Abstract
Background
Sevoflurane anesthesia is employed as the standard protocol for pediatric patients undergoing fundus examination. This study investigates the incidence of emergence delirium (ED) and its risk factors in this population, and explores the relationship between ED and negative postoperative behavioral changes (NPOBC).
Methods
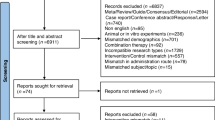
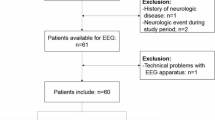
A prospective observational study was conducted from May to September 2024, involving 155 children aged 0–3 years undergoing fundus examination under general anesthesia. Patient and surgery-related data were recorded. ED was assessed using the Pediatric Anesthesia Emergence Delirium (PAED) scale, with logistic regression identifying associated factors. Postoperative behaviors were evaluated one week later using the Post-Hospital Behavior Questionnaire for Ambulatory Surgery (PHBQ-AS), with linear regression analyzing the relationship between ED and NPOBC.
Results
In 155 patients, ED incidence was 51%. In the 96 followed-up, NPOBC one week postoperatively was seen in 30.2%. Risk factors for ED included prenatal medical history (OR = 3.70, 95% CI 1.31–10.40, P = 0.013), anesthesia exposure (OR = 1.73, 95% CI 1.36–2.20, P < 0.001), preoperative anxiety (OR = 2.35, 95% CI 1.40–3.94, P = 0.001), and postoperative pain (OR = 1.69, 95% CI 1.31–2.19, P < 0.001). Increased negative behavioral scale scores were associated with anesthesia exposure (B = 0.260, 95% CI 0.123–0.396, P < 0.001) and ED occurrence (B = 1.420, 95% CI 0.598–2.234, P < 0.001).
Conclusion
Our study shows a high incidence of negative emotions and behaviors. Future research should focus on optimizing postoperative analgesia and preoperative anti-anxiety interventions for this high-risk group, and further exploring the connections among anesthesia exposure, ED and NPOBC.
Impact
-
Our study showed a high incidence of negative emotions and behaviors (emergence delirium and postoperative behavioral changes) in minimally invasive fundus examinations under total inhalation anesthesia.
-
Risk factors for emergence delirium are prenatal medical history, anesthesia exposure, preoperative anxiety and postoperative pain. Higher negative behavior scores were associated with anesthesia exposure and emergence delirium.
-
This is the first study to explore the incidence and risk factors of behavioral abnormalities in infants and preterm children after general anesthesia, making it easier to spot high-risk kids having fundus exams and to fine-tune anesthesia and perioperative care for short, minimally invasive procedures.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Mead, A. L., Chen, S. D., Wilkinson, A. & Patel, C. K. Anaesthesia for the laser treatment of neonates with retinopathy of prematurity. Eye 22, 734 (2008).
Costi, D. et al. Effects of sevoflurane versus other general anaesthesia on emergence agitation in children. Cochrane Database Syst. Rev. 2014, CD007084 (2014).
Aldakhil, S. K. et al. The prevalence of emergence delirium and its associated factors among children at a postoperative unit: a retrospective cohort at a Middle Eastern hospital. Saudi J. Anaesth. 14, 169–176 (2020).
Aldecoa, C. et al. European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur. J. Anaesthesiol. 34, 192–214 (2017).
Cole, J. W., Murray, D. J., McAllister, J. D. & Hirshberg, G. E. Emergence behaviour in children: defining the incidence of excitement and agitation following anaesthesia. Paediatr. Anaesth. 12, 442–447 (2002).
Lee, S. J. & Sung, T. Y. Emergence agitation: current knowledge and unresolved questions. Korean J. Anesthesiol. 73, 471–485 (2020).
Mason, K. P. Paediatric emergence delirium: a comprehensive review and interpretation of the literature. Br. J. Anaesth. 118, 335–343 (2017).
Voepel-Lewis, T., Malviya, S. & Tait, A. R. A prospective cohort study of emergence agitation in the pediatric postanesthesia care unit. Anesth. Analg. 96, 1625–1630 (2003).
Kanaya, A. Emergence agitation in children: risk factors, prevention, and treatment. J. Anesth. 30, 261–267 (2016).
Kain, Z. N. et al. Preoperative anxiety and emergence delirium and postoperative maladaptive behaviors. Anesth. Analg. 99, 1648–1654 (2004).
Yu, L., Sun, H., Yao, L. & Feng, Y. An approach to using central pupils as a clinical sign to assess depth of anesthesia in infants undergoing fundus examination with inhalation of sevoflurane. J. Clin. Anesth. 29, 5–9 (2016).
Aldrete, J. A. Post-anesthetic recovery score. J. Am. Coll. Surg. 205, e3–e5 (2007).
Kain, Z. N., Mayes, L. C., Weisman, S. J. & Hofstadter, M. B. Social adaptability, cognitive abilities, and other predictors for children’s reactions to surgery. J. Clin. Anesth. 12, 549–554 (2000).
