Abstract
Study design
Exploratory research
Objectives
Cutaneous silent periods (CSPs) that reflect the inhibitory spinal cord reflex, can sensitively detect spinal cord dysfunction, and contribute to the diagnosis of degenerative cervical myelopathy (DCM). However, CSP changes after DCM surgery related to functional improvement have not been reported.
Setting
University hospital in Nankoku, Japan
Methods
CSP recorded at four time points—before surgery, 3, 6, 12 months after surgery—were investigated in 31 hands of 16 DCM patients. CSPs were categorized as follows: normal, delayed onset latency, shortened duration, onset delay with shortened duration, and absent CSP. Myelopathic symptoms were evaluated by the Japanese Orthopaedic Association score (JOA score).
Results
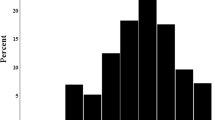
Normal CSPs were observed in five hands (16%) before surgery and six hands (19%) twelve months after surgery (P > 0.05). Either onset delay or shortened duration or both were observed in 18 hands (58%) before surgery and 16 hands (52%) twelve months after surgery (P > 0.05). Absent CSPs were observed in eight hands (26%) before surgery and nine hands (29%) twelve months after surgery (P > 0.05). Measured values of onset latency and duration also did not change throughout the study period (P > 0.05). On the other hand, JOA scores improved after surgery. (P = 0.003).
Conclusions
CSP abnormalities persisted after surgery in most cases, indicating irreversible damage of the intramedullary reflex circuit. JOA score recovery without CSP recovery provides insight into postoperative neural recovery in DCM.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data archiving
The datasets generated and/or analyzed during the current study are available from the corresponding author upon request.
References
Nouri A, Tetreault L, Dalzell K, Zamorano JJ, Fehlings MG. The relationship between preoperative clinical presentation and quantitative magnetic resonance imaging features in patients with degenerative cervical myelopathy. Neurosurgery. 2017;80:121–8.
Tetreault L, Kopjar B, Cote P, Arnold P, Fehlings MG. A clinical prediction rule for functional outcomes in patients undergoing surgery for degenerative cervical myelopathy: analysis of an international prospective multicenter data set of 757 subjects. J bone Jt Surg Am Vol. 2015;97:2038–46.
Kato F, Yukawa Y, Suda K, Yamagata M, Ueta T. Normal morphology, age-related changes and abnormal findings of the cervical spine. Part II: Magnetic resonance imaging of over 1,200 asymptomatic subjects. Eur Spine J. 2012;21:1499–507.
Leis AA, Kofler M. Silent period. In: Aminoff MJ and Daroff RB, editors. Encyclopedia of the neurological sciences, 2nd ed., Vol. 4. Oxford: Academic Press; 2014. p. 164–8.
Roser F, Ebner FH, Liebsch M, Dietz K, Tatagiba M. A new concept in the electrophysiological evaluation of syringomyelia. J Neurosurg Spine. 2008;8:517–23.
Stetkarova I, Kofler M. Cutaneous silent periods in the assessment of mild cervical spondylotic myelopathy. Spine. 2009;34:34–42.
Kofler M, Kumru H, Stetkarova I, Schindler C, Fuhr P. Muscle force up to 50% of maximum does not affect cutaneous silent periods in thenar muscles. Clin Neurophysiol. 2007;118:2025–30.
Akutagawa T, Tani T, Kida K, Tadokoro N, Enoki H, Nagano Y, et al. A new method for characterizing hand dysfunction in cervical spondylotic myelopathy: a preliminary study. Spinal Cord. 2016;54:221–5.
Kofler M, Kronenberg MF, Brenneis C, Felber A, Saltuari L. Cutaneous silent periods in intramedullary spinal cord lesions. J Neurol Sci. 2003;216:67–79.
Pullman SL, Ford B, Elibol B, Uncini A, Su PC, Fahn S. Cutaneous electromyographic silent period findings in brachial dystonia. Neurology. 1996;46:503–8.
