Abstract
Background
Very early onset inflammatory bowel disease presents a rare condition with an enrichment of monogenic disorders. This cohort study aims to investigate the prevalence of IBD-like monogenic disorders as well as genotypic and phenotypic characteristics in an Iranian cohort of VEO-IBD patients.
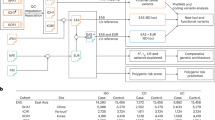
Methods
Patients with VEO-IBD diagnosed between September 2019 and May 2023 were evaluated retrospectively. Clinical data were collected, and whole exome sequencing (WES) was performed on patients. Biological therapy was given to 10 patients (52%), and three underwent intestinal surgery.
Results
Among the 19 patients, 7 (36%) had Crohn’s disease, 3 (15%) had ulcerative colitis, and 9 (47%) had unclassified IBD. Monogenic disorders were identified in 8 patients (42%), including variants in IL10RB, DKC1, FERMT1, GUCY2C, NLRC4, and a susceptibility gene variant in the MEFV gene. We identified a novel heterozygous duplication on chromosome 6 by karyotype and SNP-array analysis but the relevance of the genetic findings remains elusive and further functional testing is required. Four patients were considered for HSCT, and the patient with the MEFV variant responded well to colchicine.
Conclusions
The study revealed that 42% of VEO-IBD patients had underlying monogenic disorders. Early identification of causative mutations is crucial for improving prognosis and treatment strategies.
Impact
-
VEO-IBD is a rare condition with a high prevalence of monogenic disorders. Early detection of causal mutations is crucial for improving prognosis and selecting optimal treatment strategies.
-
In our cohort study, eight patients were found to have five known and three novel pathogenic variants in five different genes. We also identified a de novo duplication of the 6q22 region.
-
Allogeneic HSCT provides a curative treatment for IL-10R-deficient patients, while colchicine treatment resulted in sustained remission in a patient with an MEFV mutation.
-
Our study indicates that early genetic diagnosis of immune-related IBD-like monogenic disorders is essential for effective patient management.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The raw data required to reproduce these findings are available from the corresponding author upon request.
References
Krauthammer, A. et al. Infantile-onset inflammatory bowel disease has variable long-term outcomes. Front. Pediatr. 11, 1097779 (2023).
Kuenzig, M. E. et al. Twenty-first century trends in the global epidemiology of pediatric-onset inflammatory bowel disease: systematic review. J. Pediatr. Gastroenterol. Nutr. 162, 1147–1159.e4 (2023).
De Lange, K. M. et al. Genome-wide association study implicates immune activation of multiple integrin genes in inflammatory bowel disease. Nat. Genet. 49, 256–261 (2017).
Jans, D. & Cleynen, I. The genetics of non-monogenic IBD. Hum. Genet. 142, 669–682 (2023).
Ashton, J. J. et al. Identification of variants in genes associated with single-gene inflammatory bowel disease by whole-exome sequencing. Inflamm. Bowel. Dis. 22, 2317–2327 (2016).
Kammermeier, J. et al. Targeted gene panel sequencing in children with very early onset inflammatory bowel disease—evaluation and prospective analysis. J. Med. Genet. 51, 748–755 (2014).
McGovern, D. P. B., Kugathasan, S. & Cho, J. H. Genetics of inflammatory bowel diseases. Gastroenterology 149, 1163–1176.e2 (2015).
Nambu, R. et al. A systematic review of monogenic inflammatory bowel disease. Clin. Gastroenterol. Hepatol. 20, e653–e663 (2022).
Uhlig, H. H. et al. The diagnostic approach to monogenic very early onset inflammatory bowel disease. Gastroenterology 147, 990–1007.e3 (2014).
Azabdaftari, A., Jones, K. D. J., Kammermeier, J. & Uhlig, H. H. Monogenic inflammatory bowel disease-genetic variants, functional mechanisms and personalized medicine in clinical practice. Hum. Genet. 142, 599–611 (2023).
Uhlig, H. H. et al. Clinical genomics for the diagnosis of monogenic forms of inflammatory bowel disease: a position paper from the pediatric IBD porto group of European Society of Pediatric Gastroenterology, Hepatology and Nutrition. J. Pediatr. Gastroenterol. Nutr. 72, 456–473 (2021).
