Abstract
Background
Liraglutide, an analog of glucagon-like peptide-1, is prescribed for managing weight in obese people. This meta-analysis investigated whether liraglutide was suitable for younger children with obesity, and to evaluate the efficacy and safety of varying treatment durations and dosage regimens.
Methods
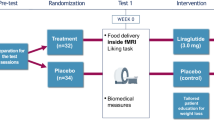
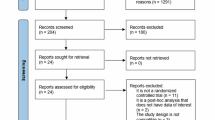
Randomized controlled trials published up to March 20, 2025 were retrieved from in PubMed, Embase, Scopus, Cochrane library, Web of Science, and Google Scholar.
Results
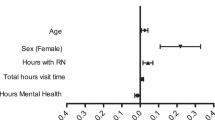
Seven trials involving 575 patients were included in the analysis. Liraglutide significantly decreased body mass index (BMI) (WMD: −0.57; P = 0.007), BMI z-score (WMD: −0.45; P < 0.00001), body weight (WMD: −0.31; P = 0.0004), HbA1c (WMD: −0.43; P = 0.004), fasting plasma glucose (WMD: −1.23; P = 0.003) and systolic blood pressure (WMD: −0.20; P = 0.03) compared with placebos in obese children and adolescents. Subgroup analyses found that children 6–12 years of age did not have a significantly different BMI z-score (z = 1.76; P = 0.08) and body weight (z = 1.75; P = 0.08) versus adolescents. Fifty-six weeks of liraglutide treatment (z = 4.60; P < 0.00001) significantly reduced the BMI z-score versus the short-term treatment group (<13 weeks) (z = 1.20; P = 0.23).
Conclusion
Liraglutide was an effective and safe option for managing overweight and obesity in children and adolescents. Liraglutide was more suitable for adolescents and is endorsed for long-term use.
Impact
-
This is the first meta-analysis to explore the suitability of liraglutide for younger children with obesity and to evaluate its efficacy and safety across varying treatment durations and dosage regimens.
-
Earlier meta-analyses did not include children under 12 years, and neither dosage nor treatment duration was specifically addressed.
-
Our result shows liraglutide is an effective and safe option for managing overweight and obesity in children and adolescents aged 6 to 18 years. Liraglutide was more suitable for adolescents and is endorsed for long-term use.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All analyzed datasets are provided in the article and supplemental materials. Reasonable requests for original materials can be made to the corresponding author.
References
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 390, 2627–2642 (2017).
GBD 2015 Obesity Collaborators et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 377, 13–27 (2017).
Shaban Mohamed, M. A. et al. Risk Factors, Clinical Consequences, Prevention, and Treatment of Childhood Obesity. Child. (Basel) 9, 1975 (2022).
Thompson, D. R. et al. Childhood overweight and cardiovascular disease risk factors: the National Heart, Lung, and Blood Institute Growth and Health Study. J. Pediatr. 150, 18–25 (2007).
Kelly, A. S., Armstrong, S. C., Michalsky, M. P. & Fox, C. K. Obesity in Adolescents: A Review. JAMA 332, 738–748 (2024).
Hampl, S. E. et al. Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents With Obesity. Pediatrics 151, e2022060640 (2023).
Jepsen, M. M. & Christensen, M. B. Emerging glucagon-like peptide 1 receptor agonists for the treatment of obesity. Expert. Opin. Emerg. Drugs 26, 231–243 (2021).
Wiegand, S. et al. Predicting weight loss and maintenance in overweight/obese pediatric patients. Horm. Res. Paediatr. 82, 380–387 (2014).
Preventive Services Task Force, U. S. et al. Screening for Obesity in Children and Adolescents: US Preventive Services Task Force Recommendation Statement. JAMA 317, 2417–2426 (2017).
Danielsson, P., Kowalski, J., Ekblom, Ö & Marcus, C. Response of severely obese children and adolescents to behavioral treatment. Arch. Pediatr. Adolesc. Med. 166, 1103–1108 (2012).
Nicolucci, A. & Maffeis, C. The adolescent with obesity: what perspectives for treatment?. Ital. J. Pediatr. 48, 9 (2022).
Bensignor, M. O., Kelly, A. S. & Arslanian, S. Anti-obesity pharmacotherapy for treatment of pediatric type 2 diabetes: Review of the literature and lessons learned from adults. Front Endocrinol. (Lausanne) 13, 1043650 (2022).
Mastrandrea, L. D. et al. Liraglutide effects in a paediatric (7-11 y) population with obesity: A randomized, double-blind, placebo-controlled, short-term trial to assess safety, tolerability, pharmacokinetics, and pharmacodynamics. Pediatr. Obes. 14, e12495 (2019).
