Abstract
Background
To characterize hemodynamics in the first 24 h after birth in neonates with severe anemia.
Method
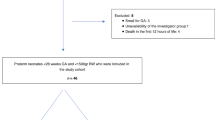
This was a retrospective analysis of data from a prospective cohort from our critically ill neonate database, that included neonates with severe anemia from December 2022 to June 2024. The results obtained from neonates with severe anemia and the control group were compared.
Results
A total of 21 neonates born at 37 [35.00, 38.00] weeks and weighing 2780 [2350, 3200] grams were included. Compared with the control group, we observed lower peak systolic myocardial velocity in biventricular (left: 5.67 [5.43, 6.48] vs. 6.6 [6.12, 7.32], p < 0.001; right: 6.33 [5.81, 7.50] vs. 8.02 [6.74, 8.86], p < 0.001). A greater ratio of the tricuspid valve early inflow velocity/early diastolic myocardial velocity was noted (6.63 [5.92, 9.27] vs. 5.31 [4.67, 6.55], p < 0.001). The peak systolic blood flow of middle cerebral arteries was greater (left: 55.90 [47.10, 64.90] vs. 44.95 [38.20, 50.95], p = 0.008; right: 52.00 [40.88, 56.15] vs. 45.20 [38.00, 52.00], p = 0.048). The lung ultrasound score was 18.00 [13.5, 25.5].
Conclusion
Neonates with severe anemia are characterized by reduced cardiac systolic function, reduced right diastolic function, increased cerebral blood flow, and pulmonary edema during the transition period.
Clinical trial registration
The study was registered in Chinese Clinical Trial Registry (ChiCTR2200065581; https://www.chictr.org.cn/com/25/showproj.aspx?proj=184095).
Impact
-
This study explored hemodynamic characteristics, including cardiac function, blood flow in middle cerebral arteries, and the lung air/fluid ratio, in neonates with early-onset severe anemia and emphasized impaired cardiac systolic and diastolic function and a hypervolemic state in the pulmonary system and brain during the transition period.
-
These hemodynamic changes are more related to the duration of severe anemia than to the severity of anemia.
-
Given the hemodynamic changes in neonates with severe anemia, volume expansion and transfusion should be optimized.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
All the data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
References
Metivier, F., Marchais, S. J., Guerin, A. P., Pannier, B. & London, G. M. Pathophysiology of anaemia: focus on the heart and blood vessels. Nephrol. Dial. Transpl. 15, 14–18 (2000).
Bahr, T. M. et al. Severe anemia at birth-incidence and implications. J. Pediatr. 248, 39–45 e2 (2022).
Christensen, R. D., Bahr, T. M., Tweddell, S. M., Ohls, R. K. & Henry, E. Diagnosing anemia in neonates: an evidence-based approach. Neoreviews 24, e343–e355 (2023).
Kalteren, W. S. et al. Perinatal anemia is associated with neonatal and neurodevelopmental outcomes in infants with moderate to severe perinatal asphyxia. Neonatology 114, 315–322 (2018).
Zonnenberg, I. A. et al. Severe neonatal anaemia, MRI findings and neurodevelopmental outcome. Neonatology 109, 282–288 (2016).
Muraskas, J. K., Kelly, A. F., Nash, M. S., Goodman, J. R. & Morrison, J. C. The role of fetal inflammatory response syndrome and fetal anemia in nonpreventable term neonatal encephalopathy. J. Perinatol. 36, 362–365 (2016).
Widness, J. A. Pathophysiology of anemia during the neonatal period, including anemia of prematurity. Neoreviews 9, e520 (2008).
Suciu, L. M., Prelipcean, I., Fagarasan, A., Giesinger, R. E. & McNamara, P. J. Normative echocardiography data of myocardial adaptation to extrauterine life: a review of prospective studies. Front. Pediatr. 11, 1192618 (2023).
Gijtenbeek, M. et al. Persistent pulmonary hypertension of the newborn after fetomaternal hemorrhage. Transfusion 58, 2819–2824 (2018).
Tongsong, T. et al. Fetal cardiac remodeling in response to anemia: using hemoglobin Bart’s disease as a study model. Ultraschall Med. 41, 186–191 (2020).
