Abstract
Study design
Exploratory clinical study.
Objectives
To localize the sites of conduction block in the spinal sensory and motor pathways for minimizing the level of surgical intervention despite MRI evidence of compression at several levels in degenerative cervical myelopathy (DCM).
Setting
Kochi Medical School Hospital, Japan.
Methods
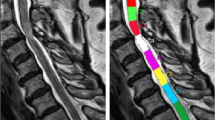
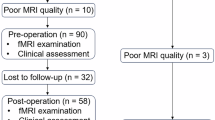
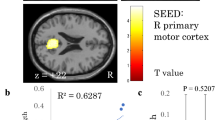
We analyzed 83 DCM patients (69 ± 12 years) who underwent serial intervertebral recording of both ascending (A-SCEPs) and descending spinal cord-evoked potentials (D-SCEPs) after epidural and transcranial stimulation, respectively, during surgery before decompression procedures. The site of conduction block was identified by an abrupt reduction of the negative peak accompanied by an enlargement of the initial-positive peak. T1-weighted MRI allowed quantitative assessments of cord compression in relation to the level of conduction block.
Results
The A-SCEP and D-SCEP studies revealed conduction blocks at the same single level in 78 patients (94%) and at two separate levels in five patients (6%) for MRI abnormalities extending to 3.1 ± 1.1 levels. The site of conduction block had intense cord compression on MRI with either the smallest (81%) or the second smallest (19%) anteroposterior diameter and cross-sectional area of the cord. Based on the SCEP findings, 44 patients were treated by a single-level (35) or a two-level (9) anterior operation for MRI abnormalities of 2.7 ± 1.1 levels.
Conclusions
Combined A-SCEP and D-SCEP studies served as useful additions to MRI in localizing the primary sites responsible for myelopathy, which helped exclude clinically silent compressions to minimize surgical intervention in 34 patients with anterior operation.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine. 2015;40:E675–93.
Kato F, Yukawa Y, Suda K, Yamagata M, Ueta T. Normal morphology, age-related changes and abnormal findings of the cervical spine. Part II: magnetic resonance imaging of over 1,200 asymptomatic subjects. Eur Spine J. 2012;21:1499–507.
Tani T, Ishida K, Ushida T, Yamamato H. Intraoperative electroneurography in the assessment of the level of operation for cervical spondylotic myelopathy in the elderly. J Bone Joint Surg. 2000;82:269–74.
Tani T, Ushida T, Taniguchi S, Kimura J. Age related shift in the primary sites of involvement in cervical spondylotic myelopathy from lower to upper levels. J Neurol Neurosurg Psychiatry. 2002;73:316–8.
Tadokoro N, Tani T, Ikeuchi M, Takemasa R, Kida K, Ikemoto T, et al Descending spinal cord evoked potentials in cervical spondylotic myelopathy: characteristic waveform changes seen at the lesion site. Clin Neurophysiol. 2014;125:202–7.
Japanese Orthopaedic Association. Scoring system (17-2) for cervical myelopathy. Nippon Seikeigeka Gakkai Zasshi. 1994;68:498.
Kimura J. Electrodiagnosis in diseases of nerve and muscle: principles and practice. 4th ed. New York, USA: Oxford University Press; 2013. p. 49–73.
Ikemoto T, Tani T, Taniguchi S, Ikeuchi M, Kimura J. Effects of experimental focal compression on excitability of human median motor axons. Clin Neurophysiol. 2009;120:342–7.
Kimura J. Electrodiagnosis in diseases of nerve and muscle: principles and practice. 4th ed. New York, USA: Oxford University Press; 2013. p. 288–96.
Tani T, Saito T, Kawasaki M, Tadokoro N, Kimura J. Spinal cord monitoring for high risk spinal surgery. In: Johari A, Luk KDK, Waddell JP, editors. Current progress in orthopedics. Maharashtra, Mumbai: Three Life Media; 2016. p. 232–53. Vol. 2, Chapter 13.
McDonald DB, Skinner S, Shils J, Yingling C. Intraoperative motor evoked potentia monitoring–a position statement by the American Society of Neurophysiological Monitoring. Clin Neurophysiol. 2013;124:2291–316.
Goodridge AE, Feasby TE, Ebers GC, Brown WF, Rice GP. Hand wasting due to mid-cervical spinal cord compression. Can J Neurol Sci. 1987;14:309–11.
Kameyama T, Hashizume Y, Sobue G Morphologic features of the normal human cadaveric spinal cord. Spine. 1996;21:1285–90.
Al-Mefty O, Harkey LH, Middleton TH, Smith RR, Fox JL. Myelopathic cervical spondylotic lesions demonstrated by magnetic resonance imaging. J Neurosurg. 1988;68:217–22.
Flanagan MN, Chung BU. Roentgenographic changes in 188 patients 10-20 years after discography and chemonucleolysis. Spine. 1986;11:444–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Tadokoro, N., Tani, T., Kida, K. et al. Localization of the primary sites of involvement in the spinal sensory and motor pathways for multilevel MRI abnormalities in degenerative cervical myelopathy. Spinal Cord 56, 117–125 (2018). https://doi.org/10.1038/s41393-017-0011-9
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41393-017-0011-9