Abstract
Background
Exclusive breastfeeding (EBF) rates at 6 months postpartum remain low globally and in Hong Kong. This prospective mixed-method study examined the barriers to and facilitators of sustaining EBF until 6 months postpartum.
Methods
Nine hundred forty-two pregnant women completed baseline and at least one of the five follow-up surveys: immediate (<7 days) (T1), 1 month (T2), 2 months (T3), 4 months (T4), and 6 months postpartum (T5). The response rates were 81.0% (T1), 69.9% (T2), 67.3% (T3), 65.8% (T4) and 81.4% (T5). Eighteen participants and 6 partners participated in either individual or focus group interviews at 6 months postpartum.
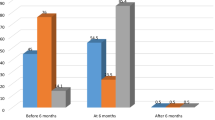
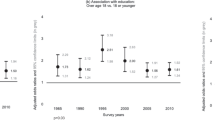
Results
The quantitative study found that mothers who worked full-time, had attained lower levels of education, lacked breastfeeding experience, and had caesarean sections were less likely to practise EBF at 6 months postpartum. In contrast, mother-in-law’s breastfeeding experience, higher breastfeeding intention and better breastfeeding knowledge were positively associated with EBF at 6 months postpartum. Qualitative data identified perceived insufficient breast milk and returning to work as the main barriers, while support from family was the key facilitator.
Conclusions
In addition to education and support for mothers, in order to sustain EBF, it is crucial to engage with family members and for workplaces to create more conducive environments.
Impact
-
This large-scale mixed methods cohort study describes mothers’ feeding practices and perspectives from the immediate postpartum period until 6 months.
-
Factors associated with EBF at 6 months included (1) mother and infant attributes, (2) workplace and employment, (3) family and community, and (4) health systems and services.
-
Policies and strategies extending to family members, workplace and health system will create a more conducive environment for sustaining EBF.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
World Health Organization. Breastfeeding. https://www.who.int/health-topics/breastfeeding#tab=tab_1 (2024).
Kramer, M. S. & Kakuma, R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst. Rev. 2012, Cd003517 (2012).
Duijts, L., Jaddoe, V. W., Hofman, A. & Moll, H. A. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics 126, e18–e25 (2010).
North, K., Gao, M., Allen, G. & Lee, A. C. C. Breastfeeding in a global context: epidemiology, impact, and future directions. Clin. Ther. 44, 228–244 (2022).
Sankar, M. J. et al. Optimal breastfeeding practices and infant and child mortality: a systematic review and meta-analysis. Acta Paediatr. 104, 3–13 (2015).
Harder, T., Bergmann, R., Kallischnigg, G. & Plagemann, A. Duration of breastfeeding and risk of overweight: a meta-analysis. Am. J. Epidemiol 162, 397–403 (2005).
Yan, J., Liu, L., Zhu, Y., Huang, G. & Wang, P. P. The association between breastfeeding and childhood obesity: a meta-analysis. BMC Public Health 14, 1267 (2014).
Belfort, M. B. et al. Infant feeding and childhood cognition at ages 3 and 7 years: effects of breastfeeding duration and exclusivity. JAMA Pediatr. 167, 836–844 (2013).
Wigg, N. R. et al. Does breastfeeding at six months predict cognitive development?. Aust. N. Z. J. Public Health 22, 232–236 (1998).
UNICEF. WHO/UNICEF discussion paper: the extension of the 2025 maternal, infant and young child nutrition targets to 2030. (2019).
Department of Health. Breastfeeding Survey 2021. https://www.fhs.gov.hk/english/reports/files/BF_survey_2021.pdf (2021).
Rollins, N. C. et al. Why invest, and what it will take to improve breastfeeding practices?. Lancet 387, 491–504 (2016).
Jama, A. et al. Exclusive breastfeeding for the first six months of life and its associated factors among children age 6-24 months in Burao district, Somaliland. Int. Breastfeed. J. 15, 5 (2020).
