Abstract
Background
Limited studies focused on characteristics of childhood-onset Takayasu arteritis (cTAK) throughout growth and development.
Methods
111 cTAK patients were recruited from six tertiary hospitals across China from January 2009 to December 2021. Patients were classified into infant group (<12 months), toddler and preschool group (≥12 months, <72 months), school-age group (≥72 months, <144 months) and adolescent group (≥144 months).
Results
Infantile cTAK patients tended to had a significantly higher proportion presenting with fever (91.7%, P-trend <0.001), and had significantly higher levels of C-reactive protein (CRP), white blood cells (WBC), platelet (PLT), and lower hemoglobin (HGB) compared to the other three groups (all P < 0.0125). Adolescent patients were more likely to present with headache (33.3%), dizziness (24.2%) and fatigue (51.5%; all P-trend < 0.001). Infantile patients were more likely to have coronary artery involvement (75.0%, P trend < 0.001). Adolescent patients were more likely to have superior mesenteric artery (36.4%, P trend = 0.005), carotid artery (30.3%, P trend = 0.003), and celiac trunk artery stenosis (27.3%, P trend = 0.005).Younger patients, especially infants, had a lower proportion of glucocorticoids use (P trend = 0.001). 73.0% (81/111) of patients were in remission, with a median follow-up time of 2.00 [2.00, 5.00] years.
Conclusion
The age-specific patterns identified in this study offered valuable insights for a comprehensive understanding of cTAK.
Impact
-
Infantile Takayasu arteritis patients tended to present with fever, elevated inflammatory biomarkers and coronary artery involvement. Adolescent patients were more likely to present with headache, dizziness and fatigue, with superior mesenteric artery, carotid artery involvement and celiac trunk artery stenosis.
-
Clinical manifestations and vascular involvement of childhood-onset Takayasu arteritis differ across age groups.
-
The clinical manifestations of childhood-onset Takayasu arteritis lack specificity. The age-specific patterns identified in this study may provide clues for early diagnosis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The dataset analyzed for the current study is available from the corresponding author upon reasonable request.
References
Maz, M. et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Giant Cell Arteritis and Takayasu Arteritis. Arthritis Rheumatol. 73, 1349–1365 (2021).
Kerr, G. S. et al. Takayasu Arteritis. Ann. Intern Med. 120, 919–929 (1994).
Fan, L. et al. Clinical scenario and long-term outcome of childhood Takayasu Arteritis undergoing 121 endovascular interventions: a large cohort over a Fifteen-Year Period. Arthritis Care Res. 73, 1678–1688 (2021).
Hassold, N. et al. Clinical spectrum and outcome of Takayasu’s Arteritis in Children. Jt. Bone Spine 91, 105735 (2024).
Rathore, U., Chandwar, K., Singh, K. & Misra, D. P. Pediatric-onset Takayasu Arteritis is associated with greater risk of mortality than adult-onset Takayasu Arteritis-a systematic review with meta-analysis of observational Cohort studies. Semin. Arthritis Rheum. 65, 152355 (2024).
Misra, D. P. et al. Paediatric-onset Takayasu’s Arteritis associates with worse survival than adult-onset Takayasu’s Arteritis. A matched retrospective cohort Study. Clin. Exp. Rheumatol. 42, 914–922 (2024).
Ishikawa, K. & Maetani, S. Long-term outcome for 120 Japanese patients with Takayasu’s disease. clinical and statistical analyses of related prognostic factors. Circulation 90, 1855–1860 (1994).
Ren, X. et al. Assessment of coronary involvement with Mdct and long-term outcomes in patients with Takayasu’s arteritis. Acad. Radio. 31, 4329–4339 (2024).
Zhao, X. et al. Clinical characteristics, treatment, and outcome of 43 cases of infant-onset Takayasu Arteritis. Indian J. Pediatr. 90, 416 (2023).
Miller-Barmak, A. et al. Infantile Takayasu: clinical features and long-term outcome. Rheumatology 62, 3126–3132 (2023).
Jin, J. et al. A retrospective study of infantile-onset Takayasu Arteritis: experience from a tertiary referral center in China. Front. Cardiovasc. Med. 11, 1249305 (2024).
Pavić, R., Blažeković, R., Divković, D., Marjanović, K. & Sipl, M. Aggressive progression of Takayasu’s Arteritis in infancy: a case report. Acta Clin. Croat. 58, 535–539 (2019).
Liu, H., Sun, L., Upadhyaya, R. S., Chen, Y. & Ajoje, O. O. Case report: Takayasu Arteritis in a 3-month-old Chinese Girl. Medicine 97, e12637 (2018).
Wang, E. L., Sato, Y., Takeichi, T. & Kitamura, O. Sudden death of an infant with coronary involvement due to Takayasu Arteritis. Cardiovasc. Pathol. 22, 109–111 (2013).
Clemente, G. et al. Takayasu Arteritis in childhood: misdiagnoses at disease onset and associated diseases. Rheumatol. Int. 38, 1089–1094 (2018).
Ozen, S. et al. Eular/Printo/Pres Criteria for Henoch-Schönlein Purpura, Childhood Polyarteritis Nodosa, Childhood Wegener Granulomatosis and Childhood Takayasu Arteritis: Ankara 2008. Part Ii: Final Classification Criteria. Ann. Rheum. Dis. 69, 798–806 (2010).
Arend, W. P. et al. The American College of Rheumatology 1990 criteria for the classification of Takayasu Arteritis. Arthritis Rheum. 33, 1129–1134 (1990).
