Abstract
Diastolic function, the combined effect of myocardial relaxation, recoil forces, stiffness and atrial function, describes the ability of the ventricle to fill up with blood and prepare a stroke volume for ejection. Diastolic dysfunction (DD), also described as ‘an increased resistance to filling’ for example due to impaired relaxation, chamber stiffness, volume load or pericardial restraint, is a situation whereby normal filling is only achieved with elevated filling pressure and higher atrial pressure. Diastolic dysfunction can progress to diastolic heart failure, a clinical syndrome with respiratory deterioration and/or edema and is associated with morbidity and mortality. Diastolic dysfunction can be diagnosed with a multi-modal multi-parameter echocardiography approach, but further development of newborn specific diagnostic algorithms is required. Diastolic dysfunction often precedes systolic dysfunction and thus provides an opportunity for management directives in newborns at high risk of heart failure: with a patent ductus arteriosus, septic shock, pulmonary hypertension, congenital diaphragmatic hernia, small for gestational age infants and infants with bronchopulmonary dysplasia. This review describes the current understanding of the physiology and pathophysiology of diastolic function in newborn infants.
Impact
-
Diastolic dysfunction is common in the neonatal intensive care and can lead to diastolic heart failure.
-
Understanding pathophysiology and clinical relevance allows for targeted treatments and supportive care.
-
Improved cardiovascular care during a crucial part of development can improve short- and long-term outcomes and limit early heart failure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Nagueh, S. F. Left Ventricular Diastolic Function. Underst. Pathophysiol., Diagnosis, Prognosis Echocardiogr. JACC Cardiovasc Imaging 13, 228–244, https://doi.org/10.1016/j.jcmg.2018.10.038 (2020).
Mekkaoui, C. et al. Diffusion MRI tractography of the developing human fetal heart. PLoS One 8, e72795, https://doi.org/10.1371/journal.pone.0072795 (2013).
Bensley, J. G., Moore, L., De Matteo, R., Harding, R. & Black, M. J. Impact of preterm birth on the developing myocardium of the neonate. Pediatr. Res 83, 880–888, https://doi.org/10.1038/pr.2017.324 (2018).
Lahmers, S., Wu, Y., Call, D. R., Labeit, S. & Granzier, H. Developmental control of titin isoform expression and passive stiffness in fetal and neonatal myocardium. Circ. Res 94, 505–513, https://doi.org/10.1161/01.res.0000115522.52554.86 (2004).
Sørensen K. et al. Changes in left ventricular diastolic flow dynamics in the neonatal transition period and beyond. Am. J. Physiol. Heart Circ. Physiol. 8, https://doi.org/10.1152/ajpheart.00214.2025 (2025).
Pfeffer, M. A., Shah, A. M. & Borlaug, B. A. Heart Failure With Preserved Ejection Fraction In Perspective. Circ. Res 124, 1598–1617, https://doi.org/10.1161/circresaha.119.313572 (2019).
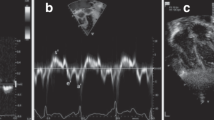
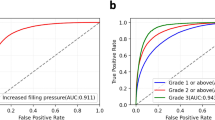
de Waal, K., Phad, N. & Crendal, E. Echocardiography algorithms to assess high left atrial pressure and grade diastolic function in preterm infants. Echocardiography 40, 1099–1106, https://doi.org/10.1111/echo.15686 (2023).
de Waal, K., Costley, N., Phad, N. & Crendal, E. Left Ventricular Diastolic Dysfunction and Diastolic Heart Failure in Preterm Infants. Pediatr. Cardiol. 40, 1709–1715, https://doi.org/10.1007/s00246-019-02208-x (2019).
Kharrat, A., Nissimov, S., Zhu, F., Deshpande, P. & Jain, A. Cardiopulmonary Physiology of Hypoxemic Respiratory Failure Among Preterm Infants with Septic Shock. J. Pediatr. 278, 114384. https://doi.org/10.1016/j.jpeds.2024.114384 (2024).