Kammermeier, J. et al. Genomic diagnosis and care co-ordination for monogenic inflammatory bowel disease in children and adults: consensus guideline on behalf of the British Society of Gastroenterology and British Society of Pediatric Gastroenterology, Hepatology and Nutrition. Lancet Gastroenterol. Hepatol. 8, 271–286 (2023).
O’Connor, C. Karyotyping for chromosomal abnormalities. Nat. Educ. 1, 27 (2008).
Güngör, T. & Chiesa, R. Cellular therapies in chronic granulomatous disease. Front Pediatr. 8, 327 (2020).
Girardelli, M. et al. The diagnostic challenge of very early-onset enterocolitis in an infant with XIAP deficiency. BMC Pediatr. 15, 208 (2015).
Tesi, B. et al. Successful hematopoietic stem cell transplantation in a patient with LPS-responsive beige-like anchor (LRBA) gene mutation. J. Clin. Immunol. 36, 480–489 (2016).
Kotlarz, D. et al. Loss of interleukin-10 signaling and infantile inflammatory bowel disease: implications for diagnosis and therapy. Gastroenterology 143, 347–355 (2012).
Glocker, E. et al. Inflammatory bowel disease and mutations affecting the interleukin-10 receptor. N. Engl. J. Med. 361, 2033–2045 (2009).
Ehlers, L. et al. Treat-to-target strategies for the management of familial Mediterranean Fever in children. Pediatr. Rheumatol. Online J. 21, 108 (2023).
Crowley, E. et al. Prevalence and clinical features of inflammatory bowel diseases associated with monogenic variants, identified by whole-exome sequencing in 1000 children at a single center. Gastroenterology 158, 2208–2220 (2020).
Charbit-Henrion, F. et al. Diagnostic yield of next-generation sequencing in very early-onset inflammatory bowel diseases: a multicenter study. J. Crohns Colitis 12, 1104–1112 (2018).
Zheng, H. B., De La Morena, M. T., Suskind, D. L. The growing need to understand very early onset inflammatory bowel disease. Front Immunol. 12, 675186 (2021).
Eslamian, G. et al. Genomic testing identifies monogenic causes in patients with very early-onset inflammatory bowel disease: a multicenter survey in an Iranian cohort. Clin. Exp. Immunol. 217, 1–11 (2024).
Borggraefe, I. et al. Severe variant of X-linked dyskeratosis congenita (hoyeraal-hreidarsson syndrome) causes significant enterocolitis in early infancy. J. Pediatr. Gastroenterol. Nutr. 49, 359–363 (2009).
Kelsen, J. R. & Sullivan, K. E. Inflammatory bowel disease in primary immunodeficiencies. Curr. Allergy Asthma Rep. 17, 1–15 (2017).
Siegel, D. H. et al. Loss of kindlin-1, a human homolog of the caenorhabditis elegans actin–extracellular-matrix linker protein UNC-112, causes kindler syndrome. Am. J. Hum. Genet 73, 174–187 (2003).
Goult, B. T. et al. The structure of the N-terminus of kindlin-1: a domain important for αiibβ3 integrin activation. J. Mol. Biol. 394, 944–956 (2009).
Shattil, S. J., Kim, C. & Ginsberg, M. H. The final steps of integrin activation: the end game. Nat. Rev. Mol. Cell Biol. 11, 288–300 (2010).
Singh, S., Singh, G., Heim, J. M. & Gerzer, R. Isolation and expression of a guanylate cyclase-coupled heat stable enterotoxin receptor cDNA from a human colonic cell line. Biochem Biophys. Res. Commun. 179, 1455–1463 (1991).
Prasad, H. & Visweswariah, S. S. Impaired intestinal sodium transport in inflammatory bowel disease: from the passenger to the driver’s seat. Cell Mol. Gastroenterol. Hepatol. 12, 277–292 (2021).
Bose, A., Banerjee, S. & Visweswariah, S. S. Mutational landscape of receptor guanylyl cyclase C: functional analysis and disease-related mutations. IUBMB Life 72, 1145–1159 (2020).
Fiskerstrand, T. et al. Familial diarrhea syndrome caused by an activating GUCY2C mutation. N. Engl. J. Med. 366, 1586–1595 (2012).
Chae, J. J. et al. The B30.2 domain of pyrin, the familial Mediterranean fever protein, interacts directly with caspase-1 to modulate IL-1B production. Proc. Natl. Acad. Sci. USA 103, 9982–9987 (2006).
