Abstract
Background
In retrospective studies, intestinal fatty acid binding protein (I-FABP) has been suggested as a potential biomarker to identify NEC prior to clinical diagnosis. We hypothesize that increasing I-FABP levels with feeding advancement may be a biomarker of intestinal stress prior to clinical suspicion of NEC.
Methods
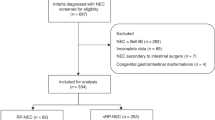
Prospective study of neonates ≤ 32-week gestation and ≤1500 grams enrolled within 72 h of life. Blood was obtained for biomarker assessment with feeding advancement. ELISA was used to assay serum I-FABP (sI-FABP).
Results
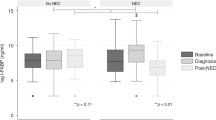
Of 96 patients enrolled, 9 were diagnosed with NEC. sI-FABP values remained low in healthy controls and NEC patients at the initial stages of feeding, up to 60 mL/kg/day. In those who developed NEC, there was a significantly higher sI-FABP at the final sample compared to their own earlier samples (p < 0.0001) or matched controls (p < 0.001). Those who developed NEC while feed volumes were being increased had a significantly higher sI-FABP than others. Receiver operating characteristic (ROC) curve analysis identified sI-FABP of 4.8 ng/mL to be predictive of early NEC with 80% sensitivity and 100% specificity (AUC 0.92; p < 0.01).
Conclusion
Elevation in sI-FABP with increasing volume of enteral feeds correlates with, and precedes, clinical suspicion of NEC.
Impact
-
Serum intestinal fatty acid binding protein elevation during feeding advancement is a sensitive and specific biomarker for necrotizing enterocolitis that precedes clinical suspicion.
-
Early and accurate identification of infants at risk for necrotizing enterocolitis prior to development of symptoms allows the identification of patients at risk that may benefit from early intervention or trial of potential therapies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Dominguez, K. M. & Moss, R. L. Necrotizing enterocolitis. Clin. Perinatol. 39, 387–401 (2012).
Rich, B. S. & Dolgin, S. E. Necrotizing enterocolitis. Pediatr. Rev. 38, 552–559 (2017).
Battersby, C., Santhalingam, T., Costeloe, K. & Modi, N. Incidence of neonatal necrotising enterocolitis in high-income countries: a systematic review. Arch. Dis. Child Fetal Neonatal Ed. 103, F182–F189 (2018).
Denning, N. L. & Prince, J. M. Neonatal intestinal dysbiosis in necrotizing enterocolitis. Mol. Med 24, 4 (2018).
Ibrahim, N. R., Van Rostenberghe, H., Ho, J. J. & Nasir, A. Short versus long feeding interval for bolus feedings in very preterm infants. Cochrane Database Syst. Rev. 8, CD012322 (2021).
Morgan, J., Young, L. & McGuire, W. Delayed introduction of progressive enteral feeds to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Syst. Rev. 12, CD001970 (2014).
Neu, J. & Pammi, M. Pathogenesis of Nec: impact of an altered intestinal microbiome. Semin Perinatol. 41, 29–35 (2017).
Hsueh, W. et al. Neonatal necrotizing enterocolitis: clinical considerations and pathogenetic concepts. Pediatr. Dev. Pathol. 6, 6–23 (2003).
Jones, I. H. & Hall, N. J. Contemporary outcomes for infants with necrotizing enterocolitis-a systematic review. J. Pediatr. 220, 86–92.e83 (2020).
Lieberman, J. M., Sacchettini, J., Marks, C. & Marks, W. H. Human intestinal fatty acid binding protein: report of an assay with studies in normal volunteers and intestinal ischemia. Surgery 121, 335–342 (1997).
Relja, B. et al. Intestinal-Fabp and Liver-Fabp: novel markers for severe abdominal injury. Acad. Emerg. Med 17, 729–735 (2010).
Gollin, G., Marks, C. & Marks, W. H. Intestinal fatty acid binding protein in serum and urine reflects early ischemic injury to the small bowel. Surgery 113, 545–551 (1993).
Zamora, I. J. et al. Low abdominal nirs values and elevated plasma intestinal fatty acid-binding protein in a premature piglet model of necrotizing enterocolitis. PLoS One 10, e0125437 (2015).
Schurink, M. et al. Intestinal fatty acid-binding protein as a diagnostic marker for complicated and uncomplicated necrotizing enterocolitis: a prospective cohort study. PLoS One 10, e0121336 (2015).
Mannoia, K. et al. Necrotizing enterocolitis is associated with neonatal intestinal injury. J. Pediatr. Surg. 46, 81–85 (2011).
Shaaban, A. I. E., Alfqy, O. A. E., Shaaban, H. M. K., YH, A. M. & Assar, E. H. Potential role of serum intestinal fatty acid-binding protein as a marker for early prediction and diagnosis of necrotizing enterocolitis in preterm neonates. J. Indian Assoc. Pediatr. Surg. 26, 393–400 (2021).
Aydemir, C. et al. Serum intestinal fatty acid binding protein level for early diagnosis and prediction of severity of necrotizing enterocolitis. Early Hum. Dev. 87, 659–661 (2011).
Viswanathan, S., Merheb, R., Wen, X., Collin, M. & Groh-Wargo, S. Standardized slow enteral feeding protocol reduces necrotizing enterocolitis in micropremies. J. Neonatal Perinat. Med. 10, 171–180 (2017).
Dako, J. et al. Slow enteral feeding decreases risk of transfusion associated necrotizing enterocolitis. J. Neonatal Perinat. Med. 11, 231–239 (2018).
Dorling, J. et al. Two speeds of increasing milk feeds for very preterm or very low-birthweight infants: the SIFT RCT. Health Technol. Assess. 24, 1–94 (2020).
Abiramalatha, T., Thomas, N. & Thanigainathan, S. High versus standard volume enteral feeds to promote growth in preterm or low birth weight infants. Cochrane Database Syst. Rev. 3, CD012413 (2021).
Sbragia, L. et al. Intestinal fatty acid-binding protein as a marker of necrotizing enterocolitis incidence and severity: a scoping review. J. Surg. Res. 303, 613–627 (2024).
Edelson, M. B. et al. Plasma intestinal fatty acid binding protein in neonates with necrotizing enterocolitis: a pilot study. J. Pediatr. Surg. 34, 1453–1457 (1999).
Acknowledgements
We thank our colleagues from the Ohio Perinatal Research Network who contributed significantly to patient recruitment and sample/data collection for the study: No financial assistance was received in support of this study.
Author information
Authors and Affiliations
Contributions
S.H. conceptualization, methodology, validation, formal analysis, investigation, writing—original draft, writing—review and editing, visualization. J.W. writing—original draft, writing—review & editing. C.S. investigation, data curation. L.S. conceptualization, writing—original draft, writing–review & editing, supervision. O.O.O. conceptualization, methodology, validation, resources, writing—original draft, writing—review & editing, supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Informed consent was obtained for all subjects enrolled in this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hameedi, S.G., Wright, J.G., Schafer, C.G. et al. Serum intestinal fatty acid binding protein is elevated during feeding advancement in necrotizing enterocolitis. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04614-9
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04614-9
This article is cited by
-
The futile search for biomarkers for necrotizing enterocolitis
Pediatric Research (2026)