Nayak, V. et al. Subclinical myocardial dysfunction among fetal growth restriction neonates: a case-control study. J. Matern Fetal Neonatal Med 37, 2392783. https://doi.org/10.1080/14767058.2024.2392783 (2024).
Fouzas, S. et al. Neonatal cardiac dysfunction in intrauterine growth restriction. Pediatr. Res 75, 651–657, https://doi.org/10.1038/pr.2014.22 (2014).
Rigotti, C., Doni, D., Zannin, E., Abdelfattah, A. S. & Ventura, M. L. Left ventricular diastolic function and respiratory outcomes in preterm infants: a retrospective study. Pediatr. Res 93, 1010–1016, https://doi.org/10.1038/s41390-022-02216-3 (2023).
Muhsen, W., Nestaas, E., Hosking, J. & Latour, J. M. Echocardiography parameters used in identifying right ventricle dysfunction in preterm infants with early bronchopulmonary dysplasia: A scoping review. Front Pediatr. 11, 1114587. https://doi.org/10.3389/fped.2023.1114587 (2023).
Altit, G. et al. Altered biventricular function in neonatal hypoxic-ischaemic encephalopathy: a case-control echocardiographic study. Cardiol. Young-. 33, 1587–1596, https://doi.org/10.1017/s1047951122002839 (2023).
Patel, N., Massolo, A. C. & Kipfmueller, F. Congenital diaphragmatic hernia-associated cardiac dysfunction. Semin Perinatol. 44, 151168. https://doi.org/10.1053/j.semperi.2019.07.007 (2020).
Burkett D. A. et al. Impact of Pulmonary Hemodynamics and Ventricular Interdependence on Left Ventricular Diastolic Function in Children With Pulmonary Hypertension. Circ Cardiovasc. Imaging. 9, https://doi.org/10.1161/circimaging.116.004612 (2016).
Friedberg, M. K. et al. Left ventricular diastolic mechanical dyssynchrony and associated clinical outcomes in children with dilated cardiomyopathy. Circ. Cardiovasc Imaging 1, 50–57, https://doi.org/10.1161/circimaging.108.782086 (2008).
Heidenreich, P. A. et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 145, e895–e1032, https://doi.org/10.1161/cir.0000000000001063 (2022).
Hsu, D. T. & Pearson, G. D. Heart failure in children: part I: history, etiology, and pathophysiology. Circ. Heart Fail 2, 63–70, https://doi.org/10.1161/circheartfailure.108.820217 (2009).
Ross, R. D. The Ross classification for heart failure in children after 25 years: a review and an age-stratified revision. Pediatr. Cardiol. 33, 1295–1300, https://doi.org/10.1007/s00246-012-0306-8 (2012).
de Waal, K. et al. The association between patterns of early respiratory disease and diastolic dysfunction in preterm infants. J. Perinatol.: Off. J. Calif. Perinat. Assoc. 43, 1268–1273, https://doi.org/10.1038/s41372-023-01608-5 (2023).
Nguyen, M. B. et al. Understanding Complex Interactions in Pediatric Diastolic Function Assessment. J. Am. Soc. Echocardiogr. 35, 868–877.e5, https://doi.org/10.1016/j.echo.2022.03.017 (2022).
Kellenberger, C. J., Lovrenski, J., Semple, T. & Caro-Domínguez, P. Neonatal cardiorespiratory imaging-a multimodality state-of-the-art review. Pediatr. Radio. 53, 660–676 https://doi.org/10.1007/s00247-022-05504-6 (2023).
Schmitz, L., Koch, H., Bein, G. & Brockmeier, K. Left ventricular diastolic function in infants, children, and adolescents. Reference values and analysis of morphologic and physiologic determinants of echocardiographic Doppler flow signals during growth and maturation. J. Am. Coll. Cardiol. 32, 1441–1448, https://doi.org/10.1016/s0735-1097(98)00379-9 (1998).
