Abstract
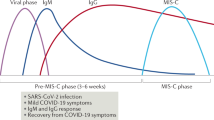
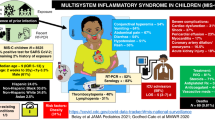
Neutrophils, specialized cells of the early innate immune response, are important for maintaining the body’s internal homeostasis. Upon invasion by foreign microbes, neutrophils are swiftly activated and recruited to the infection site, where they perform bactericidal functions through phagocytic clearance, degranulation-mediated toxin release, and NADPH oxidase-dependent killing. While their presence is crucial in the early stages of inflammation to combat infection, the prolonged engagement of neutrophils at the infection site can cause tissue damage due to apoptosis and the release of cytotoxic mediators. Neutrophils exhibit significant heterogeneity in response to allostatic conditions, with their phenotypic and functional properties undergoing distinct changes. Therefore, understanding the heterogeneity and diversity of neutrophils under physiological and pathological conditions is important. Multisystem inflammatory syndrome in children (MIS-C) is a pediatric inflammatory syndrome that emerges following exposure to SARS-CoV-2, while Kawasaki disease (KD) is a childhood systemic vasculitis with unknown etiology. Both conditions share clinical features, including neutrophilia and cardiovascular complications. This suggests the likelihood of overlapping underlying immunopathogenic mechanisms, and neutrophils may play a crucial role in these processes. This review focuses on the heterogeneity and function of neutrophils in KD and MIS-C, providing a comprehensive overview of the current research in this field.
Impact
-
Neutrophils exhibit significant heterogeneity under physiological and pathological states. Different neutrophil subsets perform diverse functional characteristics.
-
KD and MIS-C have apparent phenotypic similarities of systemic inflammation and cardiovascular complications. Neutrophil heterogeneity correlates with disease severity, and studies of neutrophil subsets reveal potential shared immunological drivers.
-
Multi-omics analysis of neutrophil heterogeneity helps to better understand neutrophil subsets and discover new functions. Research into MIS-C and KD enhances our understanding of pediatric inflammatory diseases with cardiovascular involvement.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Mestas, J. & Hughes, C. C. Of mice and not men: differences between mouse and human immunology. J. Immunol. 172, 2731–2738 (2004).
Lahoz-Beneytez, J. et al. Human neutrophil kinetics: modeling of stable isotope labeling data supports short blood neutrophil half-lives. Blood 127, 3431–3438 (2016).
Burn, G. L., Foti, A., Marsman, G., Patel, D. F. & Zychlinsky, A. The Neutrophil. Immunity 54, 1377–1391 (2021).
Tak, T., Tesselaar, K., Pillay, J., Borghans, J. A. & Koenderman, L. What’s your age again? Determination of human neutrophil half-lives revisited. J. Leukoc. Biol. 94, 595–601 (2013).
Nourshargh, S., Renshaw, S. A. & Imhof, B. A. Reverse migration of neutrophils: Where, when, how, and why?. Trends Immunol. 37, 273–286 (2016).
Wang, L., Luqmani, R. & Udalova, I. A. The role of neutrophils in rheumatic disease-associated vascular inflammation. Nat. Rev. Rheumatol. 18, 158–170 (2022).
Feldstein, L. R. et al. Multisystem inflammatory syndrome in U.S. children and adolescents. N. Engl. J. Med. 383, 334–346 (2020).
Feldstein, L. R. et al. Characteristics and outcomes of US children and adolescents with multisystem inflammatory syndrome in children (MIS-C) compared with severe acute COVID-19. JAMA 325, 1074–1087 (2021).
Yilmaz, D. et al. Evaluation of 601 children with multisystem inflammatory syndrome (Turk MISC study). Eur. J. Pediatr. 182, 5531–5542 (2023).
Henderson, L. A. et al. American College of Rheumatology Clinical Guidance for multisystem inflammatory syndrome in children associated with SARS-CoV-2 and hyperinflammation in pediatric COVID-19: version 2. Arthritis Rheumatol.73, e13–e29 (2021).
Isaza-Correa, J. et al. Innate immune dysregulation in multisystem inflammatory syndrome in children (MIS-C). Sci. Rep. 13, 16463 (2023).
Farias, J. S. et al. The use of neutrophil-lymphocyte ratio for the prediction of refractory disease and coronary artery lesions in patients with Kawasaki disease. Cardiol. Young 33, 1409–1417 (2023).
Takahashi, K., Oharaseki, T. & Yokouchi, Y. Histopathological aspects of cardiovascular lesions in Kawasaki disease. Int. J. Rheum. Dis. 21, 31–35 (2018).
Henning, A. N., Roychoudhuri, R. & Restifo, N. P. Epigenetic control of CD8(+) T cell differentiation. Nat. Rev. Immunol. 18, 340–356 (2018).
Ruterbusch, M., Pruner, K. B., Shehata, L. & Pepper, M. In vivo CD4(+) T cell differentiation and function: revisiting the Th1/Th2 paradigm. Annu. Rev. Immunol. 38, 705–725 (2020).