Lupi-Herrera, E. et al. Takayasu’s Arteritis. Clinical Study of 107 Cases. Am. Heart J. 93, 94–103 (1977).
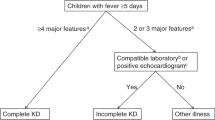
McCrindle, B. W. et al. Diagnosis, treatment, and long-term management of Kawasaki Disease: a scientific statement for health professionals from the american heart association. Circulation 135, e927–e999 (2017).
Misra, D. P. et al. Presentation and clinical course of pediatric-onset versus adult-onset Takayasu Arteritis-a systematic review and meta-analysis. Clin. Rheumatol. 41, 3601–3613 (2022).
Karabacak, M. et al. Childhood-onset versus adult-onset Takayasu Arteritis: a study of 141 patients from Turkey. Semin. Arthritis Rheum. 51, 192–197 (2021).
Danda, D. et al. Clinical course of 602 patients with Takayasu’s Arteritis: comparison between childhood-onset versus adult onset disease. Rheumatology60, 2246–2255 (2021).
Cong, X. L. et al. Takayasu’s Arteritis: clinical features and outcomes of 125 patients in China. Clin. Rheumatol. 29, 973–981 (2010).
Clemente, G. et al. Brazilian multicenter study of 71 patients with juvenile-onset Takayasu’s Arteritis: clinical and angiographic features. Rev. Bras. Reumatol. Engl. Ed. 56, 145–151 (2016).
Peremans, L. et al. Real-World Biomarkers for Pediatric Takayasu Arteritis. Int. J. Mol. Sci. 25, 7345 (2024).
Kong, F., Xu, Y., Huang, X., Lai, J. & Zhao, Y. Childhood-onset versus adult-onset Takayasu Arteritis: a study of 239 patients from China. Jt. Bone Spine 92, 105806 (2024).
Pérez-Pomares, J. M. et al. Congenital coronary artery anomalies: a bridge from embryology to anatomy and pathophysiology-a position statement of the development, anatomy, and pathology Esc Working Group. Cardiovasc. Res. 109, 204–216 (2016).
Xu, Y. et al. Clinical characteristics and risk factors of coronary artery lesions in chinese pediatric Takayasu Arteritis patients: a retrospective study. Pediatr. Rheumatol. Online J. 21, 42 (2023).
Maccora, I. et al. Long-term follow-up of coronary artery lesions in children in Kawasaki syndrome. Eur. J. Pediatr. 180, 271–275 (2021).
Jia, W. et al. Decreased absolute number of circulating regulatory T cells in patients with Takayasu’s Arteritis. Front. Immunol. 12, 768244 (2021).
Watanabe, R., Berry, G. J., Liang, D. H., Goronzy, J. J. & Weyand, C. M. Pathogenesis of giant cell arteritis and Takayasu Arteritis-similarities and differences. Curr. Rheumatol. Rep. 22, 68 (2020).
Zhao, Q. M. et al. Systemic artery Aneurysms and Kawasaki disease. Pediatrics 144, e20192254 (2019).
Burns, J. C. et al. Infliximab versus second intravenous immunoglobulin for treatment of resistant Kawasaki disease in the USA (Kidcare): a randomised, multicentre comparative effectiveness trial. Lancet Child Adolesc. Health 5, 852–861 (2021).
Wang, Z. et al. Methylprednisolone pulse therapy or additional Ivig for patients with Ivig-Resistant Kawasaki disease. J. Immunol. Res. 2020, 4175821 (2020).
Eleftheriou, D. et al. Takayasu Arteritis in childhood: retrospective experience from a tertiary referral centre in the United Kingdom. Arthritis Res. Ther. 17, 36 (2015).
Sener, S. et al. Treatment of childhood-onset Takayasu Arteritis: switching between Anti-Tnf and Anti-Il-6 Agents. Rheumatology61, 4885–4891 (2022).
Aeschlimann, F. A. et al. Childhood Takayasu Arteritis: disease course and response to therapy. Arthritis Res. Ther. 19, 255 (2017).
Stern, S. et al. Treatment of Pediatric Takayasu Arteritis with Infliximab and cyclophosphamide: experience from an American-Brazilian Cohort Study. J. Clin. Rheumatol. 20, 183–188 (2014).
Funding
This study was supported by Beijing Research Ward Excellence Program (BRWEP2024W102100100).
Author information
Authors and Affiliations
Contributions
Y.X., C.W., X.L., and J.L. conceived the study. M.K., J.Z., F.L., B.H., W.C., L.W., X.Z., G.S., D.Z., T.Y, and M.L. contributed to patient management. Y.X. and J.L. supervised patient management. YT and ML collected data. Y.X., C.W., and W.N. contributed to methodology. C.W. and W.N. performed the data analysis. Y.X. and C.W. wrote the first draft of the manuscript. X.L. and J.L. critically revised the manuscript. All the authors approved the final version of the manuscript submitted for publication and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This study was approved by the Ethics Committee of the Capital Institute of Pediatrics (SHERLLM 2021051). Written informed consents obtained from patients or guardians.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, Y., Wang, C., Niu, W. et al. Age specific clinical manifestations and vascular involvements in childhood-onset Takayasu arteritis. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04424-z
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04424-z
This article is cited by
-
Advancing the understanding of age-specific phenotypes in childhood-onset takayasu arteritis
Pediatric Research (2025)