Abstract
Background
Risk factors for cardiometabolic disease may have fetal origins, but the biological pathways linking gestational conditions to these risk factors are only partially understood.
Methods
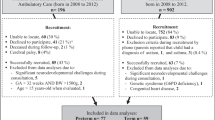
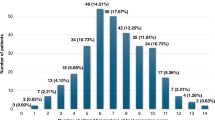
Among 145 Cincinnati-based HOME Study mother-child dyads, we detected 14,384 cord serum metabolic features using liquid chromatography high-resolution mass spectrometry. We measured cardiometabolic risk factors, including visceral fat, serum triglyceride, high-density lipoprotein cholesterol (HDL), leptin, adiponectin, insulin concentration, glucose, and systolic blood pressure (SBP) at age 12 years. Using sparse Partial Least Squares Regression (sPLS-R), we simultaneously modeled the association of metabolic features with all 8 risk factors. We prioritized features with the highest sPLS-R-derived CM risk factor correlations for metabolic pathway enrichment analysis.
Results
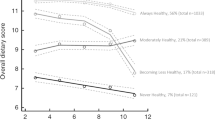
We identified two groups of cardiometabolic risk factors in adolescents maximally associated with neonatal metabolic features. The first was visceral fat, triglycerides, HDL, insulin, and leptin; the second was glucose and SBP. The 178 metabolic features with the highest sPLS-R-derived feature-outcome correlations were enriched in 31 pathways related to short-chain fatty acid, vitamins C and B3, and amino acid metabolism, as well as glycolysis and gluconeogenesis.
Conclusions
We identified 31 pathways that may help elucidate underlying mechanisms between fetal environmental stressors and the development of cardiometabolic risk factors.
Impact
-
Using non-targeted metabolomics, we identified neonatal metabolic features linked to two groups of cardiometabolic risk factors in adolescents, suggesting distinct early-life CM risk trajectories and adolescent subphenotypes.
-
One cardiometabolic group was characterized by higher visceral fat, triglycerides, insulin, leptin, as well as lower HDL; the other group was related to elevated glucose and systolic blood pressure.
-
Using a variable selection and data-dimension reduction technique, these two groups were associated with 178 metabolic features and 31 biological pathways related to short-chain fatty acid, vitamins C and B3, and amino acid metabolism, as well as glycolysis and gluconeogenesis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data are available upon reasonable request. The HOME Study Principal Investigators welcome new collaborations with other investigators and have actively engaged in collaborative data sharing projects. Interested investigators should visit https://homestudy.research.cchmc.org/contact or contact Drs Joseph M. Braun (joseph_braun_1@brown. edu) and Kimberly Yolton (kimberly.yolton@cchmc.org) to obtain additional information about The HOME Study, discuss collaborative opportunities, and request a project proposal form. The HOME Study Protocol Review Committee reviews proposed research projects to ensure that they do not overlap with extant projects and are an efficient use of scarce resources (eg, biospecimens).
References
Benziger, C. P., Roth, G. A. & Moran, A. E. The global burden of disease study and the preventable burden of NCD. Glob. Heart 11, 393–397 (2016).
Wang, H. et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388, 1459–1544 (2016).
Ahmad, F. B. & Anderson, R. N. The leading causes of death in the US for 2020. JAMA 325, 1829–1830 (2021).
Heron, M. P. Deaths: leading causes for 2018. Natl. Vital Stat. Rep. 60, 1–94 (2021).
Lurbe, E. et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J. Hypertens. 34, 1887–1920 (2016).
Lurbe, E. & Ingelfinger, J. Developmental and early life origins of cardiometabolic risk factors: novel findings and implications. Hypertension 77, 308–318 (2021).
Drozdz, D. et al. Obesity and cardiometabolic risk factors: from childhood to adulthood. Nutrients 13, 4176 (2021).
Tsao, C. W. et al. Heart disease and stroke statistics—2023 update: a report from the American Heart Association. Circulation 147, e93–e621 (2023).
American Diabetes Association Professional Practice Committee. 2. Diagnosis and classification of diabetes: standards of care in diabetes—2024. Diabetes Care 47, S20–S42 (2024).
