Abstract
Background
Physical punishment without maltreatment is still a common practice worldwide. However, there is a dearth of prospective evidence on the effects of physical punishment on children’s physical outcomes.
Methods
Data were derived from a 3-year cohort study of a representative sample of 3–6 years old Chinese children (n = 16715). Caregivers reported the usage of physical punishment, history of maltreatment, children’s physical health status (including recurrent sickness, general physical health status, and global sleep disturbance) and two measures of medical service utilization. A propensity score weighted model was used to evaluate the effects of physical punishment on physical health outcomes.
Results
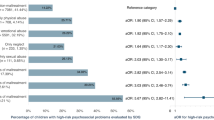
Physical punishment without maltreatment was associated with higher risk of recurrent sickness (OR = 1·15, 95% CI: 1·03,1·28), poorer general health (OR = 1·30, 95% CI: 1·16, 1·47), global sleep disturbances (OR = 1·42, 95% CI: 1·29, 1·55), and increased number of clinic visits (B = 0·18, 95% CI: 0·10, 0·26), but not the number of hospitalizations (B = 0·03, 95% CI: −0·01, 0·06).
Conclusion
Even without a history of maltreatment, physical punishment adversely affects children’s physical health and increases medical service utilization. Any form of physical discipline should be avoided.
Impact
-
The first population-representative cohort study to prospectively investigate the effects of physical punishment on physical health outcomes during early childhood.
-
Innovatively focus on physical punishment without maltreatment, revealing that even in the absence of maltreatment, physical punishment was associated with adverse physical well-being. These effects were maintained after the propensity score weighting for sociodemographic characteristics, socioeconomic status, nurturing environment factors, BMI, physical health during the neonatal period, and baseline physical health indicators.
-
Provides the first evidence that non-maltreating physical punishment independently predicts increased medical service utilization in early childhood. It highlights the hidden public health costs of physical punishment practices.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to shared ownership of Shanghai Municipal Education Commission but are available from the corresponding author on reasonable request.
References
United Nations Committee on the Rights of the Child. General Comment No. 8: The Right of the Child to Protection From Corporal Punishment and Other Cruel or Degrading Forms of Punishment. Geneva, Switzerland (2007).
United Nations Children’s Fund. A Familiar Face: Violence in the Lives of Children and Adolescents (UNICEF, New York, 2017).
Jaffee, S. R. Child maltreatment and risk for psychopathology in childhood and adulthood. Annu. Rev. Clin. Psychol. 13, 525–551 (2017).
Miller-Perrin, C. & Perrin, R. Physical punishment of children by US parents: moving beyond debate to promote children’s health and well-being. Psicol. Reflex Crit. 31, 16 (2018).
Oram, S. Child maltreatment and mental health. Lancet Psychiatry 6, 881–882 (2019).
Hughes, K. et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health 2, e356–e366 (2017).
Norman, R. E. et al. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 9, e1001349 (2012).
Heilmann, A. et al. Physical punishment and child outcomes: a narrative review of prospective studies. Lancet 398, 355–364 (2021).
Dede Yildirim, E., Roopnarine, J. L. & Abolhassani, A. Maternal use of physical and non-physical forms of discipline and preschoolers’ social and literacy skills in 25 African countries. Child Abus. Negl. 106, 104513 (2020).
Murray, A. S. & Mallie, J. P. Corporal punishment by mothers and development of children’s cognitive ability: a longitudinal study of two nationally representative age cohorts. J. Aggress. Maltreatment Trauma 18, 1–25 (2009).
Horn, I. B., Joseph, J. G. & Cheng, T. L. Nonabusive physical punishment and child behavior among African-American children: a systematic review. J. Natl. Med. Assoc. 96, 1162–1168 (2004).
Akmatov, M. K. Child abuse in 28 developing and transitional countries—results from the Multiple Indicator Cluster Surveys. Int. J. Epidemiol. 40, 219–227 (2011).
Huang G. H. C. & Gove M. Asian parenting styles and academic achievement: views from eastern and western perspectives. Education. 135, 389–397 (2015).
Afifi, T. O., Mota, N., MacMillan, H. L. & Sareen, J. Harsh physical punishment in childhood and adult physical health. Pediatrics 132, e333–e340 (2013).
Berger, R. P. & Zolotor, A. J. Is there an association between physical punishment in childhood and physical health in adulthood?. Pediatrics 132, e500–e501 (2013).
Wang, X. et al. Cohort Profile: The Shanghai Children’s Health, Education and Lifestyle Evaluation, Preschool (SCHEDULE-P) study. Int. J. Epidemiol. 50, 391–399 (2021).
Wang, H. et al. Types of on-screen content and mental health in kindergarten children. JAMA Pediatr. 178, 125–132 (2024).
Deng, Y. et al. Sleep disturbances and emotional and behavioral difficulties among preschool-aged children. JAMA Netw. Open 6, e2347623 (2023).
Zhao, J. et al. Association between screen time trajectory and early childhood development in children in China. JAMA Pediatr. 176, 768–775 (2022).
Chen, W. et al. The influence of home-rearing environment on children’s behavioral problems 3 years’ later. Psychiatry Res. 244, 185–193 (2016).
Shimada, K., Kasaba, R., Yao, A. & Tomoda, A. Less efficient detection of positive facial expressions in parents at risk of engaging in child physical abuse. BMC Psychol. 7, 56 (2019).
