Abstract
Background
While fetal hypoxia-ischemia is a known trigger for meconium aspiration syndrome (MAS), many infants develop MAS without it, suggesting other risk factors. We examined the association between MAS and the presence and severity of fetal inflammatory response (FIR) on placental histopathology.
Methods/Study design
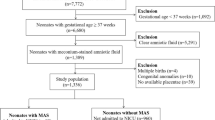
A single-center retrospective cohort study of term infants with meconium-stained amniotic fluid (MSAF) born at Parkland Hospital (2010–2018). Maternal and infant demographics and clinical data were recorded. Placental histopathologic evidence of FIR was classified per Amsterdam criteria. MAS was defined as respiratory distress in an infant with MSAF requiring NICU admission and ≥48 hours of respiratory support and/or radiographic findings of MAS.
Results
Among 1,696 term neonates with MSAF, 118 (6.9%) developed MAS. Univariate analysis showed that MAS was associated with post-term delivery, non-reassuring fetal heart patterns, cesarean delivery, thick meconium, low Apgar scores, severe acidosis, and presence of FIR (all P < 0.001). On multivariate analysis, FIR remained significant (adjusted OR 2.50, 95% CI 1.41–4.82). Moderate to severe FIR conferred 5-times higher odds for developing MAS (adjusted OR 5.43, 95% CI 2.83–10.40).
Conclusion
FIR, particularly its severity, is an independent predictor of MAS, highlighting intrauterine inflammation as a key mechanism alongside hypoxia-ischemia.
Impact
-
Fetal Inflammatory Response (FIR) is independently associated with Meconium Aspiration Syndrome (MAS)
-
Increasing severity of FIR confers progressively higher risk of MAS.
-
This is the first study to demonstrate a dose-response relationship between FIR severity on MAS.
-
These observations highlight the role of intrauterine inflammation in MAS pathogenesis and provide new insight into its impact on term neonates.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Yoder, B. A., Kirsch, E. A., Barth, W. H. & Gordon, M. C. Changing obstetric practices associated with decreasing incidence of meconium aspiration syndrome. Obstet. Gynecol. 99, 731–739 (2002).
Dargaville, P. A., Copnell, B. & Australian & New Zealand Neonatal, N The epidemiology of meconium aspiration syndrome: incidence, risk factors, therapies, and outcome. Pediatrics 117, 1712–1721 (2006).
Swarnam, K., Soraisham, A. S. & Sivanandan, S. Advances in the management of meconium aspiration syndrome. Int J. Pediatr. 2012, 359571 (2012).
Davis, R. O., Philips, J. B. 3rd, Harris, B. A. Jr, Wilson, E. R. & Huddleston, J. F. Fatal meconium aspiration syndrome occurring despite airway management considered appropriate. Am. J. Obstet. Gynecol. 151, 731–736 (1985).
Wiswell, T. E. & Bent, R. C. Meconium staining and the meconium aspiration syndrome. Unresolved issues. Pediatr. Clin. North Am. 40, 955–981 (1993).
Hernandez, C., Little, B. B., Dax, J. S., Gilstrap, L. C. 3rd & Rosenfeld, C. R. Prediction of the severity of meconium aspiration syndrome. Am. J. Obstet. Gynecol. 169, 61–70 (1993).
Yokoi, K. et al. Evidence of both foetal inflammation and hypoxia-ischaemia is associated with meconium aspiration syndrome. Sci. Rep. 11, 16799 (2021).
Ahanya, S. N., Lakshmanan, J., Morgan, B. L. & Ross, M. G. Meconium passage in utero: mechanisms, consequences, and management. Obstet. Gynecol. Surv. 60, 45–56 (2005). quiz 73-44.
van Ierland, Y. & de Beaufort, A. J. Why does meconium cause meconium aspiration syndrome? Current concepts of MAS pathophysiology. Early Hum. Dev. 85, 617–620 (2009).
Trimmer, K. J. & Gilstrap, L. C. 3rd “Meconiumcrit” and birth asphyxia. Am. J. Obstet. Gynecol. 165, 1010–1013 (1991).
Ramin, S. M., Gilstrap, L. C. 3rd, Leveno, K. J., Dax, J. S. & Little, B. B. Acid-base significance of meconium discovered prior to labor. Am. J. Perinatol. 10, 143–145 (1993).