Magge, S. N. et al. The metabolic syndrome in children and adolescents: shifting the focus to cardiometabolic risk factor clustering. Pediatrics 140, e20171603 (2017).
Kelly, A. S. et al. Predicting cardiovascular risk in young adulthood from the metabolic syndrome, its component risk factors, and a cluster score in childhood. Int. J. Pediatr. Obes. 6, e283–e289 (2011).
Azab, S. M. et al. Metabolite profiles and the risk of metabolic syndrome in early childhood: a case-control study. BMC Med. 19, 292 (2021).
Rinaudo, P. & Wang, E. Fetal programming and metabolic syndrome. Annu Rev. Physiol. 74, 107–130 (2012).
Wadhwa, P. D., Buss, C., Entringer, S. & Swanson, J. M. Developmental origins of health and disease: brief history of the approach and current focus on epigenetic mechanisms. Semin Reprod. Med. 27, 358–368 (2009).
Wishart, D. S. Metabolomics for investigating physiological and pathophysiological processes. Physiol. Rev. 99, 1819–1875 (2019).
Snyder, B. M. et al. The associations of maternal health characteristics, newborn metabolite concentrations, and child body mass index among US children in the ECHO program. Metabolites 13, 510 (2023).
Schlueter, R. J. et al. Prepregnant obesity of mothers in a multiethnic cohort is associated with cord blood metabolomic changes in offspring. J. proteome Res. 19, 1361–1374 (2020).
Patel, N. et al. Cord metabolic profiles in obese pregnant women: insights into offspring growth and body composition. J. Clin. Endocrinol. Metab. 103, 346–355 (2017).
Mansell, T. et al. The newborn metabolome: associations with gestational diabetes, sex, gestation, birth mode, and birth weight. Pediatr. Res. 91, 1864–1873 (2022).
Zhao, C. et al. Integrated metabolome analysis reveals novel connections between maternal fecal metabolome and the neonatal blood metabolome in women with gestational diabetes mellitus. Sci. Rep. 10, 3660 (2020).
Hao, H. et al. The influence of pregnancy-induced hypertension syndrome on the metabolism of newborns. Transl. Pediatr. 10, 296–305 (2021).
Cajachagua-Torres, K. N. et al. Fetal exposure to maternal smoking and neonatal metabolite profiles. Metabolites 12. https://doi.org/10.3390/metabo12111101 (2022).
Rolle-Kampczyk, U. E. et al. Metabolomics reveals effects of maternal smoking on endogenous metabolites from lipid metabolism in cord blood of newborns. Metabolomics 12, 76 (2016).
Snyder, B. M. et al. Associations between Smoking and Smoking Cessation during Pregnancy and Newborn Metabolite Concentrations: Findings from PRAMS and INSPIRE Birth Cohorts. Metabolites 13, 1163 (2023).
Vidarsdottir, H. et al. Does metabolomic profile differ with regard to birth weight?. Pediatr. Res. 89, 1144–1151 (2021).
Zhai, X. et al. Nontargeted metabolomics reveals the potential mechanism underlying the association between birthweight and metabolic disturbances. BMC Pregnancy Childbirth 23, 1–13 (2023).
Priante, E. et al. Metabolomic profiling of intrauterine growth-restricted preterm infants: a matched case–control study. Pediatr. Res. 93, 1599–1608 (2023).
Wojczakowski, W. et al. Preeclampsia and cardiovascular risk for offspring. J. Clin. Med. 10, 3154 (2021).
Joung, K. E., Lee, J. & Kim, J. H. Long-term metabolic consequences of intrauterine growth restriction. Curr. Pediatr. Rep. 8, 45–55 (2020).
Kataria, Y., Gaewsky, L. & Ellervik, C. Prenatal smoking exposure and cardio-metabolic risk factors in adulthood: a general population study and a meta-analysis. Int. J. Obes. 43, 763–773 (2019).
Hrolfsdottir, L. et al. Gestational weight gain in normal weight women and offspring cardio-metabolic risk factors at 20 years of age. Int. J. Obes. 39, 671–676 (2015).
Cao, T. et al. Cord blood metabolome and BMI trajectory from birth to adolescence: a prospective birth cohort study on early life biomarkers of persistent obesity. Metabolites 11, 739 (2021).