Schmitz, L., Stiller, B., Koch, H., Koehne, P. & Lange, P. Diastolic left ventricular function in preterm infants with a patent ductus arteriosus: a serial Doppler echocardiography study. Early Hum. Dev. 76, 91–100 (2004).
Schmitz, L., Xanthopoulos, A., Koch, H. & Lange, P. E. Doppler flow parameters of left ventricular filling in infants: how long does it take for the maturation of the diastolic function in a normal left ventricle to occur? Pediatr. Cardiol. 25, 482–491, https://doi.org/10.1007/s00246-003-0605-1 (2004).
Schmitz, L., Xanthopoulos, A. & Lange, P. E. Isovolumic relaxation time shortens significantly during the three months after birth. J. Am. Soc. Echocardiogr. 17, 275–276, https://doi.org/10.1016/j.echo.2003.10.027 (2004).
Bussmann, N. et al. Early diastolic dysfunction and respiratory morbidity in premature infants: an observational study. J. Perinatol.: Off. J. Calif. Perinat. Assoc. 38, 1205–1211, https://doi.org/10.1038/s41372-018-0147-2 (2018).
Ciccone, M. M. et al. Different functional cardiac characteristics observed in term/preterm neonates by echocardiography and tissue doppler imaging. Early Hum. Dev. 87, 555–558, https://doi.org/10.1016/j.earlhumdev.2011.04.012 (2011).
Bokiniec, R., Własienko, P., Szymkiewicz-Dangel, J. & Borszewska-Kornacka, M. K. Doppler tissue imaging assessment of myocardial velocities and atrioventricular time intervals in term newborn infants during the neonatal period. Kardiol. Pol. 71, 1154–1160, https://doi.org/10.5603/kp.2013.0296 (2013).
Petoello, E., Kerkow, E., Phad, N., Ficial, B. & de Waal, K. Which left atrial volume measurement should we use in the neonatal intensive care? Early Hum. Dev. 191, 105985. https://doi.org/10.1016/j.earlhumdev.2024.105985 (2024).
Agata, Y. et al. Changes in pulmonary venous flow pattern during early neonatal life. Br. Heart J. 71, 182–186, https://doi.org/10.1136/hrt.71.2.182 (1994).
Hong, Y. M. & Choi, J. Y. Pulmonary venous flow from fetal to neonatal period. Early Hum. Dev. 57, 95–103, https://doi.org/10.1016/s0378-3782(99)00058-4 (2000).
Erickson, C. T. et al. Progression of left ventricular diastolic function in the neonate and early childhood from transmitral color M-mode filling analysis. Pediatr. Res 89, 987–995, https://doi.org/10.1038/s41390-020-1011-6 (2021).
de Waal, K., Petoello, E., Crendal, E. & Phad, N. Reference ranges of left ventricular diastolic multimodal ultrasound parameters in stable preterm infants in the early and late neonatal intensive care admission period. J. Perinatol. https://doi.org/10.1038/s41372-025-02278-1 (2025).
James, A., Corcoran, J. D., Mertens, L., Franklin, O. & El-Khuffash, A. Left Ventricular Rotational Mechanics in Preterm Infants Less Than 29 Weeks’ Gestation over the First Week after Birth. J. Am. Soc. Echocardiogr. 28, 808–17.e1, https://doi.org/10.1016/j.echo.2015.02.015 (2015).
Smith, A. et al. Comparison of left ventricular rotational mechanics between term and extremely premature infants over the first week of age. Open Heart. 8, https://doi.org/10.1136/openhrt-2020-001458 (2021).
Mourani, P. M. et al. Early pulmonary vascular disease in preterm infants at risk for bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med 191, 87–95, https://doi.org/10.1164/rccm.201409-1594OC (2015).
Das, B. et al. Heart Failure with Preserved Ejection Fraction in Children. Pediatr. Cardiol. 44, 513–529, https://doi.org/10.1007/s00246-022-02960-7 (2023).