Cattan, D., Notarnicola, C. & Molinari, N. Inflammatory bowel disease in non-Ashkenazi Jews with familial Mediterranean fever. Lancet 355, 378–379 (2000).
Group, T.F.S. Familial Mediterranean fever (FMF) in Turkey: results of a nationwide multicenter study. Medicine 84, 1–11 (2005).
Soylemezoglu, O. et al. Unresponsiveness to colchicine therapy in patients with familial Mediterranean fever homozygous for the M694V mutation. J. Rheumatol. 37, 182–189 (2009).
Davis, B. K. et al. Emerging significance of NLRs in inflammatory bowel disease. Inflamm. Bowel Dis. 20, 2412–2432 (2014).
Vance, R. E. The NAIP/NLRC4 inflammasomes. Curr. Opin. Immunol. 32, 84–89 (2015).
Canna, S. W. et al. Life-threatening NLRC4-associated hyperinflammation successfully treated with Interleukin-18 inhibition. J. Allergy Clin. Immunol. 139, 1698–1701 (2017).
Julià, A. et al. A genome-wide association study identifies a novel locus at 6q22.1 associated with ulcerative colitis. Hum. Mol. Genet 23, 6927–6934 (2014).
Shaikh, T. H. et al. High-resolution mapping and analysis of copy number variations in the human genome: a data resource for clinical and research applications. Genome Res. 19, 1682–1690 (2009).
Sudmant, P. H. et al. Evolution and diversity of copy number variation in the great ape lineage. Genome Res. 23, 1373–1382 (2013).
Wong, K. K. et al. A comprehensive analysis of common copy-number variations in the human genome. Am. J. Hum. Genet 80, 91–104 (2007).
Uddin, M. et al. A high-resolution copy-number variation resource for clinical and population genetics. Genet Med. 17, 747–752 (2015).
Acknowledgements
Authors thank the interdisplinary medical team of Tarbiat Modares University, Pediatric Gastroenterology and Hepatology Research Center of Children’s Medical Center, Department of Pediatrics University of Dr. von Hauner Children’s Hospital, Research Institute for Gastroenterology and Liver Diseases of Shahid Beheshti University of Medical Sciences,Department of Pediatric Gastroenterology and Hepatology of Shiraz University of Medical Sciences, Department of Gastroenterology of Lorestan university of medical science, Institute of Translational Genomics Helmholtz Zentrum München German Research Center for Environmental Health, Department of Genetics, Reproductive Biomedicine Research Center, Royan Institute for Reproductive Biomedicine. We are thankful to Dr Pejman Rohani, head of the Pediatric IBD registery at Tehran University of Medical Science. We also thank the patients who participated in this study.
Funding
This work has been supported by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation; Collaborative Research Consortium (CRC)1054 project A05, CRC/TRR338 project C04), the Else Kröner-Fresenius-Stiftung, the Hector Foundation, the Helmholtz Young Investigator Group funds (Initiative and Networking Fund of the Helmholtz Association), the Leona M. and Harry B. Helmsley Charitable Trust, the VEO-IBD-Consortium, as well as institutional funds by the Dr. von Hauner Children’s Hospital.
Author information
Authors and Affiliations
Contributions
All authors contributed to this study. M.T. contributed to the study concept and design. P.R., S.S., F.F. and S.A. contributed to include patients to the study. M.H., P.R. and M.H.S. contributed to sample collection the acquisition of clinical data. M.S.A. provided pathology diagnostic support. M.R., C.K., D.K. contributed to the analysis and interpretation of data. M.H. contributed to the drafting of the manuscript. M.T., B.M.S., P.R., D.K. contributed to the critical revision of analysis of the manuscript for important intellectual content. M.T., D.K. and C.K. contributed to financial and technical supports.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The Research Ethics Committees of the Research Institute approved the study for Gastroenterology and Liver Disease (IRGLD, Shahid Beheshti University of Medical Science, Tehran, Iran, IR.SBMU.RIGLD.REC.1400.010) approved this study. Informed consent was obtained from all individual participants taking part in the study. This study is part of the Genetic Registry Program in Chronic IBD in Children’s Medical Center at Tehran University of Medical Sciences (IR.TUMS.MEDICINE.REC.1400.951).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Haghipanah, M., Rohani, P., Rohlfs, M. et al. Clinical and genomic features of Iranian patients with very early onset IBD. Pediatr Res (2026). https://doi.org/10.1038/s41390-025-04575-z
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04575-z