Yvan-Charvet, L. & Ng, L. G. Granulopoiesis and neutrophil homeostasis: a metabolic, daily balancing act. Trends Immunol. 40, 598–612 (2019).
Paudel, S., Ghimire, L., Jin, L., Jeansonne, D. & Jeyaseelan, S. Regulation of emergency granulopoiesis during infection. Front. Immunol. 13, 961601 (2022).
Muench, D. E. et al. Mouse models of neutropenia reveal progenitor-stage-specific defects. Nature 582, 109–114 (2020).
Xie, X. et al. Single-cell transcriptome profiling reveals neutrophil heterogeneity in homeostasis and infection. Nat. Immunol. 21, 1119–1133 (2020).
Kwok, I. et al. Combinatorial single-cell analyses of granulocyte-monocyte progenitor heterogeneity reveals an early uni-potent neutrophil progenitor. Immunity 53, 303–318.e5 (2020).
Dinh, H. Q. et al. Coexpression of CD71 and CD117 identifies an early unipotent neutrophil progenitor population in human bone marrow. Immunity 53, 319–334.e6 (2020).
Zhu, Y. P. et al. Identification of an early unipotent neutrophil progenitor with pro-tumoral activity in mouse and human bone marrow. Cell Rep. 24, 2329–2341.e8 (2018).
Evrard, M. et al. Developmental analysis of bone marrow neutrophils reveals populations specialized in expansion, trafficking, and effector functions. Immunity 48, 364–379.e8 (2018).
Kim, M. H. et al. A late-lineage murine neutrophil precursor population exhibits dynamic changes during demand-adapted granulopoiesis. Sci. Rep. 7, 39804 (2017).
Rosales, C. Neutrophil: a cell with many roles in inflammation or several cell types?. Front. Physiol. 9, 113 (2018).
Adrover, J. M., Nicolás-Ávila, J. A. & Hidalgo, A. Aging: a temporal dimension for neutrophils. Trends Immunol. 37, 334–345 (2016).
Lawrence, S. M., Corriden, R. & Nizet, V. How neutrophils meet their end. Trends Immunol. 41, 531–544 (2020).
Uhl, B. et al. Aged neutrophils contribute to the first line of defense in the acute inflammatory response. Blood 128, 2327–2337 (2016).
Adrover, J. M. et al. A neutrophil timer coordinates immune defense and vascular protection. Immunity 50, 390–402.e310 (2019).
Gabrilovich, D. I. Myeloid-derived suppressor cells. Cancer Immunol. Res. 5, 3–8 (2017).
Schrijver, I. T., Théroude, C. & Roger, T. Myeloid-derived suppressor cells in sepsis. Front. Immunol. 10, 327 (2019).
Hassani, M. et al. On the origin of low-density neutrophils. J. Leukoc. Biol. 107, 809–818 (2020).
Bowers, N. L. et al. Immune suppression by neutrophils in HIV-1 infection: role of PD-L1/PD-1 pathway. PLoS Pathog. 10, e1003993 (2014).
Silvestre-Roig, C., Fridlender, Z. G., Glogauer, M. & Scapini, P. Neutrophil diversity in health and disease. Trends Immunol. 40, 565–583 (2019).
Ramirez-Velazquez, C., Castillo, E. C., Guido-Bayardo, L. & Ortiz-Navarrete, V. IL-17-producing peripheral blood CD177+ neutrophils increase in allergic asthmatic subjects. Allergy Asthma Clin. Immunol. 9, 23 (2013).
Clemmensen, S. N. et al. Olfactomedin 4 defines a subset of human neutrophils. J. Leukoc. Biol. 91, 495–500 (2012).
Alder, M. N., Opoka, A. M., Lahni, P., Hildeman, D. A. & Wong, H. R. Olfactomedin-4 is a candidate marker for a pathogenic neutrophil subset in septic shock. Crit. Care Med 45, e426–e432 (2017).
Zhou, G. et al. CD177(+) neutrophils as functionally activated neutrophils negatively regulate IBD. Gut 67, 1052–1063 (2018).
Zhang, R. et al. CD177(+) cells produce neutrophil extracellular traps that promote biliary atresia. J. Hepatol. 77, 1299–1310 (2022).
Zhang, R., Huang, J., Shan, J., Chen, Y. & Xia, H. Peripheral blood CD177(+) cells as an early diagnostic marker for biliary atresia: a prospective multicentre study in pediatric patients with cholestasis. J. Hepatol. 77, 1714–1716 (2022).
Massena, S. et al. Identification and characterization of VEGF-A-responsive neutrophils expressing CD49d, VEGFR1, and CXCR4 in mice and humans. Blood 126, 2016–2026 (2015).
Wigerblad, G. et al. Single-cell analysis reveals the range of transcriptional states of circulating human neutrophils. J. Immunol. 209, 772–782 (2022).
Becher, B. et al. High-dimensional analysis of the murine myeloid cell system. Nat. Immunol. 15, 1181–1189 (2014).