Bohn, M. K. et al. Cardiac Biomarkers in Pediatrics: An Undervalued Resource. Clin. Chem. 67, 947–958, https://doi.org/10.1093/clinchem/hvab063 (2021).
Nagueh, S. F. et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur. J. Echocardiogr. 10, 165–193, https://doi.org/10.1093/ejechocard/jep007 (2009).
Nagueh, S. F. et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 29, 277–314, https://doi.org/10.1016/j.echo.2016.01.011 (2016).
Ficial, B. et al. Feasibility, Reproducibility and Reference Ranges of Left Atrial Strain in Preterm and Term Neonates in the First 48 h of Life. Diagnostics (Basel). 12, https://doi.org/10.3390/diagnostics12020350 (2022).
Jain, A. et al. Left Ventricular Function in Healthy Term Neonates During the Transitional Period. J Pediatr. 28,https://doi.org/10.1016/j.jpeds.2016.11.003 (2016).
Kozak-Barany, A., Jokinen, E., Saraste, M., Tuominen, J. & Valimaki, I. Development of left ventricular systolic and diastolic function in preterm infants during the first month of life: a prospective follow-up study. J. Pediatr. 139, 539–545, https://doi.org/10.1067/mpd.2001.118199 (2001).
de Waal, K., Phad, N. & Boyle, A. Left atrium function and deformation in very preterm infants with and without volume load. Echocardiography 35, 1818–1826, https://doi.org/10.1111/echo.14140 (2018).
Di Maria, M. V. et al. Maturational Changes in Diastolic Longitudinal Myocardial Velocity in Preterm Infants. J. Am. Soc. Echocardiogr. 28, 1045–1052, https://doi.org/10.1016/j.echo.2015.04.016 (2015).
Hirose, A. et al. Evolution of left ventricular function in the preterm infant. J. Am. Soc. Echocardiogr. 28, 302–308, https://doi.org/10.1016/j.echo.2014.10.017 (2015).
de Waal, K. et al. The association between patterns of early respiratory disease and diastolic dysfunction in preterm infants. J. Perinatol. 23, https://doi.org/10.1038/s41372-023-01608-5 (2023).
Harada, K., Takahashi, Y., Tamura, M., Orino, T. & Takada, G. Serial echocardiographic and Doppler evaluation of left ventricular systolic performance and diastolic filling in premature infants. Early Hum. Dev. 54, 169–180, https://doi.org/10.1016/s0378-3782(98)00093-0 (1999).
Sirc, J., Dempsey, E. M. & Miletin, J. Diastolic ventricular function improves during the first 48-hours-of-life in infants weighting <1250 g. Acta Paediatr. 104, e1–e6, https://doi.org/10.1111/apa.12788 (2015).
Ficial, B. et al. Left atrial strain assessment unveils left ventricular diastolic dysfunction in neonates with transient tachypnea of the newborn: A prospective observational study. Pediatr. Pulmonol. 59, 2910–2921, https://doi.org/10.1002/ppul.27156 (2024).
Matsuda, M., Anderson-Morris, J. & Raj, J. U. Microvascular pressures in isolated perfused immature lamb lungs: effects of flow rate, left atrial pressure and surfactant therapy. Biol. Neonate 70, 349–358, https://doi.org/10.1159/000244386 (1996).
Scholl, J. E. & Yanowitz, T. D. Pulmonary hemorrhage in very low birth weight infants: a case-control analysis. J. Pediatr. 166, 1083–1084, https://doi.org/10.1016/j.jpeds.2014.12.032 (2015).
Kappico, J. M. et al. Pulmonary hemorrhage in extremely low birth weight infants: Significance of the size of left to right shunting through a valve incompetent patent foramen ovale. J. Perinatol. 42, 1233–1237, https://doi.org/10.1038/s41372-022-01464-9 (2022).
Eriksen, B. H. et al. Myocardial function in premature infants: a longitudinal observational study. BMJ Open. 3, https://doi.org/10.1136/bmjopen-2012-002441 (2013).