Odar Stough, C., Khalsa, A. S., Nabors, L. A., Merianos, A. L. & Peugh, J. Predictors of exclusive breastfeeding for 6 months in a national sample of US children. Am. J. Health Promot. 33, 48–56 (2018).
Santacruz-Salas, E. et al. Mothers’ expectations and factors influencing exclusive breastfeeding during the first 6 months. Int. J. Environ. Res. Public Health 17, 77 (2020).
Zielinska, M., Sobczak, A. & Hamulka, J. Breastfeeding knowledge and exclusive breastfeeding of infants in first six months of life. Roczniki Państwowego Zakładu Higieny 68, 51–59 (2017).
Meedya, S., Fahy, K. & Kable, A. Factors that positively influence breastfeeding duration to 6 months: a literature review. Women Birth 23, 135–145 (2010).
Bai, D. L., Fong, D. Y. T. & Tarrant, M. Factors associated with breastfeeding duration and exclusivity in mothers returning to paid employment postpartum. Matern Child. Health J. 19, 990–999 (2015).
Ku, C.-M. & Chow, S. K. Y. Factors influencing the practice of exclusive breastfeeding among Hong Kong Chinese women: a questionnaire survey. J. Clin. Nurs. 19, 2434–2445 (2010).
Loke, A. Y. & Chan, L. K. S. Maternal breastfeeding self-efficacy and the breastfeeding behaviors of newborns in the practice of exclusive breastfeeding. J. Obstet. Gynecol. Neonatal Nurs. 42, 672–684 (2013).
Creswell, J. W. & Creswell, J. D. Research Design: Qualitative, Quantitative and Mixed Methods Approaches 5th edn (SAGE Publications, Inc., 2018).
Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory (Prentice-Hall, Inc., 1986).
Bandura, A. Self-efficacy: toward a unifying theory of behavioral change. Psychol. Rev. 84, 191–215 (1977).
Peduzzi, P., Concato, J., Kemper, E., Holford, T. R. & Feinstein, A. R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 49, 1373–1379 (1996).
Palinkas, L. A. et al. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm. Policy Ment. Health 42, 533–544 (2015).
World Health Organization. Exclusive Breastfeeding for Optimal Growth, Development and Health of Infants. https://www.who.int/tools/elena/interventions/exclusive-breastfeeding (2023).
Sun, C.-Y. Effect of Breastfeeding Support Program on Continuous Breastfeeding in Employed Women. Master thesis, National Taipei University of Nursing and Health Sciences (2014).
Ho, Y.-J. & McGrath, J. M. A Chinese version of Iowa Infant Feeding Attitude Scale: reliability and validity assessment. Int. J. Nurs. Stud. 48, 475–478 (2011).
Lau, C. Y. et al. Development and measurement properties of the Chinese breastfeeding self-regulation questionnaire. Midwifery 44, 24–34 (2017).
Ip, W.-Y., Yeung, L.-S., Choi, K.-C., Chair, S.-Y. & Dennis, C.-L. Translation and validation of the Hong Kong Chinese version of the breastfeeding self-efficacy scale—short form. Res. Nurs. Health 35, 450–459 (2012).
Roig, A. O. et al. Factors associated to breastfeeding cessation before 6 months. Revista latino-Americana de enfermagem 18, 373–380 (2010).
Mangrio, E., Persson, K. & Bramhagen, A.-C. Sociodemographic, physical, mental and social factors in the cessation of breastfeeding before 6 months: a systematic review. Scand. J. Caring Sci. 32, 451–465 (2018).
De Roza, J. G. et al. Exclusive breastfeeding, breastfeeding self-efficacy and perception of milk supply among mothers in Singapore: a longitudinal study. Midwifery 79, 102532 (2019).
