Abstract
Background
Metabolic alkalosis (MA) is a common complication of congenital hypertrophic pyloric stenosis (CHPS). This study develops and validates a nomogram to predict MA probability in CHPS infants.
Methods
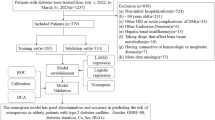
A retrospective study was conducted on CHPS patients at the First Affiliated Hospital of Zhengzhou University. Patients were divided into CHPS and MA-CHPS groups. Lasso and logistic regression selected predictive factors, and a nomogram was developed. Discriminative ability was assessed using the C-index with bootstrap validation. Calibration curves evaluated predictive accuracy, while decision curve analysis (DCA) assessed clinical applicability.
Results
A total of 107 cases were included in the final analysis, with 81 in the CHPS group and 26 in the MA-CHPS group. The predictive nomogram included the following factors: weight at diagnosis, symptom duration, and pyloric index (PI). The C-index of the predictive nomogram was determined to be 0.818, with a bootstrap validation (1000 resamples) yielding a corrected C-index of 0.798, indicating good discriminative ability. Calibration curves demonstrated a high degree of consistency between predicted and actual results. DCA confirmed good clinical utility.
Conclusion
We developed a nomogram to predict the probability of MA in CHPS patients, enabling early identification of poor prognosis and improving outcomes.
Impact statement
-
This study presents a novel predictive model for assessing the probability of metabolic alkalosis (MA) in congenital hypertrophic pyloric stenosis (CHPS) infants. It is the first model integrating the pyloric index (PI) as a predictive factor, alongside weight at diagnosis and symptom duration. The nomogram demonstrated strong discriminative ability and clinical utility, aiding early MA identification and improving perioperative management. By providing a practical risk stratification tool, this model enhances clinical decision-making, facilitates timely interventions, and ultimately improves outcomes for CHPS infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others

Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Alain, J. L., Grousseau, D. & Terrier, G. Extramucosal pyloromyotomy by laparoscopy. Surgical Endosc. 5, 174–175 (1991).
Rich, B. S. & Dolgin, S. E. Hypertrophic pyloric stenosis. Pediatrics Rev. 42, 539–545 (2021).
Jobson, M. & Hall, N. J. Contemporary management of pyloric stenosis. Semin. Pediatr. Surg. 25, 219–224 (2016).
Touloukian, R. J. & Higgins, E. The spectrum of serum electrolytes in hypertrophic pyloric stenosis. J. Pediatr. Surg. 18, 394–397 (1983).
Breaux, C. W. Jr, Hood, J. S. & Georgeson, K. E. The significance of alkalosis and hypochloremia in hypertrophic pyloric stenosis. J. Pediatr. Surg. 24, 1250–1252 (1989).
Ohri, S. K., Sackier, J. M. & Singh, P. Modified Ramstedt’s pyloromyotomy for the treatment of infantile hypertrophic pyloric stenosis. J. R. Coll. Surg. Edinb. 36, 94–96 (1991).
Downey, E. C. Jr Laparoscopic pyloromyotomy. Semin. Pediatr. Surg. 7, 220–224 (1998).
Goh, D. W. et al. Plasma chloride and alkalaemia in pyloric stenosis. Br. J. Surg. 77, 922–923 (1990).
van den Bunder, F. et al. Respiratory problems owing to severe metabolic alkalosis in infants presenting with hypertrophic pyloric stenosis. J. Pediatr. Surg. 55, 2772–2776 (2020).
Nissen, M. et al. Does metabolic alkalosis influence cerebral oxygenation in infantile hypertrophic pyloric stenosis?. J. surgical Res. 212, 229–237 (2017).
van den Bunder, F. et al. Perioperative hypoxemia and postoperative respiratory events in infants with hypertrophic pyloric stenosis. Eur. J. Pediatr. Surg. J. Austrian Assoc. Pediatr. Surg. [et al.] Z. fur Kinderchir. 33, 485–492 (2023).
Khan, A. A., Yousaf, M. A. & Ashraf, M. Role of ultrasonography in early diagnosis of infantile hypertrophic pyloric stenosis. J. Ayub Med. Coll., Abbottabad: JAMC 26, 316–319 (2014).
AlMaramhy, H. H. Is there a relation between pyloric muscle thickness and clinical and laboratory data in infants with hypertrophic pyloric stenosis?. Indian J. Surg. 77, 827–830 (2015).
Kim, H. J. Utility of pyloric length measurement for detecting severe metabolic alkalosis in infants with hypertrophic pyloric stenosis. Pediatr. Gastroenterol., Hepatol. Nutr. 27, 88–94 (2024).
Kaya, B. et al. Pyloric index, a new parameter: predicting perioperative prognosis in neonates with hypertrophic pyloric stenosis. Scand. J. Gastroenterol. 59, 1272–1276 (2024).
Hussain, M. Sonographic diagnosis of infantile hypertrophic pyloric stenosis- use of simultaneous grey-scale & colour doppler examination. Int. J. Health Sci. 2, 134–140 (2008).
Zaghal, A., El-Majzoub, N., Jaafar, R., Aoun, B. & Jradi, N. Brief overview and updates on infantile hypertrophic pyloric stenosis: focus on perioperative management. Pediatr. Ann. 50, e136–e141 (2021).
