Abstract
Study design
Retrospective data collection and patient-reported outcome measures.
Objectives
To investigate surgical outcome, complications, and patient satisfaction in patients with chronic SCI and symptomatic post-traumatic progressive myelopathy (PPM) who underwent neurosurgical untethering and/or spinal cord cyst drainage with the aim of preventing further neurological deterioration.
Setting
Single-center study at an academic neurosurgery department.
Methods
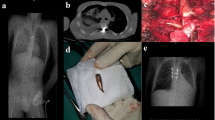
All SCI patients who underwent neurosurgery between 1996 and 2013 were retrospectively included. All medical charts and the treating surgeon’s operative reports were reviewed to identify surgical indications, surgical technique, and post-operative complications. A questionnaire and an EQ-5D-instrument were used to assess patient's self-described health status and satisfaction at long-term follow-up.
Results
Fifty-two patients (43 men, 9 women) were identified, of whom five were dead and one was lost to follow-up. Main indications for surgery were pain (54%), motor (37%), or sensory (8%) impairment, and spasticity (2.0%). Overall complications were rare (8%). At follow-up, the subjectively perceived outcome was improved in 24 and remained unchanged in 21 patients. Thus, the surgical aim was met in 87% of patients. Of the 46 eligible patients, 38 responded to the questionnaire of whom 65% were satisfied with the surgical results. Patients with cervical lesions were more satisfied with the surgical treatment than patients with thoracic/thoracolumbar lesions (p = 0.05).
Conclusions
Neurosurgical untethering and/or cyst drainage in chronic SCI patients and PPM resulted in a high degree of patient satisfaction, particularly in cervical SCI patients with minimal complications.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Dell’Anno MT, Strittmatter SM. Rewiring the spinal cord: direct and indirect strategies. Neurosci Lett. 2017;652:25–34.
Nandoe Tewarie RD, Hurtado A, Bartels RH, Grotenhuis JA, Oudega M. A clinical perspective of spinal cord injury. NeuroRehabilitation. 2010;27:129–39.
Steeves JD, Kramer JK, Fawcett JW, Cragg J, Lammertse DP, Blight AR, et al. Extent of spontaneous motor recovery after traumatic cervical sensorimotor complete spinal cord injury. Spinal Cord. 2011;49:257–65.
Falci SP, Indeck C, Lammertse DP. Posttraumatic spinal cord tethering and syringomyelia: surgical treatment and long-term outcome. J Neurosurg Spine. 2009;11:445–60.
Wyndaele M, Wyndaele JJ. Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey? Spinal Cord. 2006;44:523–9.
Lee TT, Alameda GJ, Camilo E, Green BA. Surgical treatment of post-traumatic myelopathy associated with syringomyelia. Spine. 2001;26:S119–27.
Schurch B, Wichmann W, Rossier AB. Post-traumatic syringomyelia (cystic myelopathy): a prospective study of 449 patients with spinal cord injury. J Neurol Neurosurg Psychiatry. 1996;60:61–7.
Edgar R, Quail P. Progressive post-traumatic cystic and non-cystic myelopathy. Br J Neurosurg. 1994;8:7–22.
Biyani A, el Masry WS. Post-traumatic syringomyelia: a review of the literature. Paraplegia. 1994;32:723–31.
el Masry WS, Biyani A. Incidence, management, and outcome of post-traumatic syringomyelia. In memory of Mr Bernard Williams. J Neurol Neurosurg Psychiatry. 1996;60:141–6.
Lee TT, Alameda GJ, Gromelski EB, Green BA. Outcome after surgical treatment of progressive posttraumatic cystic myelopathy. J Neurosurg. 2000;92:149–54.
Holtz A, Levi R. Spinal cord injury. Oxford University Press; Oxford, England; 2010.
Adelstein LJ. The surgical treatment of syringomyelia. Am J Surg. 1938;XL:384–95.
Aghakhani N, Baussart B, David P, Lacroix C, Benoudiba F, Tadie M, et al. Surgical treatment of posttraumatic syringomyelia. Neurosurgery. 2010;66:1120–7.
Austin JW, Afshar M, Fehlings MG. The relationship between localized subarachnoid inflammation and parenchymal pathophysiology after spinal cord injury. J Neurotrauma. 2012;29:1838–49.
