Abstract
Background
To investigate the relationship between inflammatory indicators and bone mineral density in preschool children.
Methods
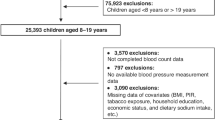
The study population consisted of 393 preschool children aged 4–6 years. NLR, PLR, SII, and PIV were calculated based on lymphocyte counts, neutrophil counts, platelet counts and monocyte counts derived from a complete blood count test. The relationships between inflammatory indicators with BMD increment were analyzed using covariance analysis. ROC curve analysis was used to find a cut-off point for inflammatory indicators that can be assessed for BMD insufficiency. Multiple linear regression models were used to analyze the association between inflammatory indicators and bone metabolism markers.
Results
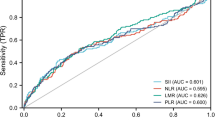
NLR (p-trend = 0.010), PIV (p-trend = 0.004) and SII (p-trend = 0.015) were positively associated with BMD increments, whereas PLR was not. ROC curve analysis showed that PIV (AUC = 0.58, 95% CI 0.52–0.64) and SII (AUC = 0.56, 95% CI 0.50–0.62) can predict low BMD, with PIV having the highest ability to predict. PIV was positively associated with osteocalcin and 25⁃(OH)D, whereas SII was positively associated with osteocalcin only.
Conclusion
PIV, SII, and NLR were positively associated with BMD increment. The study suggests that PIV holds promise as a potential tool for predicting the risk of BMD insufficiency in preschool children.
Impact
-
After controlling for various confounders during a 1-year observation period, significant associations were found between the inflammatory indicators NLR, SII, and PIV and increased left-sided heel BMD in preschool children, exploring the finding that chronic inflammation plays a different role in children’s bone health than it does in adults.
-
Our findings found that PIV holds promise as a potential tool for predicting the risk of BMD insufficiency in preschool children. Focusing on bone mineral density in preschool children, this study provides valuable evidence and fills a gap in research on this age group.
-
In the study, osteocalcin was also found to be positively correlated with SII and PIV and 25⁃(OH)D was positively correlated with PIV. They may provide potential avenues to enhance understanding of the effects of inflammation on bone.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Xiao, P. L. et al. Global, regional prevalence, and risk factors of osteoporosis according to the World Health Organization diagnostic criteria: a systematic review and meta-analysis. Osteoporos. Int 33, 2137–2153 (2022).
Si, L., Winzenberg, T. M., Jiang, Q., Chen, M. & Palmer, A. J. Projection of osteoporosis-related fractures and costs in China: 2010-2050. Osteoporos. Int 26, 1929–1937 (2015).
Qiu, X. et al. Upper limb pediatric fractures in 22 tertiary children’s hospitals, China: a multicenter epidemiological investigation and economic factor analysis of 32,832 hospitalized children. J. Orthop. Surg. Res. 17, 300 (2022).
Murray, T. M. Prevention and Management of Osteoporosis: Consensus Statements from the Scientific Advisory Board of the Osteoporosis Society of Canada. 4. Calcium Nutrition and Osteoporosis. CMAJ 155, 935–939 (1996).
Kong, H., He, Z., Li, H., Xing, D. & Lin, J. The association between fluoride and bone mineral density in us children and adolescents: a pilot study. Nutrients 16, 2948 (2024).
Wheater, G., Elshahaly, M., Tuck, S. P., Datta, H. K. & van Laar, J. M. The clinical utility of bone marker measurements in osteoporosis. J. Transl. Med. 11, 201 (2013).
Greenblatt, M. B., Tsai, J. N. & Wein, M. N. Bone turnover markers in the diagnosis and monitoring of metabolic bone disease. Clin. Chem. 63, 464–474 (2017).
Lehtonen-Veromaa, M. et al. A 1-year prospective study on the relationship between physical activity, markers of bone metabolism, and bone acquisition in peripubertal girls. J. Clin. Endocr. Metab. 85, 3726–3732 (2000).
Tommasi, M. et al. Serum biochemical markers of bone turnover in healthy infants and children. IJBM 11, 159–164 (1996).
Léger, J. et al. The relationship between the gh/igf-i axis and serum markers of bone turnover metabolism in healthy children. Eur. J. Endocrinol. 157, 685–692 (2007).
Duren, D. L. et al. Quantitative genetics of cortical bone mass in healthy 10-year-old children from the Fels Longitudinal Study. Bone 40, 464–470 (2007).
Peng, Y., Zhong, Z., Huang, C. & Wang, W. The effects of popular diets on bone health in the past decade: a narrative review. Front Endocrinol. 14, 1287140 (2023).
Buckley, J. P. et al. Per- and Polyfluoroalkyl substances and bone mineral content in early adolescence: modification by diet and physical activity. Environ. Res. 252, 118872 (2024).