Kofler M. Functional organization of exteroceptive inhibition following nociceptive electrical fingertip stimulation in humans. Clin Neurophysiol. 2003;114:973–80.
Lo YL, Tan YE, Dan YF, Leoh TH, Tan SB, Tan CT, et al. Cutaneous silent periods in the evaluation of cord compression in cervical spondylosis. J Neurol. 2007;254:14–9.
Chiba T, Konoeda F, Higashihara M, Kamiya H, Oishi C, Hatanaka Y, et al. C8 and T1 innervation of forearm muscles. Clin Neurophysiol. 2015;126:837–42.
Japanese Orthopaedic Association. Japanese Orthopaedic Association scoring system for cervical myelopathy (17-2 version and 100 version). Nippon Seikeigeka Gakkai Zasshi 1994;68:490–503.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48:452–8.
Leis AA, Kofler M, Stetkarova I, Stokic DS. The cutaneous silent period is preserved in cervical radiculopathy: significance for the diagnosis of cervical myelopathy. Eur Spine J. 2011;20:236–9.
Vasko P, Bocek V, Mencl L, Haninec P, Stetkarova I. Preserved cutaneous silent period in cervical root avulsion. J spinal cord Med. 2017;40:175–80.
Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine. 2015;40:E675–93.
Ulrich A, Min K, Curt A. High sensitivity of contact-heat evoked potentials in “snake-eye” appearance myelopathy. Clin Neurophysiol. 2015;126:1994–2003.
Tetreault L, Nouri A, Kopjar B, Cote P, Fehlings MG. The minimum clinically important difference of the modified Japanese Orthopaedic Association Scale in patients with degenerative cervical myelopathy. Spine. 2015;40:1653–9.
Nakanishi K, Tanaka N, Kamei N, Ohta R, Fujioka Y, Hiramatsu T, et al. Electrophysiological evidence of functional improvement in the corticospinal tract after laminoplasty in patients with cervical compressive myelopathy: clinical article. J Neurosurg Spine. 2014;21:210–6.
Ishida K, Tani T, Ushida T, Zinchk V, Yamamoto H. Recovery of spinal cord conduction after surgical decompression for cervical spondylotic myelopathy: serial somatosensory evoked potential studies. Am J Phys Med Rehabil / Assoc Acad Physiatr. 2003;82:130–6.
Zdunczyk A, Schwarzer V, Mikhailov M, Bagley B, Rosenstock T, Picht T, et al. The corticospinal reserve capacity: reorganization of motor area and excitability as a novel pathophysiological concept in cervical myelopathy. Neurosurgery. 2018;83:810–8.
Kofler M, Leis AA, Valls-Sole J. Cutaneous silent periods - Part 1: Update on physiological mechanisms. Clin Neurophysiol. 2019;130:588–603.
Floeter MK. Cutaneous silent periods. Muscle Nerve. 2003;28:391–401.
Velstra IM, Fellinghauer C, Abel R, Kalsi-Ryan S, Rupp R, Curt A. The graded and redefined assessment of strength, sensibility, and prehension version 2 provides interval measure properties. J Neurotrauma. 2018;35:854–63.
Author information
Authors and Affiliations
Contributions
NT contributed to the planning of this research project, data collection, data analysis and was the main author of this manuscript. KK, YK, MK, RT and MI contributed to the planning of the project, data analysis and revision of the manuscript.
Corresponding author
Ethics declarations
Statement of ethics
The participants in this prospective study provided informed consent, and this study was approved by the institutional review board (study no. ERB-102734).
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tadokoro, N., Kiyasu, K., Kasai, Y. et al. Discrepancy between functional recovery and cutaneous silent period change in surgically treated degenerative cervical myelopathy: a prospective pilot study. Spinal Cord 57, 1076–1083 (2019). https://doi.org/10.1038/s41393-019-0314-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-019-0314-0
This article is cited by
-
Neurophysiologic evaluation of patients with cervical spondylotic myelopathy
The Egyptian Journal of Neurology, Psychiatry and Neurosurgery (2022)
-
Duration and reliability of the silent period in individuals with spinal cord injury
Spinal Cord (2021)