Helfer, S., Schmitz, L., Buhrer, C. & Czernik, C. Tissue Doppler-derived strain and strain rate during the first 28 days of life in very low birth weight infants. Echocardiography 31, 765–772, https://doi.org/10.1111/echo.12463 (2014).
James, A. T. et al. Assessment of myocardial performance in preterm infants less than 29 weeks gestation during the transitional period. Early Hum. Dev. 90, 829–835, https://doi.org/10.1016/j.earlhumdev.2014.09.004 (2014).
Lee, A. et al. Tissue Doppler imaging in very preterm infants during the first 24 h of life: an observational study. Arch. Dis. Child Fetal Neonatal Ed. 99, F64–F69, https://doi.org/10.1136/archdischild-2013-304197 (2014).
Saleemi, M. S., El-Khuffash, A., Franklin, O. & Corcoran, J. D. Serial changes in myocardial function in preterm infants over a four week period: the effect of gestational age at birth. Early Hum. Dev. 90, 349–352, https://doi.org/10.1016/j.earlhumdev.2014.04.012 (2014).
de Waal, K., Phad, N., Collins, N. & Boyle, A. Cardiac remodeling in preterm infants with prolonged exposure to a patent ductus arteriosus. Congenit. Heart Dis. 12, 364–372, https://doi.org/10.1111/chd.12454 (2017).
Friedberg, M. K., Silverman, N. H., Dubin, A. M. & Rosenthal, D. N. Mechanical dyssynchrony in children with systolic dysfunction secondary to cardiomyopathy: a Doppler tissue and vector velocity imaging study. J. Am. Soc. Echocardiogr. 20, 756–763, https://doi.org/10.1016/j.echo.2006.11.007 (2007).
de Waal, K., Crendal, E. & Boyle, A. Left ventricular vortex formation in preterm infants assessed by blood speckle imaging. Echocardiography 36, 1364–1371, https://doi.org/10.1111/echo.14391 (2019).
Dikshit, K. et al. Renal and extrarenal hemodynamic effects of furosemide in congestive heart failure after acute myocardial infarction. N. Engl. J. Med 288, 1087–1090, https://doi.org/10.1056/nejm197305242882102 (1973).
Romero-Lopez, M. et al. The effect of furosemide on extremely premature infants treated with nonsteroidal anti-inflammatory drugs for persistent patent ductus arteriosus. J. Perinatol. 45, 399–401, https://doi.org/10.1038/s41372-024-02148-2 (2025).
Huang, X., Dorhout Mees, E., Vos, P., Hamza, S. & Braam, B. Everything we always wanted to know about furosemide but were afraid to ask. Am. J. Physiol. Ren. Physiol. 310, F958–F971, https://doi.org/10.1152/ajprenal.00476.2015 (2016).
El-Khuffash, A. F., Jain, A. & McNamara, P. J. Ligation of the patent ductus arteriosus in preterm infants: understanding the physiology. J. Pediatr. 162, 1100–1106, https://doi.org/10.1016/j.jpeds.2012.12.094 (2013).
Bischoff, A. R. et al. Left ventricular function before and after percutaneous patent ductus arteriosus closure in preterm infants. Pediatr. Res 94, 213–221, https://doi.org/10.1038/s41390-022-02372-6 (2023).
Bischoff, A. R. et al. Cardiorespiratory Instability after Percutaneous Patent Ductus Arteriosus Closure: A Multicenter Cohort Study. J. Pediatr. 271, 114052. https://doi.org/10.1016/j.jpeds.2024.114052 (2024).
Villamor, E. et al. Patent Ductus Arteriosus and Bronchopulmonary Dysplasia-Associated Pulmonary Hypertension: A Bayesian Meta-Analysis. JAMA Netw. Open 6, e2345299, https://doi.org/10.1001/jamanetworkopen.2023.45299 (2023).
Islam, J. Y., Keller, R. L., Aschner, J. L., Hartert, T. V. & Moore, P. E. Understanding the Short- and Long-Term Respiratory Outcomes of Prematurity and Bronchopulmonary Dysplasia. Am. J. Respir. Crit. Care Med 192, 134–156, https://doi.org/10.1164/rccm.201412-2142PP (2015).