Tongprasert, F., Srisupundit, K., Luewan, S. & Tongsong, T. Comparison of cardiac troponin T and N-terminal pro-B-type natriuretic peptide between fetuses with hemoglobin Bart’s disease and nonanemic fetuses. Prenat. Diagn. 34, 864–869 (2014).
Luewan, S., Tongprasert, F., Srisupundit, K. & Tongsong, T. Inferior vena cava Doppler indices in fetuses with hemoglobin Bart’s hydrops fetalis. Prenat. Diagn. 34, 577–580 (2014).
Franz, A. R. et al. Effects of liberal vs restrictive transfusion thresholds on survival and neurocognitive outcomes in extremely low-birth-weight infants: the ETTNO randomized clinical trial. JAMA 324, 560–570 (2020).
Zerra, P. E. & Josephson, C. D. Transfusion in neonatal patients: review of evidence-based guidelines. Clin. Lab Med. 41, 15–34 (2021).
Xiao, T. et al. A study protocol for investigating the sonographic characteristics of neonates with critical illness: an observational cohort study. BMJ Paediatr Open 7 https://doi.org/10.1136/bmjpo-2023-001975 (2023).
Al-Biltagi, M., El Razaky, O. & El Amrousy, D. Cardiac changes in infants of diabetic mothers. World J. Diabetes 12, 1233–1247 (2021).
Dimopoulou, S. et al. Impact of hypertensive disorders of pregnancy on offspring cardiovascular function: from fetal life to early childhood. Ultrasound Obstet. Gynecol. 64, 44–49 (2024).
Huang, W., Liu, D. W. & Wang, X. T. Chinese Critical Ultrasound Study G. Applications of critical ultrasonography in hemodynamic therapy. Chin. Med. J. 134, 1286–1288 (2021).
Matter, M. et al. Myocardial performance in asphyxiated full-term infants assessed by Doppler tissue imaging. Pediatr. Cardiol. 31, 634–642 (2010).
Tao, E. et al. Severe neonatal anemia affected by massive fetomaternal hemorrhage: a single-center retrospective observational study. J. Matern Fetal Neonatal Med. 35, 3972–3978 (2022).
Siwawong, W., Tongprasert, F., Srisupundit, K., Luewan, S. & Tongsong, T. Fetal cardiac circumference derived by spatiotemporal image correlation as a predictor of fetal hemoglobin Bart disease at midpregnancy. J. Ultrasound Med. 32, 1483–1488 (2013).
Leung, K. Y. et al. Ultrasonographic prediction of homozygous alpha0-thalassemia using placental thickness, fetal cardiothoracic ratio and middle cerebral artery Doppler: alone or in combination?. Ultrasound Obstet. Gynecol. 35, 149–154 (2010).
Cambonie, G. et al. Myocardial adaptation to anemia and red blood cell transfusion in premature infants requiring ventilation support in the 1st postnatal week. Neonatology 92, 174–181 (2007).
Hecher, K., Snijders, R., Campbell, S. & Nicolaides, K. Fetal venous, arterial, and intracardiac blood flows in red blood cell isoimmunization. Obstet. Gynecol. 85, 122–128 (1995).
Tongsong, T., Tongprasert, F., Srisupundit, K. & Luewan, S. Venous Doppler studies in low-output and high-output hydrops fetalis. Am. J. Obstet. Gynecol. 203, 488 e1–6 (2010).
Mari, G. et al. Noninvasive diagnosis by Doppler ultrasonography of fetal anemia due to maternal red-cell alloimmunization. Collaborative Group for Doppler Assessment of the Blood Velocity in Anemic Fetuses. N. Engl. J. Med. 342, 9–14 (2000).
Martinez-Portilla, R. J. et al. Performance of fetal middle cerebral artery peak systolic velocity for prediction of anemia in untransfused and transfused fetuses: systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 54, 722–731 (2019).
Raimondi, F. et al. Lung ultrasound score progress in neonatal respiratory distress syndrome. Pediatrics 147 https://doi.org/10.1542/peds.2020-030528 (2021).
Corsini, I. et al. Lung ultrasound scores in neonatal clinical practice: a narrative review of the literature. Pediatr. Pulmonol. 57, 1157–1166 (2022).
Razak, A. & Faden, M. Neonatal lung ultrasonography to evaluate need for surfactant or mechanical ventilation: a systematic review and meta-analysis. Arch. Dis. Child Fetal Neonatal Ed. 105, 164–171 (2020).