Zhang, M. et al. Metabolome-wide association study of cord blood metabolites with blood pressure in childhood and adolescence. Hypertension 79, 2806–2820 (2022).
Hellmuth, C. et al. Cord blood metabolome is highly associated with birth weight, but less predictive for later weight development. Obes. Facts 10, 85–100 (2017).
Braun, J. M. et al. Cohort profile: the health outcomes and measures of the environment (HOME) study. Int. J. Epidemiol. 46, 24–24 (2016).
Braun, J. M. et al. Adolescent follow-up in the health outcomes and measures of the environment (HOME) study: cohort profile. BMJ Open 10, e034838 (2020).
Hall, A. M. et al. Associations of a prenatal serum per-and polyfluoroalkyl substance mixture with the cord serum metabolome in the HOME study. Environ. Sci. Technol. 57, 21627–21636 (2023).
Kingsley, S. L. et al. Metabolomics of childhood exposure to perfluoroalkyl substances: a cross-sectional study. Metabolomics 15, 1–12 (2019).
Liu, K. H. et al. Reference standardization for quantification and harmonization of large-scale metabolomics. Anal. Chem. 92, 8836–8844 (2020).
Yu, T., Park, Y., Johnson, J. M. & Jones, D. P. apLCMS—adaptive processing of high-resolution LC/MS data. Bioinformatics 25, 1930–1936 (2009).
Deng, K. et al. WaveICA 2.0: a novel batch effect removal method for untargeted metabolomics data without using batch information. Metabolomics 17, 1–8 (2021).
Li, N. et al. Gestational and childhood exposure to per-and polyfluoroalkyl substances and cardiometabolic risk at age 12 years. Environ. Int. 147, 106344 (2021).
Lacruz, M. E. et al. Short-term blood pressure variability–variation between arm side, body position and successive measurements: a population-based cohort study. BMC Cardiovasc. Disord. 17, 1–9 (2017).
Braun, J. M. et al. Gestational perfluoroalkyl substance exposure and body mass index trajectories over the first 12 years of life. Int. J. Obes. 45, 25–35 (2021).
Rohart, F., Gautier, B., Singh, A. & Lê Cao, K.-A. mixOmics: an R package for ‘omics feature selection and multiple data integration. PLoS Comput. Biol. 13, e1005752 (2017).
Lê Cao, K.-A., Rossouw, D., Robert-Granié, C. & Besse, P. A sparse PLS for variable selection when integrating omics data. Stat. Appl. Genet. Mol. Biol. 7, 35 (2008).
Chun, H. & Keleş, S. Sparse partial least squares regression for simultaneous dimension reduction and variable selection. J. R. Stat. Soc. Ser. B Stat. Methodol. 72, 3–25 (2010).
González, I., Cao, K.-A. L., Davis, M. J. & Déjean, S. Visualising associations between paired ‘omics’ data sets. BioData Min. 5, 1–23 (2012).
Pang, Z. et al. MetaboAnalystR 4.0: a unified LC-MS workflow for global metabolomics. Nat. Commun. 15, 3675 (2024).
Schymanski, E. L. et al. Identifying small molecules via high resolution mass spectrometry: communicating confidence. Environ. Sci. Technol. 48, 2097–2098 (2014).
Steinberger, J. et al. Cardiovascular health promotion in children: challenges and opportunities for 2020 and beyond: a scientific statement from the American Heart Association. Circulation 134, e236–e255 (2016).
Stefan, N. & Schulze, M. B. Metabolic health and cardiometabolic risk clusters: implications for prediction, prevention, and treatment. Lancet Diabetes Endocrinol. 11, 426–440 (2023).
Tripathi, P. et al. Comparison of clustering and phenotyping approaches for subclassification of type 2 diabetes and its association with remission in Indian population. Sci. Rep. 14, 20260 (2024).
Wagner, R. et al. Pathophysiology-based subphenotyping of individuals at elevated risk for type 2 diabetes. Nat. Med. 27, 49–57 (2021).
Beyene, H. B. et al. Metabolic phenotyping of BMI to characterize cardiometabolic risk: evidence from large population-based cohorts. Nat. Commun. 14, 6280 (2023).
