw. 36, 7–11 (2017).
Shannon, J., Blythe, S. & Peters, K. The complexities associated with caring for hospitalised infants with neonatal abstinence syndrome: the perspectives of nurses and midwives. Child. (Basel) 8, 152 (2021).
Acknowledgements
The authors wish to thank the medical, nursing, and program staff; and the children and families participating in this trial. The authors thank the Data and Safety Monitoring Board (Dr. Vincent Smith, Dr. Elizabeth Yen, and Mr. Benjamin Sweigart). The authors also specifically want to acknowledge the contributions of Mr. John Konsin and Mr. David Morrill of Prapela Inc., for the technological support in manufacturing the study mattresses to specifications of the study protocol.
Funding
National Institutes of Health Small Business Innovation Research Program (SBIR) Grant, Award Number 2 R44 DA049300-02 (Singh, Konsin). The research was also supported by the National Center for Advancing Translational Sciences, National Institutes of Health, Award Number UM1TR004398.
Author information
Authors and Affiliations
Contributions
RS and JD drafted the original manuscript and conceived and designed the study, contributed to data acquisition and analysis, and drafted the final manuscript. LT and BK contributed to data analysis; critically reviewed and revised the manuscript for intellectual content. MC, LR, SB, JF and AA contributed to data acquisition and analysis; critically reviewed and revised the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Written informed consent was obtained from parents prior to any study related intervention or completion of survey by the caregivers (nurses, parents).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singh, R., Trinquart, L., Koethe, B. et al. Efficacy of stochastic vibro-tactile stimulation for newborns at risk of neonatal opioid withdrawal syndrome. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04162-2
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04162-2