Westra, S. J., de Groot, C. J., Smits, N. J. & Staalman, C. R. Hypertrophic pyloric stenosis: use of the pyloric volume measurement in early US diagnosis. Radiology 172, 615–619 (1989).
van den Bunder, F., Hall, N. J., van Heurn, L. W. E. & Derikx, J. P. M. A delphi analysis to reach consensus on preoperative care in infants with hypertrophic pyloric stenosis. Eur. J. Pediatr. Surg. J. Austrian Assoc. Pediatr. Surg. [et al.] = Z. fur Kinderchir. 30, 497–504 (2020).
Tutay, G. J., Capraro, G., Spirko, B., Garb, J. & Smithline, H. Electrolyte profile of pediatric patients with hypertrophic pyloric stenosis. Pediatr. Emerg. care 29, 465–468 (2013).
Bašković, M., Župančić, B., Lesjak, N. & Vukasović, I. Hypertrophic Pyloric Stenosis - Five-Year Retrospective Analysis. Acta Med. Croatica Cas. Hravatske akademije medicinskih Znan. 70, 103–106 (2016).
Ramsay, P. T. & Carr, A. Gastric acid and digestive physiology. Surgical Clin. North Am. 91, 977–982 (2011).
McCauley, M., Gunawardane, M. & Cowan, M. J. Severe metabolic alkalosis due to pyloric obstruction: case presentation, evaluation, and management. Am. J. Med. Sci. 332, 346–350 (2006).
Palmer, B. F. Potassium binders for hyperkalemia in chronic kidney disease-diet, renin-angiotensin-aldosterone system inhibitor therapy, and hemodialysis. Mayo Clin. Proc. 95, 339–354 (2020).
Terano, C. et al. Incidence of and risk factors for severe acute kidney injury in children with heart failure treated with renin-angiotensin system inhibitors. Eur. J. Pediatrics 175, 631–637 (2016).
Ndongo, R. et al. Infantile hypertrophic pyloric stenosis: a 4-year experience from two tertiary care centres in cameroon. BMC Res. Notes 11, 33 (2018).
Feng, Z. et al. The clinical features of infantile hypertrophic pyloric stenosis in Chinese Han Population: analysis from 1998 to 2010. PloS one 9, e88925 (2014).
Shaoul, R., Enav, B., Steiner, Z., Mogilner, J. & Jaffe, M. Clinical presentation of pyloric stenosis: the change is in our hands. Isr. Med. Assoc. J. : IMAJ 6, 134–137 (2004).
Labrune, P., Myara, A., Huguet, P., Trivin, F. & Odievre, M. Jaundice with hypertrophic pyloric stenosis: a possible early manifestation of Gilbert syndrome. J. Pediatrics 115, 93–95 (1989).
Hannam, S., McDonnell, M. & Rennie, J. M. Investigation of prolonged neonatal jaundice. Acta Paediatrica 89, 694–697 (2000).
Nobili, V., Alisi, A., Panera, N. & Agostoni, C. Low birth weight and catch-up-growth associated with metabolic syndrome: a ten year systematic review. Pediatr. Endocrinol. Rev. 6, 241–247 (2008).
Bhatia, J. Fluid and electrolyte management in the very low birth weight neonate. J. Perinatol. J. Calif. Perinat. Assoc. 26, S19–S21 (2006).
Ezomike, U. O., Ekenze, S. O., Amah, C. C., Nwankwo, E. P. & Obianyo, N. E. Infantile hypertrophic pyloric stenosis - our experience and challenges in a developing country. Afr. J. Paediatr. Surg. 15, 26–30 (2018).
Li, J., Gao, W., Zhu, J. M., Zuo, W. & Liu, X. Epidemiological and clinical characteristics of 304 patients with infantile hypertrophic pyloric stenosis in Anhui Province of East China, 2012-2015. J. Matern. -fetal neonatal Med. J. Eur. Assoc. Perinat. Med. Federation Asia Ocean. Perinat. Societies, Int. Soc. Perinat. Obstet. 31, 2742–2747 (2018).
Peters, B., Oomen, M. W., Bakx, R. & Benninga, M. A. Advances in infantile hypertrophic pyloric stenosis. Expert Rev. Gastroenterol. Hepatol. 8, 533–541 (2014).
Acknowledgements
The authors are grateful to those who contributed to this study. We confirm that no Large Language Models (LLMs), including ChatGPT or similar AI-based technologies, were used in the conceptualization, writing, analysis, or editing of this manuscript. All content was independently developed, reviewed, and approved by the authors, ensuring full accountability and compliance with the journal’s authorship criteria.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The project was funded by the Key Scientific Research Projects of Henan Higher Education Institutions (No. 24A320078), the Science and Technology Research Program of Henan Province (No. 242102310256), and the Nursing Research Special Fund of the First Affiliated Hospital of Zhengzhou University (No. HLKY2023015).
Author information
Authors and Affiliations
Contributions
F.Y.C. contributed to data curation, formal analysis, and writing of the original draft. Z.D. and D.J. contributed to supervision. C.J., Z.X., Q.X.H. contributed to methodology. W.Y.Y., W.J.Y., L.S.K., D.J. and Z.D. contributed to conceptualization, reviewing and editing, and resources. All authors approved the final manuscript as submitted.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the Ethics Committees of the First Affiliated Hospital of Zhengzhou University (Approval Number No. 2025-KY-0737-001).
Informed consent
This was a retrospective study, so the requirement for informed consent was waived.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fu, Y., Cheng, J., Zhou, X. et al. Pyloric index: a novel nomogram predictor of metabolic alkalosis in congenital hypertrophic pyloric stenosis. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04382-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04382-6