Abstract
Study design
Retrospective observational cohort study.
Objectives
To describe outcomes, risk factors for complications, and relapse rates associated with the multimodal treatment approach for deep pressure ulcers (PUs) grade IV for the ischium, trochanter major, and sacral regions of patients with traumatic and non-traumatic spinal cord injury (SCI).
Setting
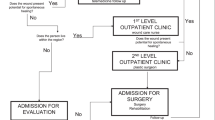
The settings comprised two spinal cord units within a maximum care hospital. The treatment of all patients followed the modified interdisciplinary “Basler treatment concept”.
Methods
We included all individuals with SCI with a first occurrence of PU grade IV in the buttocks area between August 2008 and December 2012 inclusive, with a maximum follow-up of 3 years. Descriptive, univariate, and bivariate analyses were undertaken, as were group comparisons.
Results
In 47 patients aged 18–87 years (mean age: 51 years) a total of 63 fasciocutaneous and myocutaneous flaps were performed. Wound healing was complete after a mean of 34 days (SD = 21). Postoperative mobilisation in a wheelchair was performed after a mean of 46 days (SD = 24). Delayed healing was reported in 18 patients (38%), and revision surgery was necessary in five patients (11%). ASIA impairment scale (AIS) A (p = .001), and male gender (p = .001) were identified as risk factors for delayed wound healing and prolonged inpatient stay.
Treatment-associated pneumonia occurred in four cases (11% of all patients, 25% of patients with tetraplegia). Patients were discharged when the time spent sitting in a wheelchair was 2 × 2 h per day; this occurred after a mean of 100 days (SD = 36). PU recurrence was observed in six cases (18%).
Conclusions
Our multimodal treatment concept was found to have complication rates comparable to those in the literature; additionally, this approach might be associated with lower recurrence rates with respect to the literature. To reduce high rates of pneumonia occurrence among patients with tetraplegia, preventive measures need to be established. Further evidence of the efficiency of this complex treatment approach for PU in individuals with SCI is needed.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Schryvers OI, Stranc MF, Nance PW. Surgical treatment of pressure ulcers: 20-year experience. Arch Phys Med Rehabil. 2000;81:1556–62.
Rieger U, Scheufler O, Schmid D, Zweifel-Schlatter M, Kalbermatten D, Pierer G. Die sechs Behandlungsprinzipien des Basler Dekubituskonzepts. Handchir Mikrochir Plast Chir. 2007;39:206–14.
Kruger EA, Pires M, Ngann Y, Sterling M, Rubayi S. Comprehensive management of pressure ulcers in spinal cord injury: current concepts and future trends. J Spinal Cord Med. 2013;36:572–85.
Srivastava A, Gupta A, Taly AB. Surgical management of pressure ulcers during inpatient neurologic rehabilitation: outcomes for patients with spinal cord disease. J Spinal Cord Med. 2009;32:125–31.
Stausberg J, Kiefer E. Classification of pressure ulcers: a systematic literature review. Stud Health Technol Inform. 2009;146:511–5.
National Pressure Ulcer Advisory Panel EPUAPaPP, Alliance PI. Prevention and treatment of pressure ulcers: quick reference guide. Perth: Cambridge Media; 2014.
Mak AF, Zhang M, Tam EW. Biomechanics of pressure ulcer in body tissues interacting with external forces during locomotion. Annu Rev Biomed Eng. 2010;12:29–53.
Chen Y, Devivo MJ, Jackson AB. Pressure ulcer prevalence in people with spinal cord injury: age-period-duration effects. Arch Phys Med Rehabil. 2005;86:1208–13.
Hartkopp A, Bronnum-Hansen H, Seidenschnur AM, Biering-Sorensen F. Survival and cause of death after traumatic spinal cord injury. A long-term epidemiological survey from Denmark. Spinal Cord. 1997;35:76–85.
Byrne DW, Salzberg CA. Major risk factors for pressure ulcers in the spinal cord disabled: a literature review. Spinal Cord. 1996;34:255–63.
Schubart JR, Hilgart M, Lyder C. Pressure ulcer prevention and management in spinal cord-injured adults: analysis of educational needs. Adv Skin Wound Care. 2008;21:322–9.
Sorensen JL, Jorgensen B, Gottrup F. Surgical treatment of pressure ulcers. Am J Surg. 2004;188:42–51.
Disa JJ, Carlton JM, Goldberg NH. Efficacy of operative cure in pressure sore patients. Plast Reconstr Surg. 1992;89:272–8.
Sundell B, Pentti A, Langensiold A. Surgical treatment of pressure ulcers in paraplegics. Acta Orthop Scand. 1967;38:532–42.
Braver SD. Surgical treatment of decubitus ulcers in paraplegic patients. Ohio State Med J. 1968;64:582–5.
Foster RD, Anthony JP, Mathes SJ, Hoffman WY. Ischial pressure sore coverage: a rationale for flap selection. Br J Plast Surg. 1997;50:374–9.
Parkash S, Banerjee S. The total gluteus maximus rotation and other gluteus maximus musculocutaneous flaps in the treatment of pressure ulcers. Br J Plast Surg. 1986;39:66–71.
Mandrekas AD, Mastorakos DP. The management of decubitus ulcers by musculocutaneous flaps: a five-year experience. Ann Plast Surg. 1992;28:167–74.