Schulze, M. B. & Stefan, N. Metabolically healthy obesity: from epidemiology and mechanisms to clinical implications. Nat. Rev. Endocrinol. 20, 633–646 (2024).
Zhan, J. et al. Left ventricular myocardial work indices in pediatric hypertension: correlations with conventional echocardiographic assessment and subphenotyping. Eur. J. Pediatr. 181, 2643–2654 (2022).
Melka, M. G. et al. Clustering of the metabolic syndrome components in adolescence: role of visceral fat. PLoS ONE 8, e82368 (2013).
Yuan, W. L. et al. The adverse influence of maternal glycaemia during pregnancy on offspring's cardiometabolic health profiles. Acta Paediatr. 114, 2287–2297 (2025).
Rice, M. M. et al. Pregnancy-associated hypertension and offspring cardiometabolic health. Obstet. Gynecol. 131, 313–321 (2018).
Macfarlane, S. & Macfarlane, G. T. Regulation of short-chain fatty acid production. Proc. Nutr. Soc. 62, 67–72 (2003).
Chang, Y. et al. Short-chain fatty acids accompanying changes in the gut microbiome contribute to the development of hypertension in patients with preeclampsia. Clin. Sci. 134, 289–302 (2020).
Li, J. et al. The diagnostic potential of gut microbiota-derived short-chain fatty acids in preeclampsia. Front. Pediatr. 10, 878924 (2022).
Gomez-Arango, L. F. et al. Increased systolic and diastolic blood pressure is associated with altered gut microbiota composition and butyrate production in early pregnancy. Hypertension 68, 974–981 (2016).
Priyadarshini, M. et al. Maternal short-chain fatty acids are associated with metabolic parameters in mothers and newborns. Transl. Res. 164, 153–157 (2014).
Coppola, S. et al. Therapeutic effects of butyrate on pediatric obesity: a randomized clinical trial. JAMA Netw. Open 5, e2244912–e2244912 (2022).
Chambers, E. S. et al. Effects of targeted delivery of propionate to the human colon on appetite regulation, body weight maintenance and adiposity in overweight adults. Gut 64, 1744–1754 (2015).
Goffredo, M. et al. Role of gut microbiota and short chain fatty acids in modulating energy harvest and fat partitioning in youth. J. Clin. Endocrinol. Metab. 101, 4367–4376 (2016).
Solinas, G., Borén, J. & Dulloo, A. G. De novo lipogenesis in metabolic homeostasis: More friend than foe?. Mol. Metab. 4, 367–377 (2015).
Miller, T. L. & Wolin, M. J. Pathways of acetate, propionate, and butyrate formation by the human fecal microbial flora. Appl. Environ. Microbiol. 62, 1589–1592 (1996).
Dasgupta, S. et al. Discovery of novel metabolic signatures for early identification of women at risk of developing gestational hypertension. Metabolomics 19, 50 (2023).
Menon, R. et al. Amniotic fluid metabolomic analysis in spontaneous preterm birth. Reprod. Sci. 21, 791–803 (2014).
Gui, S. et al. Arginine supplementation for improving maternal and neonatal outcomes in hypertensive disorder of pregnancy: a systematic review. J. ReninAngiotensinAldosterone Syst. 15, 88–96 (2014).
Zhao, J. et al. Causal effects of maternal circulating amino acids on offspring birthweight: a Mendelian randomisation study. EBioMedicine 88, 104441 (2023).
De Spiegeleer, M. et al. Paediatric obesity: a systematic review and pathway mapping of metabolic alterations underlying early disease processes. Mol. Med. 27, 1–20 (2021).
Liang, H. & Song, K. Elucidating ascorbate and aldarate metabolism pathway characteristics via integration of untargeted metabolomics and transcriptomics of the kidney of high-fat diet-fed obese mice. Plos ONE 19, e0300705 (2024).
Roberts, J. M. et al. Vitamins C and E to prevent complications of pregnancy-associated hypertension. N. Engl. J. Med. 362, 1282–1291 (2010).
García, O. P. et al. Zinc, iron and vitamins A, C and E are associated with obesity, inflammation, lipid profile and insulin resistance in Mexican school-aged children. Nutrients 5, 5012–5030 (2013).