Ballesteros, I. et al. Co-option of neutrophil fates by tissue environments. Cell 183, 1282–1297.e18 (2020).
Deniset, J. F., Surewaard, B. G., Lee, W. Y. & Kubes, P. Splenic Ly6G(high) mature and Ly6G(int) immature neutrophils contribute to eradication of S. pneumoniae. J. Exp. Med. 214, 1333–1350 (2017).
Wang, K. et al. Locally organised and activated Fth1(hi) neutrophils aggravate inflammation of acute lung injury in an IL-10-dependent manner. Nat. Commun. 13, 7703 (2022).
Cui, A. et al. Single-cell atlas of the liver myeloid compartment before and after cure of chronic viral hepatitis. J. Hepatol. 80, 251–267 (2024).
Calcagno, D. M. et al. SiglecF(HI) marks late-stage neutrophils of the infarcted heart: a single-cell transcriptomic analysis of neutrophil diversification. J. Am. Heart Assoc. 10, e019019 (2021).
Vafadarnejad, E. et al. Dynamics of cardiac neutrophil diversity in murine myocardial infarction. Circ. Res. 127, e232–e249 (2020).
Sreejit, G. et al. Retention of the NLRP3 inflammasome-primed neutrophils in the bone marrow is essential for myocardial infarction-induced granulopoiesis. Circulation 145, 31–44 (2022).
Sreejit, G. et al. Neutrophil-derived S100A8/A9 amplify granulopoiesis after myocardial infarction. Circulation 141, 1080–1094 (2020).
Salcher, S. et al. High-resolution single-cell atlas reveals diversity and plasticity of tissue-resident neutrophils in non-small cell lung cancer. Cancer Cell 40, 1503–1520.e8 (2022).
Ng, M. S. F. et al. Deterministic reprogramming of neutrophils within tumors. Science 383, eadf6493 (2024).
Liew, P. X. & Kubes, P. The neutrophil’s role during health and disease. Physiol. Rev. 99, 1223–1248 (2019).
Dale, D. C., Boxer, L. & Liles, W. C. The phagocytes: neutrophils and monocytes. Blood 112, 935–945 (2008).
Segal, A. W. How neutrophils kill microbes. Annu. Rev. Immunol. 23, 197–223 (2005).
Kruger, P. et al. Neutrophils: between host defence, immune modulation, and tissue injury. PLoS Pathog. 11, e1004651 (2015).
Li, P. et al. PAD4 is essential for antibacterial innate immunity mediated by neutrophil extracellular traps. J. Exp. Med. 207, 1853–1862 (2010).
Schauer, C. et al. Aggregated neutrophil extracellular traps limit inflammation by degrading cytokines and chemokines. Nat. Med. 20, 511–517 (2014).
Leppkes, M. et al. Neutrophils prevent rectal bleeding in ulcerative colitis by peptidyl-arginine deiminase-4-dependent immunothrombosis. Gut 71, 2414–2429 (2022).
Leppkes, M. et al. Vascular occlusion by neutrophil extracellular traps in COVID-19. EBioMedicine 58, 102925 (2020).
Liu, J. et al. Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J. Transl. Med. 18, 206 (2020).
Guan, J. et al. Continuous tracking of COVID-19 patients’ immune status. Int. Immunopharmacol. 89, 107034 (2020).
Pouletty, M. et al. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 mimicking Kawasaki disease (Kawa-COVID-19): a multicentre cohort. Ann. Rheum. Dis. 79, 999–1006 (2020).
Porritt, R. A. et al. The autoimmune signature of hyperinflammatory multisystem inflammatory syndrome in children. J. Clin. Investig. 131, https://doi.org/10.1172/jci151520 (2021).
Meizlish, M. L. et al. A neutrophil activation signature predicts critical illness and mortality in COVID-19. Blood Adv. 5, 1164–1177 (2021).
Gruber, C. N. et al. Mapping systemic inflammation and antibody responses in multisystem inflammatory syndrome in children (MIS-C). Cell 186, 3325 (2023).
Aschenbrenner, A. C. et al. Disease severity-specific neutrophil signatures in blood transcriptomes stratify COVID-19 patients. Genome Med. 13, 7 (2021).
Hemmat, N. et al. Neutrophils, crucial, or harmful immune cells involved in coronavirus infection: a bioinformatics study. Front. Genet. 11, 641 (2020).
McElvaney, O. J. et al. Characterization of the inflammatory response to severe COVID-19 illness. Am. J. Respir. Crit. Care Med. 202, 812–821 (2020).
Sengupta, S., Caldwell, C. C. & Nomellini, V. Distinct neutrophil populations in the spleen during PICS. Front. Immunol. 11, 804 (2020).
Belchamber, K. B. R. et al. Dysregulated neutrophil phenotype and function in hospitalised non-ICU COVID-19 pneumonia. Cells 11, https://doi.org/10.3390/cells11182901 (2022).