Fox, C. K. et al. Liraglutide for Children 6 to <12 Years of Age with Obesity — A Randomized Trial. N. Engl. J. Med. 392, 555–565 (2025).
Cornejo-Estrada, A. et al. Efficacy of Liraglutide in Obesity in Children and Adolescents: Systematic Review and Meta-Analysis of Randomized Controlled Trials. Child. (Basel) 10, 208 (2023).
Gou, H., Zhai, Y. & Guo, J. Efficacy and safety of liraglutide for weight management in children and adolescents: a systematic review and meta-analysis of randomized controlled trials. Eur. J. Pediatr. 182, 5095–5108 (2023).
Higgins, J. P. T. et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343, d5928 (2011).
Guyatt, G. H. et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336, 924–926 (2008).
Kelly, A. S. et al. A Randomized, Controlled Trial of Liraglutide for Adolescents with Obesity. N. Engl. J. Med. 382, 2117–2128 (2020).
Tamborlane, W. V. et al. Liraglutide in Children and Adolescents with Type 2 Diabetes. N. Engl. J. Med. 381, 637–646 (2019).
Danne, T. et al. Liraglutide in an Adolescent Population with Obesity: A Randomized, Double-Blind, Placebo-Controlled 5-Week Trial to Assess Safety, Tolerability, and Pharmacokinetics of Liraglutide in Adolescents Aged 12-17 Years. J. Pediatrics 181, 146–153.e3 (2017).
Zhou Q. X., Wang, Z. Y., Zhao, H. F. & Wang, S. The effects of GLP-1 analogues on pre-diabetes of the children. Exp. Ther. Med. 13, 1426–1430 (2017).
Klein, D. J. et al. Liraglutide’s Safety, Tolerability, Pharmacokinetics, and Pharmacodynamics in Pediatric Type 2 Diabetes: A Randomized, Double-Blind, Placebo-Controlled Trial. Diabetes Technol. Therapeutics 16, 679–687 (2014).
Drozdz, D. et al. Obesity and Cardiometabolic Risk Factors: From Childhood to Adulthood. Nutrients 13, 4176 (2021).
Vanderwall, C., Randall Clark, R., Eickhoff, J. & Carrel, A. L. BMI is a poor predictor of adiposity in young overweight and obese children. BMC Pediatr. 17, 135 (2017).
Drucker, D. J. & Nauck, M. A. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet 368, 1696–1705 (2006).
Geserick, M. et al. Acceleration of BMI in Early Childhood and Risk of Sustained Obesity. N. Engl. J. Med. 379, 1303–1312 (2018).
Veldhuis, J. D. et al. Endocrine control of body composition in infancy, childhood, and puberty. Endocr. Rev. 26, 114–146 (2005).
Fox, C. K., Kelly, A. S., Reilly, J. L., Theis-Mahon, N. & Raatz, S. J. Current and future state of pharmacological management of pediatric obesity. Int. J. Obes. https://doi.org/10.1038/s41366-024-01465-y (2024).
Kelly, A. S. Current and future pharmacotherapies for obesity in children and adolescents. Nat. Rev. Endocrinol. 19, 534–541 (2023).
Stefater-Richards, M. A., Jhe, G. & Zhang, Y. J. GLP-1 Receptor Agonists in Pediatric and Adolescent Obesity. Pediatrics 155, e2024068119 (2025).
Perry, C., Guillory, T. S. & Dilks, S. S. Obesity and Psychiatric Disorders. Nurs. Clin. North. Am. 56, 553–563 (2021).
Abdelkawy, Y. S., Elharoun, M., Sheta, E., Abdel-Raheem, I. T. & Nematalla, H. A. Liraglutide and Naringenin relieve depressive symptoms in mice by enhancing Neurogenesis and reducing inflammation. Eur. J. Pharmacol. 971, 176525 (2024).
Mansur, R. B. et al. Liraglutide promotes improvements in objective measures of cognitive dysfunction in individuals with mood disorders: A pilot, open-label study. J. Affect. Disord. 207, 114–120 (2017).
Acknowledgements
We are grateful to Dr Liu for helpful comments on a draft version of this manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by [Jiayue Dong], [Meilin Liu], and [Zhanli Liu]. The first draft of the manuscript was written by [Jiayue Dong,] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dong, J., Liu, M. & Liu, Z. Long-term administration of liraglutide for weight management in pediatric patients under 18 years: evidence from 7 randomized controlled trials. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04537-5
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04537-5