Zhu, H. X. et al. Logistic regression analysis on influencing factors of exclusive breastfeeding in 1918 pairs of mothers and infants [Article in Chinese]. Mat. Child Health Care China 34, 648–654 (2019).
Thomas, J. S. et al. Maternal knowledge, attitudes and self-efficacy in relation to intention to exclusively breastfeed among pregnant women in rural Bangladesh. Matern Child. Health J. 19, 49–57 (2015).
Hong Kong Department of Health. A Survey of Young Child Feeding in Hong Kong 2016. https://www.fhs.gov.hk/english/reports/files/young_child_feeding_summary.pdf (2018).
Huang, Y., Liu, Y., Yu, X.-Y. & Zeng, T.-Y. The rates and factors of perceived insufficient milk supply: a systematic review. Matern. Child Nutr. 18, e13255 (2022).
Shi, H. et al. Determinants of exclusive breastfeeding for the first six months in China: a cross-sectional study. Int. Breastfeed. J. 16, 40 (2021).
Zhang, Z., Zhu, Y., Zhang, L. & Wan, H. What factors influence exclusive breastfeeding based on the theory of planned behaviour. Midwifery 62, 177–182 (2018).
Gatti, L. Maternal perceptions of insufficient milk supply in breastfeeding. J. Nurs. Scholarsh. 40, 355–363 (2008).
Zhao, A. et al. Traditional postpartum customs in modern urban Chinese women and its association with dietary quality. Glob. Transit. 4, 82–89 (2022).
Chan, S. M., Nelson, E. A. S., Leung, S. S. F., Cheung, P. C. K. & Li, C. Y. Special postpartum dietary practices of Hong Kong Chinese women. Eur. J. Clin. Nutr. 54, 797–802 (2000).
Mak, S. W. Digitalised health, risk and motherhood: politics of infant feeding in post-colonial Hong Kong. Health Risk Soc. 17, 547–564 (2016).
Zahra, S., Monireh, A., Easa, M. & Susan, P. Successful breastfeeding mothers’ experiences of the difficulties of exclusive breastfeeding. Acta Med. Mediterr. 31, 1479–1487 (2015).
Adugnaw, E. et al. The median time to stopover exclusive breastfeeding among employed and unemployed mothers of infants aged 6–12 months in Ethiopia, 2019. Sci. Rep. 13, 6259 (2023).
Smith, J. P. et al. Workplace support, breastfeeding and health. Fam. Matters 83, 58–73 (2013).
Canaan, S., Lassen, A., Rosenbaum, P. & Steingrimsdottir, H. Maternity leave and paternity Leave: Evidence on the economic impact of legislative changes in high income countries. IZA Discussion Paper No. 15129 (2022).
Yan, C., Arijit, N. & Jody, H. Does extending the duration of legislated paid maternity leave improve breastfeeding practices? Evidence from 38 low-income and middle-income countries. BMJ Glob. Health 3, e001032 (2018).
Koksal, I., Acikgoz, A. & Cakirli, M. The effect of a father’s support on breastfeeding: a systematic review. Breastfeed. Med. 17, 711–722 (2022).
Flacking, R., Dykes, F. & Ewald, U. The influence of fathers’ socioeconomic status and paternity leave on breastfeeding duration: a population-based cohort study. Scand. J. Public Health 38, 337–343 (2010).
UNICEF. What is a Breastfeeding Friendly Workplace. https://www.sayyestobreastfeeding.hk/en-gb/work-place-info (2024).
Tarrant, M., Dodgson, J. E. & Choi, V. W. K. Becoming a role model: the breastfeeding trajectory of Hong Kong women breastfeeding longer than 6 months. Int. J. Nurs. Stud. 41, 535–546 (2004).
Mahesh, P. K. B. et al. Effectiveness of targeting fathers for breastfeeding promotion: systematic review and meta-analysis. BMC Public Health 18, 1140 (2018).