Karawajczyk, M. et al. High expression of neutrophil and monocyte CD64 with simultaneous lack of upregulation of adhesion receptors CD11b, CD162, CD15, CD65 on neutrophils in severe COVID-19. Ther. Adv. Infect. Dis. 8, 20499361211034065 (2021).
Carter, M. J. et al. Peripheral immunophenotypes in children with multisystem inflammatory syndrome associated with SARS-CoV-2 infection. Nat. Med. 26, 1701–1707 (2020).
van der Poel, C. E., Spaapen, R. M., van de Winkel, J. G. & Leusen, J. H. Functional characteristics of the high affinity IgG receptor, FcγRI. J. Immunol. 186, 2699–2704 (2011).
Boribong, B. P. et al. Neutrophil profiles of pediatric COVID-19 and multisystem inflammatory syndrome in children. Cell Rep. Med. 3, 100848 (2022).
Ramaswamy, A. et al. Immune dysregulation and autoreactivity correlate with disease severity in SARS-CoV-2-associated multisystem inflammatory syndrome in children. Immunity 54, 1083–1095.e7 (2021).
Wang, W. T. et al. Inflammasome activation in children with Kawasaki disease and multisystem inflammatory syndrome. Arterioscler Thromb. Vasc. Biol. 41, 2509–2511 (2021).
Silva, C. M. S. et al. Gasdermin-D activation by SARS-CoV-2 triggers NET and mediate COVID-19 immunopathology. Crit. Care 26, 206 (2022).
Al-Kuraishy, H. M. et al. Neutrophil Extracellular Traps (NETs) and Covid-19: a new frontiers for therapeutic modality. Int. Immunopharmacol. 104, 108516 (2022).
Sinha, S. et al. Dexamethasone modulates immature neutrophils and interferon programming in severe COVID-19. Nat. Med. 28, 201–211 (2022).
Combes, A. J. et al. Global absence and targeting of protective immune states in severe COVID-19. Nature 591, 124–130 (2021).
Park, A. & Iwasaki, A. Type I and type III interferons—induction, signaling, evasion, and application to combat COVID-19. Cell Host Microbe 27, 870–878 (2020).
LaSalle, T. J. et al. Longitudinal characterization of circulating neutrophils uncovers phenotypes associated with severity in hospitalized COVID-19 patients. Cell Rep. Med. 3, 100779 (2022).
Carissimo, G. et al. Whole blood immunophenotyping uncovers immature neutrophil-to-VD2 T-cell ratio as an early marker for severe COVID-19. Nat. Commun. 11, 5243 (2020).
Schulte-Schrepping, J. et al. Severe COVID-19 is marked by a dysregulated myeloid cell compartment. Cell 182, 1419–1440.e23 (2020).
Silvin, A. et al. Elevated calprotectin and abnormal myeloid cell subsets discriminate severe from mild COVID-19. Cell 182, 1401–1418.e18 (2020).
Karagol, C. et al. Delta neutrophil index and C-reactive protein: a potential diagnostic marker of multisystem inflammatory syndrome in children (MIS-C) with COVID-19. Eur. J. Pediatr. 181, 775–781 (2022).
Kawasaki, T., Kosaki, F., Okawa, S., Shigematsu, I. & Yanagawa, H. A new infantile acute febrile mucocutaneous lymph node syndrome (MLNS) prevailing in Japan. Pediatrics 54, 271–276 (1974).
McCrindle, B. W. et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation 135, e927–e999 (2017).
Watts, R. A., Hatemi, G., Burns, J. C. & Mohammad, A. J. Global epidemiology of vasculitis. Nat. Rev. Rheumatol. 18, 22–34 (2022).
Ae, R. et al. Epidemiology, treatments, and cardiac complications in patients with kawasaki disease: the nationwide survey in Japan, 2017-2018. J. Pediatr. 225, 23–29.e2 (2020).
Burns, J. C., Capparelli, E. V., Brown, J. A., Newburger, J. W. & Glode, M. P. Intravenous gamma-globulin treatment and retreatment in Kawasaki disease. US/Canadian Kawasaki Syndrome Study Group. Pediatr. Infect. Dis. J. 17, 1144–1148 (1998).
Daniels, L. B. et al. Prevalence of Kawasaki disease in young adults with suspected myocardial ischemia. Circulation 125, 2447–2453 (2012).
Kato, H. et al. Long-term consequences of Kawasaki disease. A 10- to 21-year follow-up study of 594 patients. Circulation 94, 1379–1385 (1996).
Friedman, K. G. et al. Coronary artery aneurysms in Kawasaki disease: risk factors for progressive disease and adverse cardiac events in the US population. J. Am. Heart Assoc. 5, https://doi.org/10.1161/jaha.116.003289 (2016).
Moffett, B. S., Syblik, D., Denfield, S., Altman, C. & Tejtel-Sexson, K. Epidemiology of immunoglobulin resistant Kawasaki disease: results from a large, national database. Pediatr. Cardiol. 36, 374–378 (2015).
Skochko, S. M. et al. Kawasaki disease outcomes and response to therapy in a multiethnic community: a 10-year experience. J. Pediatr. 203, 408–415.e3 (2018).