Varghese, N. P., Altit, G., Gubichuk, M. M. & Siddaiah, R. Navigating Diagnostic and Treatment Challenges of Pulmonary Hypertension in Infants with Bronchopulmonary Dysplasia. J. Clin. Med. 13, https://doi.org/10.3390/jcm13123417 (2024).
Sehgal, A., South, A. M. & Menahem, S. Systemic hemodynamics and pediatric lung disease: mechanistic links and therapeutic relevance. Am. J. Physiol. Heart Circ. Physiol. 327, H454–H459, https://doi.org/10.1152/ajpheart.00271.2024 (2024).
Gopagondanahalli, K. R. et al. Characterizing the Role of Left Ventricular Indices and Biventricular Interaction in Bronchopulmonary Dysplasia-Associated Pulmonary Hypertension in Extreme Prematurity. Neonatology 122, 210–221, https://doi.org/10.1159/000542980 (2025).
Sullivan, R. T. et al. Role of left atrial hypertension in pulmonary hypertension associated with bronchopulmonary dysplasia. Front Pediatr. 10, 1012136. https://doi.org/10.3389/fped.2022.1012136 (2022).
Bokiniec, R., Wlasienko, P., Borszewska-Kornacka, M. & Szymkiewicz-Dangel, J. Evaluation of left ventricular function in preterm infants with bronchopulmonary dysplasia using various echocardiographic techniques. Echocardiography 34, 567–576, https://doi.org/10.1111/echo.13488 (2017).
Greer, J. Pathophysiology of cardiovascular dysfunction in sepsis. BJA Educ. 15, 316–321, https://doi.org/10.1093/bjaceaccp/mkv003 (2015).
Sanfilippo, F. et al. Diastolic dysfunction and mortality in septic patients: a systematic review and meta-analysis. Intensive Care Med 41, 1004–1013, https://doi.org/10.1007/s00134-015-3748-7 (2015).
Sanfilippo, F. et al. Echocardiographic Parameters and Mortality in Pediatric Sepsis: A Systematic Review and Meta-Analysis. Pediatr. Crit. Care Med 22, 251–261, https://doi.org/10.1097/pcc.0000000000002622 (2021).
Kharrat, A. & Jain, A. Hemodynamic dysfunction in neonatal sepsis. Pediatr. Res 91, 413–424, https://doi.org/10.1038/s41390-021-01855-2 (2022).
Gorantiwar, S. & de Waal, K. Progression from sepsis to septic shock and time to treatments in preterm infants with late-onset sepsis. J. Paediatr. Child Health 57, 1905–1911, https://doi.org/10.1111/jpc.15606 (2021).
Johnston, N. & de Waal, K. Clinical and haemodynamic characteristics of preterm infants with early onset sepsis. J. Paediatr. Child Health 58, 2267–2272, https://doi.org/10.1111/jpc.16218 (2022).
de Waal, K. & Petoello, E. Assessing fluid responsiveness with ultrasound in the neonatal intensive care setting: the mini-fluid challenge. Eur. J. Pediatr. 183, 1947–1951, https://doi.org/10.1007/s00431-024-05425-6 (2024).
Bidegain, M. et al. Vasopressin for refractory hypotension in extremely low birth weight infants. J. Pediatr. 157, 502–504, https://doi.org/10.1016/j.jpeds.2010.04.038 (2010).
Nestaas, E. & Walsh, B. H. Hypothermia and Cardiovascular Instability. Clin. Perinatol. 47, 575–592, https://doi.org/10.1016/j.clp.2020.05.012 (2020).
Giesinger, R. E., Bailey, L. J., Deshpande, P. & McNamara, P. J. Hypoxic-Ischemic Encephalopathy and Therapeutic Hypothermia: The Hemodynamic Perspective. J. Pediatr. 180, 22–30.e2, https://doi.org/10.1016/j.jpeds.2016.09.009 (2017).