Zhao, Z.-H. et al. Co-parenting impact on breastfeeding: systematic review and meta-Analysis. Breastfeed. Med. 18, 431–448 (2023).
Wu, Q., Tang, N. & Wacharasin, C. Factors influencing exclusive breastfeeding for 6 months postpartum: a systematic review. Int. J. Nurs. Knowl. 33, 290–303 (2022).
Duan, Y. et al. What are the determinants of low exclusive breastfeeding prevalence in China? A cross-sectional study. Matern. Child Nutr. 18, e13324 (2022).
Foong, S. C., Tan, M. L., Foong, W. C., Ho, J. J. & Rahim, F. F. Comparing breastfeeding experiences between mothers spending the traditional Chinese confinement period in a confinement centre and those staying at home: a cohort study. Int. Breastfeed. J. 16, 4 (2021).
Al-Sahab, B., Lanes, A., Feldman, M. & Tamim, H. Prevalence and predictors of 6-month exclusive breastfeeding among Canadian women: a national survey. BMC Pediatr. 10, 20 (2010).
Hobbs, A. J., Mannion, C. A., McDonald, S. W., Brockway, M. & Tough, S. C. The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy Childbirth 16, 90 (2016).
Patil, D. S. et al. A mixed-methods systematic review on barriers to exclusive breastfeeding. Nutr. Health 26, 323–346 (2020).
Wen, J., Yu, G., Kong, Y., Liu, F. & Wei, H. An exploration of the breastfeeding behaviors of women after cesarean section: a qualitative study. Int. J. Nurs. Sci. 7, 419–426 (2020).
Chaplin, J., Kelly, J. & Kildea, S. Maternal perceptions of breastfeeding difficulty after caesarean section with regional anaesthesia: a qualitative study. Women Birth 29, 144–152 (2016).
Intiful, F., Osei, C., Steele-Dadzie, R., Nyarko, R. & Asante, M. Views of first-time expectant mothers on breastfeeding: a study in three health facilities in Accra, Ghana. Adv. Public Health. 2017, 4894026 (2017).
Zhang, Y., Jin, Y., Vereijken, C., Stahl, B. & Jiang, H. Breastfeeding experience, challenges and service demands among Chinese mothers: a qualitative study in two cities. Appetite 128, 263–270 (2018).
Hong Kong Census and Statistics Department. 2021 Population Census. https://www.censtatd.gov.hk/en/scode600.html (2024).
Acknowledgements
We would like to express our gratitude to Ms Carrie Cheung, Ling Chow and Angela Mak for their help with data collection, and to Dr Kai Chow Choi and Mr Jeffy Fung for their support in statistical analysis. We also express our sincere gratitude to all the mothers for their participation in this study.
Funding
This study was part of the research project ‘Commissioned Study on Mothers Barriers to Sustain Exclusive Breastfeeding in the First Six Months’ which was supported by the Health and Medical Research Fund, Health Bureau, The Government of the HKSAR.
Author information
Authors and Affiliations
Contributions
Ka Ming Chow: conceptualisation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, supervision, validation, visualisation, and writing—original draft. Alice Wai Yi Leung: data curation, formal analysis, and writing—original draft. Lai Ling Hui: conceptualisation, funding acquisition, methodology, and writing—review & editing. Karene Hoi Ting Yeung: conceptualisation, funding acquisition, methodology, and writing—review & editing. Esther Yuet Ying Lau: conceptualisation and writing—review & editing. Nigel C. Rollins: conceptualisation and writing—review & editing. E. Anthony S. Nelson: conceptualisation, funding acquisition, methodology, validation, and writing—review & editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent
Written patient consent was provided by all participants before enrollment.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chow, K.M., Leung, A.W.Y., Hui, L.L. et al. Factors associated with exclusive breastfeeding at 6 months postpartum: a prospective mixed-method cohort study. Pediatr Res (2026). https://doi.org/10.1038/s41390-025-04731-5
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41390-025-04731-5