Cope C, Barry P, Hassall M, Barnett R, Richards M, Vandervord J. V-Y advancement hamstring myocutaneous island flap repair of ischial pressure ulcers. Aust N Z J Surg. 1995;65:412–6.
Paletta CE, Freedman B, Shehadi SI. The VY tensor fasciae latae musculocutaneous flap. Plast Reconstr Surg. 1989;83:852–7.
Nahai F. The tensor fascia lata flap. Clin Plast Surg. 1980;7:51–6.
Guihan M, Bombardier CH. Potentially modifiable risk factors among veterans with spinal cord injury hospitalized for severe pressure ulcers: a descriptive study. J Spinal Cord Med. 2012;35:240–50.
Marin J, Nixon J, Gorecki C. A systematic review of risk factors for the development and recurrence of pressure ulcers in people with spinal cord injuries. Spinal Cord. 2013;51:522–7.
Wettstein R, Tremp M, Baumberger M, Schaefer DJ, Kalbermatten DF. Local flap therapy for the treatment of pressure sore wounds. Int Wound J. 2015;12:572–6.
Lüscher NJ. Value of surgical treatment of decubitus ulcer in geriatric patients. Ther Umsch Rev Ther. 1991;48:341–6.
De Roche R. Störfall Decubitus—Handbuch zur gesundheitsökonomischen Bedeutung, Prävention, konservativen und chirurgischen Therapie. Rehab Basel. 2012;1:280.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39:165–228.
Kondrup J, Rasmussen HH, Hamberg O, Stanga Z. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22:321–36.
Devivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012;50:365–72.
Kato H, Inoue T, Torii S. A new postoperative management scheme for preventing sacral pressure sores in patients with spinal cord injuries. Ann Plast Surg. 1998;40:39–43.
Wilczweski P, Grimm D, Gianakis A, Gill B, Sarver W, McNett M. Risk factors associated with pressure ulcer development in critically ill traumatic spinal cord injury patients. J Trauma Nurs. 2012;19:5–10.
Ho CH, Powell HL, Collins JF, Bauman WA, Spungen AM. Poor nutrition is a relative contraindication to negative pressure wound therapy for pressure ulcers: preliminary observations in patients with spinal cord injury. Adv Skin Wound Care. 2010;23:508–16.
Foster RD, Anthony JP, Mathes SJ, Hoffman WY, Young D, Eshima I. Flap selection as a determinant of success in pressure sore coverage. Arch Surg. 1997;132:868–73.
Ljung AC, Stenius MC, Bjelak S, Lagergren JF. Surgery for pressure ulcers in spinal cord-injured patients following a structured treatment programme: a 10-year follow-up. Int Wound J. 2017;14:355–9.
Kierney PC, Engrav LH, Isik FF, Esselman PC, Cardenas DD, Rand RP. Results of 268 pressure sores in 158 patients managed jointly by plastic surgery and rehabilitation medicine. Plast Reconstr Surg. 1998;102:765–72.
Sameem M, Au M, Wood T, Farrokhyar F, Mahoney J. A systematic review of complication and recurrence rates of musculocutaneous, fasciocutaneous, and perforator-based flaps for treatment of pressure sores. Plast Reconstr Surg. 2012;130:67e–77e.
Tchanque-Fossuo CN, Kuzon WMJ. An evidence-based approach to pressure sores. Plast Reconstr Surg. 2011;127:932–9.
Coleman S, Gorecki C, Nelson EA, Closs SJ, Defloor T, Halfens R, et al. Patient risk factors for pressure ulcer development: systematic review. Int J Nurs Stud. 2013;50:974–1003.
Ash D. An exploration of the occurrence of pressure ulcers in a British spinal injuries unit. J Clin Nurs. 2002;11:470–8.
Eslami V, Saadat S, Habibi Arejan R, Vaccaro AR, Ghodsi SM, Rahimi-Movaghar V. Factors associated with the development of pressure ulcers after spinal cord injury. Spinal Cord. 2012;50:899–903.
Rabadi MH, Vincent AS. Do vascular risk factors contribute to the prevalence of pressure ulcer in veterans with spinal cord injury? J Spinal Cord Med. 2013;34:46–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kreutzträger, M., Voss, H., Scheel-Sailer, A. et al. Outcome analyses of a multimodal treatment approach for deep pressure ulcers in spinal cord injuries: a retrospective cohort study. Spinal Cord 56, 582–590 (2018). https://doi.org/10.1038/s41393-018-0065-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-018-0065-3
This article is cited by
-
The frequency of osteomyelitis after pressure injury in spinal cord injury: a systematic review and meta-analysis
Spinal Cord Series and Cases (2024)
-
Risk factors of major complications after flap surgery in the treatment of stage III and IV pressure injury in people with spinal cord injury/disorder: a retrospective cohort study
Spinal Cord (2024)
-
Effect of a computerized decision support system on the treatment approach of stage III or IV pressure injury in patients with spinal cord injury: a feasibility study
BMC Health Services Research (2023)
-
Multidisciplinary treatment protocol for ischiatic, sacral, trochanteric or other pressure injuries in people with spinal cord injury: a retrospective cohort study
Spinal Cord (2023)
-
Osteomyelitis and antibiotic treatment in patients with grade IV pressure injury and spinal cord lesion—a retrospective cohort study
Spinal Cord (2022)