Sigvaldsen, A. et al. Prenatal and childhood exposure to bisphenols and bone mineral density in 7-year-old children from the Odense Child Cohort. Int. J. Hyg. Environ. Health 260, 114408 (2024).
Okamoto, K. & Takayanagi, H. Osteoimmunology. Cold Spring Harb Perspect. Med. 9, a031245 (2019).
Okamoto, K. et al. Osteoimmunology: the conceptual framework unifying the immune and skeletal systems. Physiol. Rev. 97, 1295–1349 (2017).
Limmer, A. & Wirtz, D. C. Osteoimmunology: Influence of the Immune System on Bone Regeneration and Consumption. Z. Orthop. Unf. 155, 273–280 (2017).
Weitzmann, M. N. & Ofotokun, I. Physiological and pathophysiological bone turnover - role of the immune system. Nat. Rev. Endocrinol. 12, 518–532 (2016).
Bozan, N. et al. Mean platelet volume, red cell distribution width, platelet-to-lymphocyte and neutrophil-to-lymphocyte ratios in patients with ankylosing spondylitis and their relationships with high-frequency hearing thresholds. Eur. Arch. Otorhinolaryngol. 273, 3663–3672 (2016).
Zhang, L. N. et al. Association between systemic inflammation markers and blood pressure among children and adolescents: National Health and Nutrition Examination Survey. Pediatr. Res. 97, 558–567 (2024).
Hu, B. et al. Systemic Immune-Inflammation Index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin. Cancer Res. 20, 6212–6222 (2014).
Jomrich, G. et al. High systemic immune-inflammation index is an adverse prognostic factor for patients with gastroesophageal adenocarcinoma. Ann. Surg. 273, 532–541 (2021).
Qin, Z. et al. Systemic Immune-Inflammation Index is associated with increased urinary albumin excretion: a population-based study. Front. immunol. 13, 863640 (2022).
Fucà, G. et al. The pan-immune-inflammation value is a new prognostic biomarker in metastatic colorectal cancer: results from a pooled-analysis of the valentino and tribe first-line trials. Br. J. Cancer 123, 403–409 (2020).
Zhang, X. J. et al. Blood cell count-derived inflammation indices as predictors of the osteoporotic risk of postmenopausal women. Eur. Rev. Med. Pharmacol. Sci. 28, 2207–2216 (2024).
Qu, L., Zuo, X., Yu, J., Duan, R. & Zhao, B. Association of inflammatory markers with all-cause mortality and cardiovascular mortality in postmenopausal women with osteoporosis or osteopenia. BMC Women’s. Health 23, 487 (2023).
Wang, Z. et al. High Platelet-to-lymphocyte Ratio Predicts Poor Survival Of Elderly Patients With Hip Fracture. Int Orthop. 45, 13–21 (2021).
Chen, S., Sun, X., Jin, J., Zhou, G. & Li, Z. Association between inflammatory markers and bone mineral density: a cross-sectional study from NHANES 2007–2010. J. Orthop. Surg. Res. 18, 305 (2023).
Morawiecka-Pietrzak, M. et al. The relationship of neutrophil-to-lymphocyte ratio and the platelet-to-lymphocyte ratio with bone mineral density in adolescent girls suffering from Anorexia Nervosa. Endokrynol. Pol. 72, 336–346 (2021).
Bala, M. M. & Bala, K. A. Bone Mineral Density (BMD) and Neutrophil-Lymphocyte Ratio (NLR), Monocyte-Lymphocyte Ratio (MLR), and Platelet-Lymphocyte Ratio (PLR) in Childhood Thyroid Diseases. Eur. Rev. Med. Pharm. Sci. 26, 1945–1951 (2022).
Bala, M. M. & Bala, K. A. Bone mineral density and complete blood count ratios in children and adolescents with obesity. Eur. Rev. Med Pharm. Sci. 26, 249–256 (2022).
Bala, M. M. & Bala, K. A. Association among complete blood count parameters, bone mineral density, and Cobb angle in cases of adolescent idiopathic scoliosis. Med Sci. Monit. 29, e940355 (2023).
Jürimäe, J. Interpretation and application of bone turnover markers in children and adolescents. Curr. Opin. Pediatr. 22, 494–500 (2010).
Du, X. et al. School-milk intervention trial enhances growth and bone mineral accretion in Chinese girls aged 10-12 years in Beijing. Br. J. Nutr. 92, 159–168 (2004).
Brett, N. R. et al. Vitamin D status and functional health outcomes in children aged 2-8 Y: A 6-Mo Vitamin D randomized controlled trial. Am. J. Clin. Nutr. 107, 355–364 (2018).
Cheng, T. et al. Tartrate-resistant acid phosphatase 5b is a potential biomarker for rheumatoid arthritis: a pilot study in Han Chinese. Chin. Med J. 127, 2894–2899 (2014).