Sehgal, A., Linduska, N. & Huynh, C. Cardiac adaptation in asphyxiated infants treated with therapeutic hypothermia. J. Neonatal Perinat. Med 12, 117–125, https://doi.org/10.3233/npm-1853 (2019).
Post, H. et al. Cardiac function during mild hypothermia in pigs: increased inotropy at the expense of diastolic dysfunction. Acta Physiol. (Oxf.) 199, 43–52, https://doi.org/10.1111/j.1748-1716.2010.02083.x (2010).
Rodriguez, M. J., Martinez-Orgado, J., Corredera, A., Serrano, I. & Arruza, L. Diastolic Dysfunction in Neonates With Hypoxic-Ischemic Encephalopathy During Therapeutic Hypothermia: A Tissue Doppler Study. Front Pediatr. 10, 880786. https://doi.org/10.3389/fped.2022.880786 (2022).
Kumagai, T. et al. Correlation between echocardiographic superior vena cava flow and short-term outcome in infants with asphyxia. Early Hum. Dev. 89, 307–310, https://doi.org/10.1016/j.earlhumdev.2012.10.011 (2013).
Gebauer, C. M., Knuepfer, M., Robel-Tillig, E., Pulzer, F. & Vogtmann, C. Hemodynamics among neonates with hypoxic-ischemic encephalopathy during whole-body hypothermia and passive rewarming. Pediatrics 117, 843–850, https://doi.org/10.1542/peds.2004-1587 (2006).
Konstam, M. A. et al. Evaluation and Management of Right-Sided Heart Failure: A Scientific Statement From the American Heart Association. Circulation 137, e578–e622, https://doi.org/10.1161/CIR.0000000000000560 (2018).
Hsia, H. H. & Haddad, F. Pulmonary hypertension: a stage for ventricular interdependence?. J. Am. Coll. Cardiol. 59, 2203–2205, https://doi.org/10.1016/j.jacc.2011.12.049 (2012).
Jayasekera, G. et al. Left ventricular dysfunction and intra-ventricular dyssynchrony in idiopathic pulmonary arterial hypertension. Int J. Cardiol. 365, 131–139, https://doi.org/10.1016/j.ijcard.2022.07.032 (2022).
Richter, M. J. et al. Right ventricular dyssynchrony: from load-independent right ventricular function to wall stress in severe pulmonary arterial hypertension. Pulm. Circ. 10, 2045894020925759, https://doi.org/10.1177/2045894020925759 (2020).
Wan, C. et al. Prognostic effect of left ventricular-pulmonary arterial coupling indicator in pulmonary arterial hypertension. Int J. Cardiol. 434, 133347. https://doi.org/10.1016/j.ijcard.2025.133347 (2025).
Zani, A. et al. Congenital diaphragmatic hernia. Nat. Rev. Dis. Prim. 8, 37, https://doi.org/10.1038/s41572-022-00362-w (2022).
Altit, G., Bhombal, S., Van Meurs, K. & Tacy, T. A. Ventricular Performance is Associated with Need for Extracorporeal Membrane Oxygenation in Newborns with Congenital Diaphragmatic Hernia. J. Pediatr. 191, 28–34.e1, https://doi.org/10.1016/j.jpeds.2017.08.060 (2017).
Patel, N. et al. Early Postnatal Ventricular Dysfunction Is Associated with Disease Severity in Patients with Congenital Diaphragmatic Hernia. J. Pediatr. 203, 400–407.e1, https://doi.org/10.1016/j.jpeds.2018.07.062 (2018).
Tydén, K., Mesas Burgos, C., Jonsson, B. & Nordenstam, F. Left atrial strain in neonates with congenital diaphragmatic hernia and length of stay in pediatric intensive care unit. Front Pediatr. 12, 1404350. https://doi.org/10.3389/fped.2024.1404350 (2024).
