Abstract
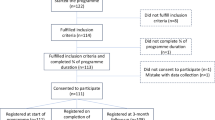
Study design
A quasi-experimental, pretest–posttest design.
Objectives
To identify acute changes in the supraspinatus and biceps tendon following fatiguing wheelchair propulsion and to associate tendon changes with risk factors associated with shoulder pain in persons with spinal cord injury (SCI).
Setting
Biomechanical laboratory Swiss Paraplegic Research.
Methods
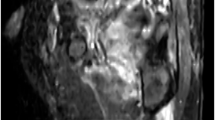
A population-based sample of 50 wheelchair users with SCI at lesion level T2 or below participated. Fatigue was measured by using the rate of perceived exertion and heart rate. Linear regression techniques were used to assess the association between the dependent and independent variables. Dependent variables included absolute differences in supraspinatus and biceps tendon thickness, contrast, and echogenicity ratio assessed with ultrasound before and after a fatiguing wheelchair propulsion intervention. Independent variables included susceptibility to fatigue (Yes/No), the acromio-humeral distance, sex, time since injury, activity levels, and body weight.
Results
A reduction in supraspinatus tendon thickness after fatiguing wheelchair propulsion (–1.39 mm; 95% CI: –2.28; –0.51) was identified after controlling for all potential confounders. Females who fatigued (n = 4) displayed a greater reduction in supraspinatus tendon thickness as compared with those who did not fatigue (n = 7). In contrast, higher body weight was associated with an increase in supraspinatus tendon thickness and a greater acromio-humeral distance before the intervention was associated with an increase in biceps tendon thickness.
Conclusions
Acute changes in the supraspinatus and biceps tendon after fatiguing wheelchair propulsion may explain the high prevalence of tendon injuries in this population. Future research should determine the consequences of tendon changes and its relationship to tendinopathy.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Veeger HEJ, van der Woude LHV, Rozendal RH. Load on the upper extremity in manual wheelchair propulsion. J Electromyogr Kinesiol. 1991;1:270–80.
Gutierrez DD, Thompson L, Kemp B, Mulroy SJ. The relationship of shoulder pain intensity to quality of life, physical activity, and community participation in persons with paraplegia. J Spinal Cord Med. 2007;30:251–5.
Bossuyt FM, Arnet U, Brinkhof MWG, Eriks-Hoogland I, Lay V, Muller R, et al. Shoulder pain in the swiss spinal cord injury community: Prevalence and associated factors. Disabil Rehabil. 2018;40:798–805.
Michener LA, McClure PW, Karduna AR. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin Biomech (Bristol, Avon). 2003;18:369–79.
Brose SW, Boninger ML, Fullerton B, McCann T, Collinger JL, Impink BG, et al. Shoulder ultrasound abnormalities, physical examination findings, and pain in manual wheelchair users with spinal cord injury. Arch Phys Med Rehabil. 2008;89:2086–93.
Morrow MM, Kaufman KR, An KN. Scapula kinematics and associated impingement risk in manual wheelchair users during propulsion and a weight relief lift. Clin Biomech (Bristol, Avon). 2011;26:352–7.
Mulroy SJ, Gronley JK, Newsam CJ, Perry J. Electromyographic activity of shoulder muscles during wheelchair propulsion by paraplegic persons. Arch Phys Med Rehabil. 1996;77:187–93.
Enoka RM, Duchateau J. Translating fatigue to human performance. Med Sci Sports Exerc. 2016;48:2228–38.
Bossuyt FM, Arnet U, Cools A, Rigot S, de Vries W, Eriks-Hoogland I, et al. Compensation strategies in response to fatiguing propulsion in wheelchair users: implications for shoulder injury risk. Am J Phys Med Rehabil. 2019. https://doi.org/10.1097/PHM.0000000000001267. [Epub ahead of print].
Maganaris CN, Chatzistergos P, Reeves ND, Narici MV. Quantification of internal stress-strain fields in human tendon: unraveling the mechanisms that underlie regional tendon adaptations and mal-adaptations to mechanical loading and the effectiveness of therapeutic eccentric exercise. Front Physiol. 2017;8:91.
Tardioli A, Malliaras P, Maffulli N. Immediate and short-term effects of exercise on tendon structure: biochemical, biomechanical and imaging responses. Br Med Bull. 2012;103:169–202.
Arya S, Kulig K. Tendinopathy alters mechanical and material properties of the achilles tendon. J Appl Physiol (1985) 2010;108:670–5.
Allen GM. Shoulder ultrasound imaging-integrating anatomy, biomechanics and disease processes. Eur J Radio. 2008;68:137–46.
Xu Y, Murrell GAC. The basic science of tendinopathy. Clin Orthop Rel Res. 2008;466:1528–38.
Collinger JL, Fullerton B, Impink BG, Koontz AM, Boninger ML. Validation of grayscale-based quantitative ultrasound in manual wheelchair users: Relationship to established clinical measures of shoulder pathology. Am J Phys Med Rehabil. 2010;89:390–400.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (strobe) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7.
Brinkhof MW, Fekete C, Chamberlain JD, Post MW, Gemperli A. Swiss national community survey on functioning after spinal cord injury: Protocol, characteristics of participants and determinants of non-response. J Rehabil Med. 2016;48:120–30.
van Drongelen S, Boninger ML, Impink BG, Khalaf T. Ultrasound imaging of acute biceps tendon changes after wheelchair sports. Arch Phys Med Rehabil. 2007;88:381–5.