Andreozzi, L., Bracci, B., D’Errico, F. & Rigante, D. A master role for neutrophils in Kawasaki syndrome. Immunol. Lett. 184, 112–114 (2017).
Orenstein, J. M. et al. Three linked vasculopathic processes characterize Kawasaki disease: a light and transmission electron microscopic study. PLoS ONE 7, e38998 (2012).
Wu, S. et al. Prediction of intravenous immunoglobulin resistance in Kawasaki disease in children. World J. Pediatr. 16, 607–613 (2020).
Tang, Y. et al. Prediction of intravenous immunoglobulin resistance in Kawasaki disease in an East China population. Clin. Rheumatol. 35, 2771–2776 (2016).
Lao, S., Zhou, T., Kuo, H. C., Zhong, G. & Zeng, W. Risk factors for coronary artery lesions in Kawasaki disease independent of antibiotic use in Chinese children. Front. Public Health 10, 817613 (2022).
Lee, H. Y. & Song, M. S. Predictive factors of resistance to intravenous immunoglobulin and coronary artery lesions in Kawasaki disease. Korean J. Pediatr. 59, 477–482 (2016).
Ha, K. S. et al. Value of neutrophil-lymphocyte ratio in predicting outcomes in Kawasaki disease. Am. J. Cardiol. 116, 301–306 (2015).
Chang, L. S. et al. Neutrophil-to-lymphocyte ratio and scoring system for predicting coronary artery lesions of Kawasaki disease. BMC Pediatr. 20, 398 (2020).
Cho, H. J. et al. High neutrophil : lymphocyte ratio is associated with refractory Kawasaki disease. Pediatr. Int. 59, 669–674 (2017).
Brodeur, K. E. et al. Elevation of IL-17 cytokines distinguishes Kawasaki disease from other pediatric inflammatory disorders. Arthritis Rheumatol. https://doi.org/10.1002/art.42680 (2023).
Hui-Yuen, J. S., Duong, T. T. & Yeung, R. S. TNF-alpha is necessary for induction of coronary artery inflammation and aneurysm formation in an animal model of Kawasaki disease. J. Immunol. 176, 6294–6301 (2006).
Netea, S. A. et al. Transient anti-cytokine autoantibodies superimpose the hyperinflammatory response in Kawasaki disease and multisystem inflammatory syndrome in children: a comparative cohort study on correlates of disease. EBioMedicine 95, 104736 (2023).
Lord, B. I. et al. Myeloid cell kinetics in mice treated with recombinant interleukin-3, granulocyte colony-stimulating factor (CSF), or granulocyte-macrophage CSF in vivo. Blood 77, 2154–2159 (1991).
Lieschke, G. J. et al. Mice lacking granulocyte colony-stimulating factor have chronic neutropenia, granulocyte and macrophage progenitor cell deficiency, and impaired neutrophil mobilization. Blood 84, 1737–1746 (1994).
Suzuki, H. et al. Serum levels of neutrophil activation cytokines in Kawasaki disease. Pediatr. Int. 43, 115–119 (2001).
Tsujimoto, H. et al. Delayed apoptosis of circulating neutrophils in Kawasaki disease. Clin. Exp. Immunol. 126, 355–364 (2001).
Stock, A. T., Hansen, J. A., Sleeman, M. A., McKenzie, B. S. & Wicks, I. P. GM-CSF primes cardiac inflammation in a mouse model of Kawasaki disease. J. Exp. Med. 213, 1983–1998 (2016).
Harada, M. et al. Histopathological characteristics of myocarditis in acute-phase Kawasaki disease. Histopathology 61, 1156–1167 (2012).
Takahashi, K., Oharaseki, T., Naoe, S., Wakayama, M. & Yokouchi, Y. Neutrophilic involvement in the damage to coronary arteries in acute stage of Kawasaki disease. Pediatr. Int. 47, 305–310 (2005).
Zhu, Y. P. et al. Immune response to intravenous immunoglobulin in patients with Kawasaki disease and MIS-C. J. Clin. Investig. 131, https://doi.org/10.1172/jci147076 (2021).
Hu, J., Qian, W., Wang, T., Ling, J. & Shi, Y. Neutrophil extracellular traps formation and citrullinated histones 3 levels in patients with Kawasaki disease. Iran. J. Immunol. 3, 327–334 (2023).
Carmona-Rivera, C. Multicenter analysis of neutrophil extracellular trap dysregulation in adult and pediatric COVID-19. JCI Insight. 7, e160332 (2022).
Yamashita, K., Takaori-Kondo, A. & Mizugishi, K. Exaggerated neutrophil extracellular trap formation in Kawasaki disease: a key phenomenon behind the outbreak in western countries? Ann. Rheum. Dis. https://doi.org/10.1136/annrheumdis-2020-218593 (2020).
Jing, Y. et al. Neutrophil extracellular trap from Kawasaki disease alter the biologic responses of PBMC. Biosci. Rep. 40, https://doi.org/10.1042/bsr20200928 (2020).