Sikich, N. & Lerman, J. Development and psychometric evaluation of the pediatric anesthesia emergence delirium scale. Anesthesiology 100, 1138–1145 (2004).
Bajwa, S. A., Costi, D. & Cyna, A. M. A comparison of emergence delirium scales following general anesthesia in children. Paediatr. Anaesth. 20, 704–711 (2010).
Merkel, S. I., Voepel-Lewis, T., Shayevitz, J. R. & Malviya, S. The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr. Nurs. 23, 293–297 (1997).
Jenkins, B. N. et al. Revisiting a measure of child postoperative recovery: development of the Post hospitalization Behavior Questionnaire for ambulatory surgery. Paediatr. Anaesth. 25, 738–745 (2015).
Hino, M. et al. Development and validation of a risk scale for emergence agitation after general anesthesia in children: a prospective observational study. Anesth. Analg. 125, 550–555 (2017).
Eshetie, D., Getinet, H., Abdissa, Z. & Mollalign, M. Incidence and associated factors of emergence agitation after general anesthesia and surgery among pediatric patients: a prospective follow-up study. Int. J. Surg. Open. 27, 25–31 (2020).
Farag, R. S. et al. Incidence of emergence agitation in children undergoing sevoflurane anesthesia compared to isoflurane anesthesia: an updated systematic review and meta-analysis. Paediatr. Anaesth. 34, 304–317 (2024).
Costi, D. et al. Middleton P. Effects of sevoflurane versus other general anaesthesia on emergence agitation in children. Cochrane Database Syst. Rev. 2014, CD007084 (2014).
Gao, X. et al. Electroencephalographic insights into the pathophysiological mechanisms of emergence delirium in children and corresponding clinical treatment strategies. Front. Pharmacol. 15, 1349105 (2024).
Poorun, R. et al. Electroencephalography during general anaesthesia differs between term-born and premature-born children. Clin. Neurophysiol. 127, 1216–1222 (2016).
Kim, J. et al. Frontal electroencephalogram activity during emergence from general anaesthesia in children with and without emergence delirium. Br. J. Anaesth. 126, 293–303 (2021).
Apai, C., Shah, R., Tran, K. & Pandya Shah, S. Anesthesia and the developing brain: a review of sevoflurane-induced neurotoxicity in pediatric populations. Clin. Ther. 43, 762–778 (2021).
Subramaniyan, S. & Terrando, N. Neuroinflammation and Perioperative Neurocognitive Disorders. Anesth. Analg. 128, 781–788 (2019).
Yu, H., Sun, X., Li, P. & Deng, X. Prevalence and risk factors of emergence agitation among pediatric patients undergo ophthalmic and ENT Surgery: a cross-sectional study. BMC Pediatr. 23, 598 (2023).
Xue, Q., Xia, J., Lu, J. & Shen, X. Added syrup as a flavoring to oral midazolam intravenous solution premedication improves tolerability in pediatric patients. Drug Des. Dev. Ther. 16, 1211–1216 (2022).
He, H. et al. The effect of intranasal dexmedetomidine on emergence delirium prevention in pediatric ambulatory dental rehabilitation under general anesthesia: a randomized clinical trial. Drug Des. Dev. Ther. 17, 3563–3570 (2023).
Eijlers, R. et al. Virtual reality exposure before elective day care surgery to reduce anxiety and pain in children: a randomised controlled trial. Eur. J. Anaesthesiol. 36, 728–737 (2019).
Muzzi, E. et al. Effects of intraoperative auditory stimulation on pain and agitation on awakening after pediatric adenotonsillectomy: a randomized clinical trial. JAMA Otolaryngol. Head. Neck Surg. 147, 638–645 (2021).
Yang, Y. Y. et al. Effect of recorded maternal voice on emergence agitation in children undergoing bilateral ophthalmic surgery: a randomised controlled trial. J. Paediatr. Child Health 56, 1402–1407 (2020).
Larsen, L. G., Wegger, M., Lé Greves, S., Erngaard, L. & Hansen, T. G. Emergence agitation in paediatric day case surgery: a randomised, single-blinded study comparing narcotrend and heart rate variability with standard monitoring. Eur. J. Anaesthesiol. 39, 261–268 (2022).
Acknowledgements
The authors thank the surgeons and nurses working in the ophthalmic surgery units for their involvement and support.
Funding
This study received no financial support from gene-related projects, commercial entities, or public funding agencies.
Author information
Authors and Affiliations
Contributions
Wanlu Zhao and HASHIMOTO KINJI have given substantial contributions to the conception or the design of the manuscript, Weisi Ding to collection of the data, Yunpeng Zhang and Chunyu Guo to analysis and interpretation of the data. All authors have participated in drafting the manuscript, and Yi Feng & Haiyan An revised it critically. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Peking University People’s Hospital (Approval No. 2024PHB133 − 001). Written informed consent was obtained from the legal guardian of the children before they were enrolled in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, W., Hashimoto, K., Ding, W. et al. Risk factors for emergence delirium in infant-toddlers undergoing sevoflurane anesthesia and its impact on negative postoperative behavioral changes. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04608-7
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04608-7