Collinger JL, Impink BG, Ozawa H, Boninger ML. Effect of an intense wheelchair propulsion task on quantitative ultrasound of shoulder tendons. PM R. 2010;2:920–5.
Collinger JL, Gagnon D, Jacobson J, Impink BG, Boninger ML. Reliability of quantitative ultrasound measures of the biceps and supraspinatus tendons. Acad Radio. 2009;16:1424–32.
Mackenzie TA, Bdaiwi AH, Herrington L, Cools A. Inter-rater reliability of real-time ultrasound to measure acromiohumeral distance. PM R. 2016;8:629–34.
Washburn RA, Zhu W, McAuley E, Frogley M, Figoni SF. The physical activity scale for individuals with physical disabilities: development and evaluation. Arch Phys Med Rehabil. 2002;83:193–200.
van der Ploeg HP, Streppel KR, van der Beek AJ, van der Woude LH, Vollenbroek-Hutten M, van Mechelen W. The physical activity scale for individuals with physical disabilities: test-retest reliability and comparison with an accelerometer. J Phys Act Health. 2007;4:96–100.
Borg G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health. 1990;16:55–8.
Portney LG, Watkins MP. Foundations of clinical research: application to practice. Stamford: Appleton & Lange; 2000.
Magnusson SP, Narici MV, Maganaris CN, Kjaer M. Human tendon behaviour and adaptation, in vivo. J Physiol. 2008;586:71–81.
Pearson SJ, Engel AJ, Bashford GR. Changes in tendon spatial frequency parameters with loading. J Biomech. 2017;57:136–40.
Maganaris CN, Baltzopoulos V, Sargeant AJ. Repeated contractions alter the geometry of human skeletal muscle. J Appl Physiol. 2002;93:2089–94.
Kubo K, Kanehisa H, Fukunaga T. Gender differences in the viscoelastic properties of tendon structures. Eur J Appl Physiol. 2003;88:520–6.
Miller BF, Hansen M, Olesen JL, Schwarz P, Babraj JA, Smith K, et al. Tendon collagen synthesis at rest and after exercise in women. J Appl Physiol. 2006;102:541–6.
Cook JL, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med. 2009;43:409–16.
Paralyzed Veterans of America Consortium for Spinal Cord M. Preservation of upper limb function following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2005;28:434–70.
Fournier Belley A, Gagnon DH, Routhier F, Roy JS. Ultrasonographic measures of the acromiohumeral distance and supraspinatus tendon thickness in manual wheelchair users with spinal cord injury. Arch Phys Med Rehabil. 2017;98:517–24.
Acknowledgements
We thank Benjamin Beirens, MSc, Angelene Fong, MSc MA, Stephanie Marino-Wäckerlin, MA, and Ursina Minder, BSc for their contributions to the data collection and Benjamin Beirens, MSc and Dr. Jonviea D. Chamberlain for proofreading the paper.
Funding
This project is supported by the Administration on Community Living, National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) (grant no. 90SI5014). NIDILRR is a Center within the Administration for Community Living (ACL) within the Department of Health and Human Services (HHS). The contents of this paper do not necessarily represent the policy of NIDILRR, ACL, or HHS, and you should not assume endorsement by the U.S. Government. This project has been supported by the Sports Medicine Nottwil from the Swiss Paraplegic Group by providing their ultrasound device. This project has also been supported by the International Society of Biomechanics with the International Travel Grant (1 July 2016). This study has been financed in the framework of the Swiss Spinal Cord Injury Cohort Study (SwiSCI, www.swisci.ch), supported by the Swiss Paraplegic Foundation. The members of the SwiSCI Steering Committee are: Xavier Jordan, Fabienne Reynard (Clinique Romande de Réadaptation, Sion); Michael Baumberger, Hans Peter Gmünder (Swiss Paraplegic Center, Nottwil); Armin Curt, Martin Schubert (University Clinic Balgrist, Zürich); Margret Hund-Georgiadis, Kerstin Hug (REHAB Basel, Basel); Hardy Landolt (Representative of persons with SCI, Glarus); Daniel Joggi (Swiss Paraplegic Foundation, Nottwil); Nadja Münzel (Parahelp, Nottwil); Mirjam Brach, Gerold Stucki (Swiss Paraplegic Research, Nottwil); Christine Fekete (SwiSCI Coordination Group at Swiss Paraplegic Research, Nottwil).
Author information
Authors and Affiliations
Consortia
Contributions
FMB, MLB, and UA initiated the study. FMB, MLB, UA, and AC contributed to the conception and design of the study. FMB performed the data collection and was responsible for all analyses, drafting, and finalization of the paper. All authors critically revised the paper. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was granted by the Ethikkommision Nordwest-und Zentralschweiz (EKNZ, Project-ID: 2017-00355). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bossuyt, F.M., Boninger, M.L., Cools, A. et al. Changes in supraspinatus and biceps tendon thickness: influence of fatiguing propulsion in wheelchair users with spinal cord injury. Spinal Cord 58, 324–333 (2020). https://doi.org/10.1038/s41393-019-0376-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-019-0376-z
This article is cited by
-
Finite Element Model of the Shoulder with Active Rotator Cuff Muscles: Application to Wheelchair Propulsion
Annals of Biomedical Engineering (2024)
-
Changes in shoulder outcomes using ultrasonographic assessment of breast cancer survivors: a prospective longitudinal study with 6-month follow-up
Scientific Reports (2021)