Yoshida, Y. et al. Enhanced formation of neutrophil extracellular traps in Kawasaki disease. Pediatr. Res. 87, 998–1004 (2020).
Wang, H. et al. Subgroups of children with Kawasaki disease: a data-driven cluster analysis. Lancet Child Adolesc. Health 7, 697–707 (2023).
Lee, S. H. et al. Delta-neutrophil index: a potential predictor of coronary artery involvement in Kawasaki disease by retrospective analysis. Rheumatol. Int. 39, 1955–1960 (2019).
Abe, J. et al. Elevated granulocyte colony-stimulating factor levels predict treatment failure in patients with Kawasaki disease. J. Allergy Clin. Immunol. 122, 1008–1013.e8 (2008).
Ogata, S. et al. Clinical score and transcript abundance patterns identify Kawasaki disease patients who may benefit from addition of methylprednisolone. Pediatr. Res. 66, 577–584 (2009).
Ko, T. M. et al. Genome-wide transcriptome analysis to further understand neutrophil activation and lncRNA transcript profiles in Kawasaki disease. Sci. Rep. 9, 328 (2019).
Beltran, J. V. B., Lin, F. P., Chang, C. L. & Ko, T. M. Single-cell meta-analysis of neutrophil activation in Kawasaki disease and multisystem inflammatory syndrome in children reveals potential shared immunological drivers. Circulation 148, 1778–1796 (2023).
Bai, M. et al. CD177 modulates human neutrophil migration through activation-mediated integrin and chemoreceptor regulation. Blood 130, 2092–2100 (2017).
Chen, K. D. et al. Comparable bidirectional neutrophil immune dysregulation between Kawasaki disease and severe COVID-19. Front. Immunol. 13, 995886 (2022).
Wakita, D. et al. Role of interleukin-1 signaling in a mouse model of Kawasaki disease-associated abdominal aortic aneurysm. Arterioscler. Thromb. Vasc. Biol. 36, 886–897 (2016).
Meher, A. K. et al. Novel role of IL (Interleukin)-1β in neutrophil extracellular trap formation and abdominal aortic aneurysms. Arterioscler. Thromb. Vasc. Biol. 38, 843–853 (2018).
Gruber, C. N. et al. Mapping systemic inflammation and antibody responses in multisystem inflammatory syndrome in children (MIS-C). Cell 183, 982–995.e14 (2020).
Hoang, L. T. et al. Global gene expression profiling identifies new therapeutic targets in acute Kawasaki disease. Genome Med. 6 541 (2014).
Huet, T. et al. Anakinra for severe forms of COVID-19: a cohort study. Lancet Rheumatol. 2, e393–e400 (2020).
Tremoulet, A. H. et al. Rationale and study design for a phase I/IIa trial of anakinra in children with Kawasaki disease and early coronary artery abnormalities (the ANAKID trial). Contemp. Clin. Trials 48, 70–75 (2016).
Veras, F. P. et al. SARS-CoV-2-triggered neutrophil extracellular traps mediate COVID-19 pathology. J. Exp. Med. 217, https://doi.org/10.1084/jem.20201129 (2020).
Radermecker, C. et al. Neutrophil extracellular traps infiltrate the lung airway, interstitial, and vascular compartments in severe COVID-19. J. Exp. Med. 217, https://doi.org/10.1084/jem.20201012 (2020).
Martinod, K. et al. Neutrophil histone modification by peptidylarginine deiminase 4 is critical for deep vein thrombosis in mice. Proc. Natl. Acad. Sci. USA 110, 8674–8679 (2013).
Fuchs, T. A. et al. Extracellular DNA traps promote thrombosis. Proc. Natl. Acad. Sci. USA 107, 15880–15885 (2010).
Burmeister, A. et al. Impact of neutrophil extracellular traps on fluid properties, blood flow and complement activation. Front. Immunol. 13, 1078891 (2022).
Zuo, Y. et al. Neutrophil extracellular traps in COVID-19. JCI Insight 5, https://doi.org/10.1172/jci.insight.138999 (2020).
Noval Rivas, M. et al. Intestinal permeability and IgA provoke immune vasculitis linked to cardiovascular inflammation. Immunity 51, 508–521.e6 (2019).
Yonker, L. M. et al. Multisystem inflammatory syndrome in children is driven by zonulin-dependent loss of gut mucosal barrier. J. Clin. Investig. 131, https://doi.org/10.1172/jci149633 (2021).
Menikou, S., Langford, P. R. & Levin, M. Kawasaki disease: the role of immune complexes revisited. Front. Immunol. 10, 1156 (2019).
Philip, S., Jindal, A. & Krishna Kumar, R. An update on understanding the pathophysiology in Kawasaki disease: possible role of immune complexes in coronary artery lesion revisited. Int. J. Rheum. Dis. 26, 1453–1463 (2023).
Ricke, D. O. & Smith, N. VAERS vasculitis adverse events retrospective study: etiology model of immune complexes activating Fc receptors in kawasaki disease and multisystem inflammatory syndromes. Life 14, https://doi.org/10.3390/life14030353 (2024).