Ashor, A. W. et al. Limited evidence for a beneficial effect of vitamin C supplementation on biomarkers of cardiovascular diseases: an umbrella review of systematic reviews and meta-analyses. Nutr. Res. 61, 1–12 (2019).
Takahashi, N. et al. Vitamin B3 nicotinamide: a promising candidate for treating preeclampsia and improving fetal growth. Tohoku J. Exp. Med. 244, 243–248 (2018).
Georgakopoulou, I. et al. Metabolic changes in early neonatal life: NMR analysis of the neonatal metabolic profile to monitor postnatal metabolic adaptations. Metabolomics 16, 1–12 (2020).
Knapen, M. F., Zusterzeel, P. L., Peters, W. H. & Steegers, E. A. Glutathione and glutathione-related enzymes in reproduction: a review. Eur. J. Obstet. Gynecol. Reprod. Biol. 82, 171–184 (1999).
Fragoso, M. B. T. et al. Biomarkers of inflammation and redox imbalance in umbilical cord in pregnancies with and without preeclampsia and consequent perinatal outcomes. Oxidative Med. Cell. Longev. 2021, 9970627 (2021).
Küster, A. et al. Cord blood glutathione depletion in preterm infants: correlation with maternal cysteine depletion. PLoS One 6, e27626 (2011).
Jain, A. et al. Glutathione metabolism in newborns: evidence for glutathione deficiency in plasma, bronchoalveolar lavage fluid, and lymphocytes in prematures. Pediatr. Pulmonol. 20, 160–166 (1995).
Alkazemi, D., Rahman, A. & Habra, B. Alterations in glutathione redox homeostasis among adolescents with obesity and anemia. Sci. Rep. 11, 3034 (2021).
Gou, R. & Zhang, X. Glycolysis: a fork in the path of normal and pathological pregnancy. FASEB J. 37, e23263 (2023).
Donauer, S. et al. An observational study to evaluate associations between low-level gestational exposure to organophosphate pesticides and cognition during early childhood. Am. J. Epidemiol. 184, 410–418 (2016).
Valo, E. et al. Effect of serum sample storage temperature on metabolomic and proteomic biomarkers. Sci. Rep. 12, 4571 (2022).
Wagner-Golbs, A. et al. Effects of long-term storage at −80 °C on the human plasma metabolome. Metabolites 9, 99 (2019).
Funding
This work was supported by National Institute of Environmental Health Sciences grants R01 ES032386, R01 ES025214, P01 ES011261, R01 ES014575, R01 ES020349, R01 ES027224, R01 ES030078 and R01 ES033252.
Author information
Authors and Affiliations
Contributions
G.D.P., E.S.C.F., and J.M.B. conceptualized the study. K.M., K.P., D.W., K.Y., and K.C. acquired the data. G.D.P. and E.S.C.F. analyzed the data. G.D.P., E.S.C.F., and J.M.B. interpreted the data. E.S.C.F. and G.D.P. drafted the article. K.E.M., K.P., A.M.H., A.C., J.P.B., K.Y., K.M.C., B.P.L., C.B.E., D.I.W., and J.M.B. revised it critically for important intellectual content. E.S.C.F., G.D.P., K.E.M., K.P., A.M.H., A.C., J.P.B., K.Y., K.M.C., B.P.L., C.B.E., D.I.W., and J.M.B. approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
Joseph Braun was compensated for serving as an expert witness for plaintiffs in litigation related to PFAS-contaminated drinking water.
Consent statement
The Institutional Review Boards (IRBs) of Cincinnati Children’s Hospital Medical Center (CCHMC) and all delivery hospitals approved the study protocol. The Centers for Disease Control and Prevention and Brown University deferred to the CCHMC IRB as the IRB of record. Women provided written informed consent for themselves and their children. Children provided written assent at the age 12 visit.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fleury, E.S., Papandonatos, G.D., Manz, K.E. et al. Evaluating neonatal cord serum metabolome in association with adolescent cardiometabolic risk factors. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04322-4
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04322-4
This article is cited by
-
Cord blood metabolomics: a window into future heart health
Pediatric Research (2025)