Gan-Yadam A. Quality of Child Care Environment among the Parents of Children with Disabilities, in the case of Khovd Province, Mongolia. Research Square. Preprint https://doi.org/10.21203/rs.3.rs-3874982/v1 (2024).
Anme T. et al. Validity and reliability of the index of child care environment (ICCE). Public Health Front. 2, 141 (2013).
Salum, G. A. et al. Measuring child maltreatment using multi-informant survey data: a higher-order confirmatory factor analysis. Trends Psychiatry Psychother. 38, 23–32 (2016).
Shan, W. et al. Positive parent-child interactions moderate certain maltreatment effects on psychosocial well-being in 6-year-old children. Pediatr. Res 95, 802–808 (2024).
Shan, W. et al. Association between maltreatment, hair cortisol concentration, positive parent-child interaction, and psychosocial outcomes in Chinese preschool children. Eur. Child Adolesc. Psychiatry 33, 2719–2730 (2024).
Zhao, J. et al. Measuring early childhood development with The Early Human Capability Index (eHCI): a reliability and validity study in China. BMC Pediatr. 20, 323 (2020).
Kenney, M. K. & Chanlongbutra, A. Prevalence of parent reported health conditions among 0- to 17-Year-olds in rural United States: National Survey of Children’s Health, 2016-2017. J. Rural Health 36, 394–409 (2020).
Owens, J. A., Spirito, A. & McGuinn, M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep 23, 1043–1051 (2000).
Li, S. et al. Development and psychometric properties of the Chinese version of Children’s Sleep Habits Questionnaire. Zhonghua er ke za zhi/Chin. J. Pediatr. 45, 176–180 (2007).
Wang, Y. et al. Effects of sleep disturbances on behavioral problems in preschool children with autism spectrum disorder. Front Psychiatry 11, 559694 (2020).
Chen, X., Ke, Z. L., Chen, Y. & Lin, X. The prevalence of sleep problems among children in mainland China: a meta-analysis and systemic-analysis. Sleep. Med 83, 248–255 (2021).
Li X., et al. Parent-preferred childcare environment styles: a latent class analysis and association with parental stress. Child. Youth Serv. Rev. 155, 107176 (2023).
Ruffolo, L. I. et al. Outcomes after child physical abuse and association with community-level social determinants of health. J. Am. Coll. Surg. 235, 810–818 (2022).
Kendall-Tackett, K. & Klest, B. Causal mechanisms and multidirectional pathways between trauma, dissociation, and health. J. Trauma Dissociation 10, 129–134 (2009).
Sachs-Ericsson, N., Cromer, K., Hernandez, A. & Kendall-Tackett, K. A review of childhood abuse, health, and pain-related problems: the role of psychiatric disorders and current life stress. J. Trauma Dissociation 10, 170–188 (2009).
Hornor, G. Childhood trauma exposure and toxic stress: what the PNP needs to know. J. Pediatr. Health Care 29, 191–198 (2015).
Liu, Y. et al. Do children evaluated for maltreatment have higher subsequent emergency department and inpatient care utilization compared to a general pediatric sample?. Child Abus. Negl. 134, 105938 (2022).
Wang, S. et al. Characteristics of prescriptions and costs for acute upper respiratory tract infections in Chinese outpatient pediatric patients: a nationwide cross-sectional study. BMC Complement Med. Ther. 20, 346 (2020).
Wu, P. et al. The economic burden of medical treatment of children with asthma in China. BMC Pediatr. 20, 386 (2020).
Yang, J. et al. The economic burden of influenza-associated outpatient visits and hospitalizations in China: a retrospective survey. Infect. Dis. Poverty 4, 44 (2015).
Wang, D. et al. Socio-economic burden of influenza among children younger than 5 years in the outpatient setting in Suzhou, China. PLoS ONE 8, e69035 (2013).
Acknowledgements
This study was sponsored by Shanghai Pujiang Programme (24PJD070), Shanghai Jiao Tong University Medical-Industrial Interdisciplinary Research Fund (YG2025QNB09), National Natural Science Foundation of China (82103866), National Natural Science Foundation of China Joint Fund Project (U23A20170), Shanghai Municipal Education Commission (2024you1-1, D1502), Innovative Research Team of High-level Local Universities in Shanghai (SHSMU-ZDCX20211900), and Shanghai Key Laboratory of Child Brain and Development (24dz2260100).
Author information
Authors and Affiliations
Contributions
Wenjie Shan (W.S.), Yihong Wang (Y.W.), Yunting Zhang (Y.Z.) and Fan Jiang (F.J.) took the initiative in conception and design. W.S., Y.W., and Jin Zhao (J.Z.) conducted the investigation, collected the data, and provided critical suggestions on data analysis. WS and YW analyzed the data, and W.S. completed the draft. W.S., Y.W., Y.Z., F.J., Lei Zhang (L.Z.), and Patrick Ip (P.I.) made substantial contributions to the interpretation of data and manuscript revision. WS, YW, and JZ directly accessed and verified the underlying data reported in the manuscript. All the authors accepted full responsibility for the finished work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
The study received approval from the institutional review board of the Shanghai Children’s Medical Center, Shanghai Jiao Tong University (SCMCIRB-K2016022-01). Parents of the involved children signed the informed consent before participating in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shan, W., Wang, Y., Zhang, Y. et al. Association of physical punishment and health outcomes in early childhood: a population representative prospective study. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04600-1
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04600-1