Abstract
Study design
Prospective observational.
Aim
The aim of this study was to analyse changes in bladder and bowel management methods in persons with long-standing spinal cord injury (SCI).
Setting
Two spinal centres in UK.
Method
Data were collected through interviews and examinations between 1990 and 2010 in a sample of persons injured more than 20 years prior to 1990.
Results
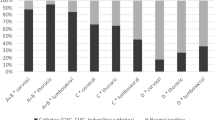
For the 85 participants who completed the 2010 follow-up, the mean age was 67.7 years and the mean duration of injury was 46.3 years, 80% were male, 37.7% had tetraplegia AIS grade A, B, or C, 44.7% paraplegia AIS A, B, or C, and 17.6% an AIS D grade regardless of level. In all, 50.6% reported having changed their bladder method, 63.1% their bowel method, and 40.5% both methods since they enroled in the study. The reasons for change were a combination of medical and practical. In men, condom drainage remained the most frequent bladder method, and in women, suprapubic catheter replaced straining/expressing as the most frequent method. The use of condom drainage and straining/expressing bladder methods decreased, whereas the use of suprapubic and intermittent catheters increased. Manual evacuation remained the most frequent bowel management method. The percentage of participants on spontaneous/voluntary bowel emptying, straining and medications alone decreased, whereas the use of colostomy and transanal irrigation increased over time.
Conclusions
More than half the sample, all living with SCI for more than 40 years, required change in their bladder and bowel management methods, for either medical or practical reasons. Regular follow-ups ensure adequate change of method if/when needed.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Sekar P, Wallace DD, Waites KB, DeVivo MJ, Lloyd LK, Stover SL, et al. Comparison of long-term renal function after spinal cord injury using different urinary management methods. Arch Phys Med Rehabil. 1997;78:992–7.
Drake MJ, Cortina-Borja M, Savic G, Charlifue SW, Gardner BP. Prospective evaluation of urological effects of aging in chronic spinal cord injury by method of bladder management. Neurourol Urodyn. 2005;24:111–6.
Savic G, Charlifue S, Glass C, Soni BM, Gerhart KA, Jamous MA. British ageing with SCI study: changes in physical and psychosocial outcomes over time. Top Spinal Cord Inj Rehabil. 2010;15:41–53.
Liu CW, Huang CC, Yang YH, Chen SC, Weng MC, Huang MH. Relationship between neurogenic bowel dysfunction and health-related quality of life in persons with spinal cord injury. J Rehabil Med. 2009;41:35–40.
Menter R, Weitzenkamp D, Cooper D, Bingley J, Charlifue S, Whiteneck G. Bowel management outcomes in individuals with long-term spinal cord injuries. Spinal Cord. 1997;35:608–12.
Faaborg PM, Christensen P, Finnerup N, Laurberg S, Krogh K. The pattern of colorectal dysfunction changes with time since spinal cord injury. Spinal Cord. 2008;46:234–8.
Coggrave M, Norton C, Wilson-Barnett J. Management of neurogenic bowel dysfunction in the community after spinal cord injury: a postal survey in the United Kingdom. Spinal Cord. 2009;47:323–30. quiz 331-3
Whiteneck G, Charlifue S, Frankel H, Fraser M, Gardner B, Gerhart K, et al. Mortality, morbidity and psychosocial outcomes of persons spinal cord injured more than 20 years ago. Paraplegia . 1992;30:617–30.
American Spinal Injury Association. International Standards for Neurological Classification of Spinal Cord Injury. Atlanta, GA: American Spinal Injury Association; 2015 (revised 2011).
Hansen RB, Biering-SorensenF, Kristensen JK. Bladder emptying over a period of 10–45 years after a traumatic spinal cord injury. Spinal Cord. 2004;42:631–7.
Rabadi MH, Aston C. Complications and urologic risks of neurogenic bladder in veterans with traumatic spinal cord injury. Spinal Cord. 2015;53:200–3.