Kaufmann, M. et al. Clinical utility of simultaneous quantitation of 25-Hydroxyvitamin D and 24,25-Dihydroxyvitamin D by LC-MS/MS involving Derivatization with DMEQ-Tad. J. Clin. Endocrinol. Metab. 99, 2567–2574 (2014).
Willett, W. & Stampfer, M. J. Total energy intake: implications for epidemiologic analyses. Am. J. Epidemiol. 124, 17–27 (1986).
McCullough, L. E. & Byrd, D. A. Total energy intake: implications for epidemiologic analyses. Am. J. Epidemiol. 192, 1801–1805 (2023).
Dixit, M., Poudel, S. B. & Yakar, S. Effects of GH/IGF AXIS ON BONE AND CARTILage. Mol. Cell Endocrinol. 519, 111052 (2021).
Üçler, R. et al. Evaluation of blood neutrophil to lymphocyte and platelet to lymphocyte ratios according to plasma glucose status and serum insulin-like growth Factor 1 levels in patients with Acromegaly. Hum. Exp. Toxicol. 35, 608–612 (2016).
Szydełko, J., Szydełko-Gorzkowicz, M. & Matyjaszek-Matuszek, B. Neutrophil-to-lymphocyte, platelet-to-lymphocyte ratios, and systemic immune-inflammation index as potential biomarkers of chronic inflammation in patients with newly diagnosed acromegaly: a single-centre study. J. Clin. Med. 10, 3997 (2021).
Juul, A. Serum lkevels of Insulin-Like Growth Factor I and its binding proteins in health and disease. Growth Horm. IGF Res. 13, 113–170 (2003).
Tang, Y. et al. Systemic Immune-Inflammation Index and bone mineral density in postmenopausal women: a cross-sectional Study of the National Health and Nutrition Examination Survey (NHANES) 2007-2018. Front Immunol. 13, 975400 (2022).
Yolaçan, H. & Guler, S. Inverse correlation between bone mineral density and systemic immune inflammation index in postmenopausal Turkish Women. Cureus 15, e37463 (2023).
Öztürk, Z. A. et al. Inverse Relationship between Neutrophil Lymphocyte Ratio (NLR) and Bone Mineral Density (BMD) in elderly people. Arch. Gerontol. Geriatr. 57, 81–85 (2013).
Liang, G. et al. Study on the Levels of 25-Hydroxy Vitamin D parathyroid hormone, and bone-specific alkaline phosphatase of children aged 0~10 years in Nanjing. Chin. J. Child Health Care. 17, 15–16+20.
Chan, E. L. et al. Age-related changes in bone density, serum parathyroid hormone, calcium absorption and other indices of bone metabolism in Chinese Women. Clin. Endocrinol 36, 375–381 (1992).
Fu, Q., Jilka, R. L., Manolagas, S. C. & O’Brien, C. A. Parathyroid hormone stimulates receptor Activator of Nfkappa B ligand and inhibits osteoprotegerin expression via protein kinase a activation of camp-response element-binding protein. J. Biol. Chem. 277, 48868–48875 (2002).
Toribio, R. E., Kohn, C. W., Capen, C. C. & Rosol, T. J. Parathyroid Hormone (PTH) Secretion, PTH mRNA and Calcium-Sensing Receptor mRNA Expression in Equine Parathyroid Cells, and Effects of Interleukin (IL)-1, IL-6, and Tumor Necrosis Factor-Alpha on Equine Parathyroid Cell Function. J. Mol. Endocrinol. 31, 609–620 (2003).
Silva, B. C., Costa, A. G., Cusano, N. E., Kousteni, S. & Bilezikian, J. P. Catabolic and anabolic actions of parathyroid hormone on the skeleton. J. Endocrinol. Invest 34, 801–810 (2011).
Tripathi, T. et al. Osteocalcin and Serum Insulin-Like Growth Factor-1 as biochemical skeletal maturity indicators. Prog. Orthod. 18, 30 (2017).
Esposito, S. et al. Vitamin D and growth hormone in children: a review of the current scientific knowledge. J. Transl. Med. 17, 87 (2019).
Acknowledgements
The authors would like to thank all research members involved in the data collection of the study.
Funding
This work was supported by the Fundamental Research Funds for the Central Universities (grant number lzujbky-2023-40).
Author information
Authors and Affiliations
Contributions
Y.H., X-Y.J., and X-Q.M. analyzed the data. C.W., C-Y.T., K-W.L., and X-G.L. checked the relevant literature. All authors contributed to the acquisition and interpretation of the data. Y.H. drafted the first version of the manuscript. All authors critically revised the manuscript for important intellectual content, ultimately approved the version to be published, and agreed to take responsibility for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Informed consent was given by the guardians of all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hu, Y., Jin, Xy., Mao, Xq. et al. Relationship between inflammatory indicators and bone mineral density in preschool children. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04665-y
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04665-y