Altit, G., Lapointe, A., Kipfmueller, F. & Patel, N. Cardiac function in congenital diaphragmatic hernia. Semin Pediatr. Surg. 33, 151438. https://doi.org/10.1016/j.sempedsurg.2024.151438 (2024).
Patel, N., Massolo, A. C., Kraemer, U. S. & Kipfmueller, F. The heart in congenital diaphragmatic hernia: Knowns, unknowns, and future priorities. Front Pediatr. 10, 890422. https://doi.org/10.3389/fped.2022.890422 (2022).
Pugnaloni, F. et al. Early Postnatal Ventricular Disproportion Predicts Outcome in Congenital Diaphragmatic Hernia. Am. J. Respir. Crit. Care Med 208, 325–328, https://doi.org/10.1164/rccm.202212-2306LE (2023).
Stressig, R. et al. Preferential streaming of the ductus venosus toward the right atrium is associated with a worse outcome despite a higher rate of invasive procedures in human fetuses with left diaphragmatic hernia. Ultraschall Med 34, 568–572, https://doi.org/10.1055/s-0032-1330702 (2013).
Massolo, A. C. et al. Ventricular Dysfunction, Interdependence, and Mechanical Dispersion in Newborn Infants with Congenital Diaphragmatic Hernia. Neonatology 116, 68–75, https://doi.org/10.1159/000499347 (2019).
Noh, C. Y. et al. Early nitric oxide is not associated with improved outcomes in congenital diaphragmatic hernia. Pediatr. Res 93, 1899–1906, https://doi.org/10.1038/s41390-023-02491-8 (2023).
Tanaka, T. et al. The evaluation of diastolic function using the diastolic wall strain (DWS) before and after radical surgery for congenital diaphragmatic hernia. Pediatr. Surg. Int 31, 905–910, https://doi.org/10.1007/s00383-015-3766-0 (2015).
Patel, N. & Kipfmueller, F. Cardiac dysfunction in congenital diaphragmatic hernia: Pathophysiology, clinical assessment, and management. Semin Pediatr. Surg. 26, 154–158, https://doi.org/10.1053/j.sempedsurg.2017.04.001 (2017).
Sehgal, A., Krishnamurthy, M. B., Clark, M. & Menahem, S. ACE inhibition for severe bronchopulmonary dysplasia - an approach based on physiology. Physiol. Rep. 6, e13821, https://doi.org/10.14814/phy2.13821 (2018).
Kluckow, M., Seri, I. & Evans, N. Functional echocardiography: an emerging clinical tool for the neonatologist. J. Pediatr. 150, 125–130, https://doi.org/10.1016/j.jpeds.2006.10.056 (2007).
Lewandowski, A. J. et al. Preterm heart in adult life: cardiovascular magnetic resonance reveals distinct differences in left ventricular mass, geometry, and function. Circulation 127, 197–206, https://doi.org/10.1161/circulationaha.112.126920 (2013).
Phad, N. S., de Waal, K., Holder, C. & Oldmeadow, C. Dilated hypertrophy: a distinct pattern of cardiac remodeling in preterm infants. Pediatr. Res. 87, 146–152, https://doi.org/10.1038/s41390-019-0568-4 (2020).
Lewandowski, A. J. et al. Association of Preterm Birth With Myocardial Fibrosis and Diastolic Dysfunction in Young Adulthood. J. Am. Coll. Cardiol. 78, 683–692, https://doi.org/10.1016/j.jacc.2021.05.053 (2021).
Leeson, P. & Lewandowski, A. J. A New Risk Factor for Early Heart Failure: Preterm Birth. J. Am. Coll. Cardiol. 69, 2643–2645, https://doi.org/10.1016/j.jacc.2017.03.574 (2017).
Author information
Authors and Affiliations
Contributions
Dr. de Waal, Dr. Prelipcean, and Dr. Patel were authors of the original draft of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in studies used in this review.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Waal, K., Prelipcean, I. & Patel, N. Diastolic function in newborn infants: understanding pathophysiology, diagnosis and clinical relevance. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04561-5
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04561-5