Adriaansen JJ, van Asbeck FW, Tepper M, Faber WX, Visser-Meily JM, de Kort LM, et al. Bladder-emptying methods, neurogenic lower urinary tract dysfunction and impact on quality of life in people with long-term spinal cord injury. J Spinal Cord Med. 2017;40:43–53.
Krebs J, Wöllner J, Pannek J. Risk factors for symptomatic urinary tract infections in individuals with chronic neurogenic lower urinary tract dysfunction. Spinal Cord. 2016;54:682–6.
El-Masri WS, Chong T, Kyriakider AE, Wang D. Long-term follow-up study of outcomes of bladder management in spinal cord injury patients under the care of the Midlands Centre for Spinal Injuries in Oswestry. Spinal Cord. 2012;50:14–21.
Coggrave MJ, Ingram RM, Gardner BP, Norton CS. The impact of stoma for bowel management after spinal cord injury. Spinal Cord. 2012;50:848–52.
Christensen P, Bazzocchi G, Coggrave M, Abel R, Hultling C, Krogh K, et al. A randomized, controlled trial of transanal irrigation versus conservative bowel management in spinal cord-injured patients. Gastroenterology. 2006;131:738–47.
Christensen P, Bazzocchi G, Coggrave M, Abel R, Hulting C, Krogh K, et al. Outcome of transanal irrigation for bowel dysfunction in patients with spinal cord injury. J Spinal Cord Med. 2008;31:560–7.
Nielsen SD, Faaborg PM, Finnerup NB, Christensen P, Krogh K. Ageing with neurogenic bowel dysfunction. Spinal Cord. 2017;55:769–73.
Cameron AP, Rodriguez GM, Gursky A, He C, Clemens JQ, Stoffel JT. The severity of bowel dysfunction in patients with neurogenic bladder. J Urol. 2015;194:1336–41.
Martinez L, Neshatian L, Khavari R. Neurogenic bowel dysfunction in patients with neurogenic bladder. Curr Bladder Dysfunct Rep. 2016;11:334–40.
Acknowledgements
We authors thank all the participants for taking part in the study, and staff at the collaborating spinal centres at Stoke Mandeville and Southport Hospitals, UK. Over the years, the study was financially supported by the following funders: 1990 and 1996—National Institute on Disability and Rehabilitation Research (NIDRR), USA; 1993—Centers for Disease Control and Prevention (CDC), USA; 1999 and 2002—Ontario Neurotrauma Foundation, Canada; 2006—Buckinghamshire Hospitals NHS Trust Charitable Spinal Fund, UK; David Tolkien Trust Fund, UK; Southport and Ormskirk Hospital Spinal Injuries Centre Endowment Fund, UK; 2010—Buckinghamshire Healthcare NHS Trust Charitable Spinal Fund, UK and Ann Masson Legacy for Spinal Research Fund, UK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Savic, G., Frankel, H.L., Jamous, M.A. et al. Long-term bladder and bowel management after spinal cord injury: a 20-year longitudinal study. Spinal Cord 56, 575–581 (2018). https://doi.org/10.1038/s41393-018-0072-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-018-0072-4
This article is cited by
-
Priorities, needs and willingness of use of nerve stimulation devices for bladder and bowel function in people with spinal cord injury (SCI): an Australian survey
Spinal Cord Series and Cases (2024)
-
Safety of ultrasound-guided percutaneous suprapubic catheter insertion in spinal cord injury patients
Spinal Cord Series and Cases (2024)
-
Colostomy may offer hope in improving quality of life: a phenomenological qualitative study with patients dependent on a wheelchair
Quality of Life Research (2023)
-
Neurogenic Bowel: Traditional Approaches and Clinical Pearls
Current Physical Medicine and Rehabilitation Reports (2020)
-
Urinary tract infections and bladder management over the first year after discharge from inpatient rehabilitation
Spinal Cord Series and Cases (2018)