Mongodi, S. et al. Quantitative lung ultrasound: technical aspects and clinical applications. Anesthesiology 134, 949–965 (2021).
Stainsby, D. et al. Adverse outcomes of blood transfusion in children: analysis of UK reports to the Serious Hazards of Transfusion scheme 1996-2005. Br. J. Haematol. 141, 73–79 (2008).
Semple, J. W., Rebetz, J. & Kapur, R. Transfusion-associated circulatory overload and transfusion-related acute lung injury. Blood 133, 1840–1853 (2019).
Rashid, N., Al-Sufayan, F., Seshia, M. M. & Baier, R. J. Post transfusion lung injury in the neonatal population. J. Perinatol. 33, 292–296 (2013).
De Cloedt, L. et al. Transfusion-associated circulatory overload in a pediatric intensive care unit: different incidences with different diagnostic criteria. Transfusion 58, 1037–1044 (2018).
Nand, N., Gupta, M. S. & Sharma, M. Furosemide supplemented blood transfusion in cases of chronic severe anemia. Jpn Heart J. 27, 177–182 (1986).
Radicioni, M., Troiani, S. & Mezzetti, D. Functional echocardiographic assessment of myocardial performance in anemic premature infants: a pilot study. Pediatr. Cardiol. 33, 554–561 (2012).
Jain, A. et al. Cardiopulmonary adaptation during first day of life in human neonates. J. Pediatr. 200, 50–57 e2 (2018).
Acknowledgements
We thank all the staff at Neonatal Critical Ultrasound Collaborative Group. Group information of : Pei Zhang, Women and children’s hospital of Hubei province; Li Feng, Sichuan Jinxin xinan women and children’s hospital; Lina Zeng, Pidu People’s Hospital; Longjun Ren, Women and children’s healthcare hospital of Dujiangyan; Min Xi, Kunming children’s hospital; Xiazi Song, Wenzhou women and children’s hospital; Kai Jie, Fangping Zhang, Qingdao women and children’s hospital; Lin Mei, Yaan people’s hospital; Ailing Su, Nanjing women and children’s healthcare hospital; Linrong Mo, The second affiliated hospital of Guilin medical university; Yongjiang Jiang, Guangzhou women and children’s medical center Liuzhou hospital; Meina Lai, Maoming maternal and child health hospital; Ling Xu, Shuangliu women and children’s healthcare hospital; Xiaobo Zeng, Jiangxi maternal and child health hospital; Lijun Zeng, Foshan women and children hospital; Lili, Yin, General hospital of Ningxia medical university; Yu Wang, Northwest women and children’s hospital; Guina Pan, Panyu maternal and child care service centre of Guangzhou; Jian Wang, Zhangzhou municipal hospital of Fujian province; Zhen Tian, Ningxia women and children’s healthcare hospital; Jiping Luo, Xichang people’s hospital; Xiaoyan Ma, Neimenggu women and children’s healthcare hospital; Qingmei Huang, The second affiliated hospital of Guangxi medical university.
Funding
This research is funded by the Chengdu Medical Scientific Research Project 2023010.
Author information
Authors and Affiliations
Contributions
T.X. and R.J. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: T.X., R.J., Y.F., B.L., and J.Z., Acquisition, analysis, or interpretation of data: T.X., R.J., Y.F., B.L., J.Z., X.L., H.L., X.Z., L.Z., L.Z., G.Q., X.Z., M.Z., Y.H., S.G., and X.H. Drafting of the manuscript: Y.F., B.L., and J.Z. Critical review of the manuscript for important intellectual content: T.X., R.J., Y.F., B.L., J.Z., X.L., H.L., X.Z., L.Z., L.Z., G.Q., X.Z., M.Z., Y.H., S.G., and X.H. Statistical analysis: Y.F., B.L., J.Z., X.L., H.L., X.Z., L.Z., L.Z., and G.Q. Administrative, technical, or material support: X.Z., M.Z., Y.H., S.G., and X.H. Supervision: T.X. and R.J.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study involves human participants and was approved by the Research Ethics Committee of the Chengdu Women’s and Children’s Central Hospital (No. 2022(104)). Participants gave informed consent to participate in the study before taking part.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fu, Y., Li, B., Zhang, J. et al. Hemodynamic adaptation in neonates with early-onset severe anemia during transition period. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04574-0
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04574-0