Sun, S. et al. Neutrophil extracellular traps impair intestinal barrier functions in sepsis by regulating TLR9-mediated endoplasmic reticulum stress pathway. Cell Death Dis. 12, 606 (2021).
Wang, S. et al. Neutrophil-derived PAD4 induces citrullination of CKMT1 exacerbates mucosal inflammation in inflammatory bowel disease. Cell. Mol. Immunol. 21, 620–633 (2024).
Grieshaber-Bouyer, R. & Nigrovic, P. A. Neutrophil heterogeneity as therapeutic opportunity in immune-mediated disease. Front. Immunol. 10, 346 (2019).
Deniset, J. F. & Kubes, P. Neutrophil heterogeneity: Bona fide subsets or polarization states?. J. Leukoc. Biol. 103, 829–838 (2018).
van Grinsven, E. et al. Immature neutrophils released in acute inflammation exhibit efficient migration despite incomplete segmentation of the nucleus. J. Immunol.202, 207–217 (2019).
Drifte, G., Dunn-Siegrist, I., Tissières, P. & Pugin, J. Innate immune functions of immature neutrophils in patients with sepsis and severe systemic inflammatory response syndrome. Crit. Care Med. 41, 820–832 (2013).
Wang, L. et al. ROS-producing immature neutrophils in giant cell arteritis are linked to vascular pathologies. JCI Insight 5, https://doi.org/10.1172/jci.insight.139163 (2020).
Yao, X. et al. Neutrophil heterogeneity is modified during acute lung inflammation in Apoa1-/- mice. J. Immunol. 213, 456–468 (2024).
Bae, G. H. et al. Unique characteristics of lung-resident neutrophils are maintained by PGE2/PKA/Tgm2-mediated signaling. Blood 140, 889–899 (2022).
Devi, S. et al. Neutrophil mobilization via plerixafor-mediated CXCR4 inhibition arises from lung demargination and blockade of neutrophil homing to the bone marrow. J. Exp. Med. 210, 2321–2336 (2013).
Song, Z. et al. NADPH oxidase 2 limits amplification of IL-1β-G-CSF axis and an immature neutrophil subset in murine lung inflammation. Blood Adv. 7, 1225–1240 (2023).
Becker, N. et al. Club cell protein 16 attenuates CD16(bright)CD62(dim) immunosuppressive neutrophils in damaged tissue upon posttraumatic sepsis-induced lung injury. J. Immunol. Res. 2021, 6647753 (2021).
Leliefeld, P. H. C. et al. Differential antibacterial control by neutrophil subsets. Blood Adv. 2, 1344–1355 (2018).
Maali, Y. et al. Two transcriptionally and functionally distinct waves of neutrophils during mouse acute liver injury. Hepatol. Commun. 8, https://doi.org/10.1097/hc9.0000000000000459 (2024).
Umeshappa, C. S. et al. Liver-specific T regulatory type-1 cells program local neutrophils to suppress hepatic autoimmunity via CRAMP. Cell Rep. 34, 108919 (2021).
Wang, J. et al. Visualizing the function and fate of neutrophils in sterile injury and repair. Science 358, 111–116 (2017).
Cho, Y. et al. Neutrophil extracellular traps contribute to liver damage and increase defective low-density neutrophils in alcohol-associated hepatitis. J. Hepatol. 78, 28–44 (2023).
Mi, X. et al. Stimulation of liver fibrosis by N2 neutrophils in Wilson’s disease. Cell. Mol. Gastroenterol. Hepatol. 16, 657–684 (2023).
Li, J. et al. TGFβ1(+)CCR5(+) neutrophil subset increases in bone marrow and causes age-related osteoporosis in male mice. Nat. Commun. 14, 159 (2023).
Rambault, M. et al. Neutrophils encompass a regulatory subset suppressing T cells in apparently healthy cattle and mice. Front. Immunol. 12, 625244 (2021).
Creusat, F. et al. IFN-γ primes bone marrow neutrophils to acquire regulatory functions in severe viral respiratory infections. Sci. Adv. 10, eadn3257 (2024).
Deng, Y. et al. Expression characteristics of interferon-stimulated genes and possible regulatory mechanisms in lupus patients using transcriptomics analyses. EBioMedicine 70, 103477 (2021).
Skopelja-Gardner, S. et al. Acute skin exposure to ultraviolet light triggers neutrophil-mediated kidney inflammation. Proc. Natl. Acad. Sci. USA 118, https://doi.org/10.1073/pnas.2019097118 (2021).
Rudolph, V. et al. Myeloperoxidase acts as a profibrotic mediator of atrial fibrillation. Nat. Med. 16, 470–474 (2010).
Ma, Y. et al. Temporal neutrophil polarization following myocardial infarction. Cardiovasc. Res. 110, 51–61 (2016).
Li, Y. et al. S100a8/a9 signaling causes mitochondrial dysfunction and cardiomyocyte death in response to ischemic/reperfusion injury. Circulation 140, 751–764 (2019).