Blackwell, S. C. et al. Meconium aspiration syndrome in term neonates with normal acid-base status at delivery: is it different?. Am. J. Obstet. Gynecol. 184, 1422–1425 (2001).
Oyelese, Y. et al. Meconium-stained amniotic fluid across gestation and neonatal acid-base status. Obstet. Gynecol. 108, 345–349 (2006).
Yeomans, E. R., Gilstrap, L. C. 3rd, Leveno, K. J. & Burris, J. S. Meconium in the amniotic fluid and fetal acid-base status. Obstet. Gynecol. 73, 175–178 (1989).
Ghidini, A. & Spong, C. Y. Severe meconium aspiration syndrome is not caused by aspiration of meconium. Am. J. Obstet. Gynecol. 185, 931–938 (2001).
Lee, J. et al. Meconium aspiration syndrome: a role for fetal systemic inflammation. Am. J. Obstet. Gynecol. 214, 366 e361–369 (2016).
Romero, R. et al. Meconium-stained amniotic fluid: a risk factor for microbial invasion of the amniotic cavity. Am. J. Obstet. Gynecol. 164, 859–862 (1991).
Romero, R. et al. Bacteria and endotoxin in meconium-stained amniotic fluid at term: could intra-amniotic infection cause meconium passage?. J. Matern Fetal Neonatal Med 27, 775–788 (2014).
Mazouri, A., Fallah, R., Saboute, M., Taherifard, P. & Dehghan, M. The prognostic value of the level of lactate in umbilical cord blood in predicting complications of neonates with meconium aspiration syndrome. J. Matern Fetal Neonatal Med 34, 1013–1019 (2021).
Roberts, D. J. et al. Acute histologic chorioamnionitis at term: nearly always noninfectious. PLoS One 7, e31819 (2012).
Yokoi, K., Iwata, O., Kobayashi, S., Muramatsu, K. & Goto, H. Influence of foetal inflammation on the development of meconium aspiration syndrome in term neonates with meconium-stained amniotic fluid. PeerJ 7, e7049 (2019).
Thureen, P. J., Hall, D. M., Hoffenberg, A. & Tyson, R. W. Fatal meconium aspiration in spite of appropriate perinatal airway management: pulmonary and placental evidence of prenatal disease. Am. J. Obstet. Gynecol. 176, 967–975 (1997).
Greer, L. G. et al. An immunologic basis for placental insufficiency in fetal growth restriction. Am. J. Perinatol. 29, 533–538 (2012).
Khong, T. Y. et al. Sampling and Definitions of Placental Lesions: Amsterdam Placental Workshop Group Consensus Statement. Arch. Pathol. Lab Med 140, 698–713 (2016).
Mir, I. N. et al. Placental pathology is associated with severity of neonatal encephalopathy and adverse developmental outcomes following hypothermia. Am. J. Obstet. Gynecol. 213, 849 e841–847 (2015).
Alayli, Y. et al. Neurodevelopmental outcomes in extremely preterm infants with placental pathologic evidence of fetal inflammatroy response. Pediatr. Res 97, 1147–1154 (2025).
Wolfs, T. G. et al. Chorioamnionitis-induced fetal gut injury is mediated by direct gut exposure of inflammatory mediators or by lung inflammation. Am. J. Physiol. Gastrointest. Liver Physiol. 306, G382–G393 (2014).
Liu, F. D. & McCullough, L. D. Inflammatory responses in hypoxic ischemic encephalopathy. Acta Pharm. Sin. 34, 1121–1130 (2013).
Pacora, P. et al. Funisitis and chorionic vasculitis: the histological counterpart of the fetal inflammatory response syndrome. J. Matern Fetal Neonatal Med 11, 18–25 (2002).
Acknowledgements
We wish to thank several people who participated in data collection: Patti J Burchfield, RN, and Pollieanna M Sepulveda, RN.
Funding
This work was supported by Children’s Clinical Research Advisory Council (CCRAC) grant awarded to Dr. Imran N. Mir.
Author information
Authors and Affiliations
Contributions
Imran N. Mir wrote the first version of the manuscript. Steven Brown performed statistical analyses. All authors participated in the study design, data collection, data interpretation, and revision and approval of the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
The Institutional Review Board of University of Texas Southwestern Medical Center and Parkland Health approved the study and waived the need for individual consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gonzalez, R., Brown, S., Sisman, J. et al. Fetal inflammatory response severity on placental histology identifies neonates at risk for meconium aspiration syndrome. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04657-y
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04657-y