Klekamp J. Treatment of posttraumatic syringomyelia. J Neurosurg Spine. 2012;17:199–211.
Rossier AB, Foo D, Shillito J, Dyro FM. Posttraumatic cervical syringomyelia. Incidence, clinical presentation, electrophysiological studies, syrinx protein and results of conservative and operative treatment. Brain. 1985;108:439–61.
Greitz D. Unraveling the riddle of syringomyelia. Neurosurg Rev. 2006;29:251–63.
Williams B. Pathogenesis of post-traumatic syringomyelia. Br J Neurosurg. 1992;6:517–20.
Bonfield CM, Levi AD, Arnold PM, Okonkwo DO. Surgical management of post-traumatic syringomyelia. Spine. 2010;35:S245–58.
Krebs J, Koch HG, Hartmann K, Frotzler A. The characteristics of posttraumatic syringomyelia. Spinal Cord. 2016;54:463–6.
Ewelt C, Stalder S, Steiger HJ, Hildebrandt G, Heilbronner R. Impact of cordectomy as a treatment option for posttraumatic and non-posttraumatic syringomyelia with tethered cord syndrome and myelopathy. J Neurosurg Spine. 2010;13:193–9.
Hayashi T, Ueta T, Kubo M, Maeda T, Shiba K. Subarachnoid-subarachnoid bypass: a new surgical technique for posttraumatic syringomyelia. J Neurosurg Spine. 2013;18:382–7.
Sgouros S, Williams B. A critical appraisal of drainage in syringomyelia. J Neurosurg. 1995;82:1–10.
EuroQolGroup. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208.
Lee TT, Arias JM, Andrus HL, Quencer RM, Falcone SF, Green BA. Progressive posttraumatic myelomalacic myelopathy: treatment with untethering and expansive duraplasty. J Neurosurg. 1997;86:624–8.
Grace PM, Hutchinson MR, Maier SF, Watkins LR. Pathological pain and the neuroimmune interface. Nat Rev Immunol. 2014;14:217–31.
Grau JW, Huang YJ, Turtle JD, Strain MM, Miranda RC, Garraway SM, et al. When pain hurts: nociceptive stimulation induces a state of maladaptive plasticity and impairs recovery after spinal cord injury. J Neurotrauma. 2017;34:1873–90.
Vernon JD, Silver JR, Symon L. Post-traumatic syringomyelia: the results of surgery. Paraplegia. 1983;21:37–46.
Klekamp J, Batzdorf U, Samii M, Bothe HW. Treatment of syringomyelia associated with arachnoid scarring caused by arachnoiditis or trauma. J Neurosurg. 1997;86:233–40.
Ghobrial GM, Dalyai RT, Maltenfort MG, Prasad SK, Harrop JS, Sharan AD. Arachnolysis or cerebrospinal fluid diversion for adult-onset syringomyelia? A systematic review of the literature. World Neurosurg. 2015;83:829–35.
Karam Y, Hitchon PW, Mhanna NE, He W, Noeller J. Post-traumatic syringomyelia: outcome predictors. Clin Neurol Neurosurg. 2014;124:44–50.
Acknowledgements
This study received funds from Uppsala University Hospital (to NM and UH) and the Swedish Research Council and from Personskadeförbundet RTP (to NM).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Holmström, U., Tsitsopoulos, P.P., Flygt, H. et al. Neurosurgical untethering with or without syrinx drainage results in high patient satisfaction and favorable clinical outcome in post-traumatic myelopathy patients. Spinal Cord 56, 873–882 (2018). https://doi.org/10.1038/s41393-018-0094-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-018-0094-y
This article is cited by
-
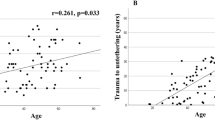
Spinal cord tethering and syringomyelia after trauma: impact of age and surgical outcome
Scientific Reports (2023)
-
Long-term outcome following surgical treatment of posttraumatic tethered cord syndrome: a retrospective population-based cohort study
Spinal Cord (2022)
-
Treatment of posttraumatic syringomyelia: evidence from a systematic review
Acta Neurochirurgica (2020)
-
Cerebrospinal fluid levels of GFAP and pNF-H are elevated in patients with chronic spinal cord injury and neurological deterioration
Acta Neurochirurgica (2020)