Lawrence, D. A. et al. Inflammatory and autoimmune aspects of multisystem inflammatory syndrome in children (MIS-C): a prospective cohort study. Viruses 16, https://doi.org/10.3390/v16060950 (2024).
Muto, T. et al. White blood cell and neutrophil counts and response to intravenous immunoglobulin in Kawasaki disease. Glob. Pediatr. Health 6, 2333794×19884826 (2019).
Gruber, C. N. et al. Mapping systemic inflammation and antibody responses in multisystem inflammatory syndrome in children (MIS-C. Cell 183, 982–995.e14 (2020).
Sacco, K. et al. Immunopathological signatures in multisystem inflammatory syndrome in children and pediatric COVID-19. Nat. Med. 28, 1050–1062 (2022).
Wang, J. et al. Excessive neutrophils and neutrophil extracellular traps in COVID-19. Front. Immunol. 11, 2063 (2020).
Yamashita, K., Takaori-Kondo, A. & Mizugishi, K. Exaggerated neutrophil extracellular trap formation in Kawasaki disease: a key phenomenon behind the outbreak in western countries. Ann. Rheum. Dis. 81, e177 (2022).
Aymonnier, K. et al. Inflammasome activation in neutrophils of patients with severe COVID-19. Blood Adv. 6, 2001–2013 (2022).
Shahi, A. et al. Potential roles of NLRP3 inflammasome in the pathogenesis of Kawasaki disease. J. Cell. Physiol. 238, 513–532 (2023).
Jin, J. et al. Neutrophil extracellular traps promote the activation of the NLRP3 inflammasome and PBMCs pyroptosis via the ROS-dependent signaling pathway in Kawasaki disease. Int. Immunopharmacol. 145, 113783 (2024).
Çaǧlayan, Ş et al. Anakinra treatment in multisystemic inflammatory syndrome in children (MIS-C) associated with COVID-19. Front. Pediatr. 10, 942455 (2022).
Dusser, P. et al. Subcutaneous anakinra in the management of refractory MIS-C in France. Front. Pediatr. 12, 1270878 (2024).
Taddio, A. et al. Early anakinra treatment improves cardiac outcome of multisystem inflammatory syndrome in children, regardless of disease severity. Rheumatology 63, 366–375 (2024).
Kessel, C. et al. An immunological axis involving interleukin 1β and leucine-rich-α2-glycoprotein reflects therapeutic response of children with Kawasaki disease: implications from the KAWAKINRA Trial. J. Clin. Immunol. 42, 1330–1341 (2022).
Ferrara, G. et al. Anakinra for treatment-resistant Kawasaki disease: evidence from a literature review. Paediatr. Drugs 22, 645–652 (2020).
Masso-Silva, J. A. et al. Abrogation of neutrophil inflammatory pathways and potential reduction of neutrophil-related factors in COVID-19 by intravenous immunoglobulin. Front. Immunol. 13, 993720 (2022).
Ganigara, M., Sharma, C. & Bayry, J. Unraveling the mechanisms of IVIG immunotherapy in MIS-C. Cell Rep. Med. 2, 100431 (2021).
Syrimi, E. et al. The immune landscape of SARS-CoV-2-associated Multisystem Inflammatory Syndrome in Children (MIS-C) from acute disease to recovery. iScience 24, 103215 (2021).
Zheng, Y. et al. Single-cell mapping of peripheral blood mononuclear cells reveals key transcriptomic changes favoring coronary artery lesion in IVIG-resistant Kawasaki disease. Heliyon 10, e37857 (2024).
Son, M. B. F. et al. Multisystem inflammatory syndrome in children—initial therapy and outcomes. N. Engl. J. Med. 385, 23–34 (2021).
Kobayashi, T. et al. Efficacy of immunoglobulin plus prednisolone for prevention of coronary artery abnormalities in severe Kawasaki disease (RAISE study): a randomised, open-label, blinded-endpoints trial. Lancet 379, 1613–1620 (2012).
Patel, H. et al. Shared neutrophil and T cell dysfunction is accompanied by a distinct interferon signature during severe febrile illnesses in children. Nat. Commun. 15, 8224 (2024).
Funding
This work was supported by grants from the National Natural Science Foundation of China (82400581, 82070512, and 82270529), Jiangsu Provincial Social Development Project (BE2021655), and Suzhou “Kejiaoxingwei” Youth Science Project (KJXW2023024). The funders had no role in data collection, preparation of the manuscript, and decision to publish.
Author information
Authors and Affiliations
Contributions
Nana Wang contributed to the relevant literature review and wrote the first draft of the manuscript. Ling Sun and Guanghui Qian helped with literature collection. Zhiheng Liu had primary responsibility for reviewing the design and writing the manuscript. Haitao Lv corrected the final draft of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, N., Sun, L., Qian, G. et al. Neutrophil heterogeneity in Kawasaki disease and multisystem inflammatory syndrome in children. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04200-z
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04200-z