Abstract
Study design
Retrospective analysis of treated inpatients compared to expected neurorecovery from a propensity score-matched national database cohort.
Objective
Evaluate the effectiveness of buspirone on clinical neurorecovery following traumatic SCI when started during acute inpatient rehabilitation.
Setting
University-based hospital in Boston, USA.
Methods
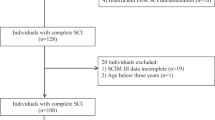
Chart review yielded thirty-one individuals with acute, traumatic SCI treated with buspirone during inpatient rehabilitation from 2011–2017. Propensity score matching to a cohort of individuals from the spinal cord injury model systems (SCIMS) national database was completed. Changes in upper extremity motor score (UEMS), lower extremity motor score (LEMS), American Spinal Injury Association Impairment Scale (AIS), neurological level of injury (NLI), and functional impairment measure (FIM) from admission to discharge and discharge to 1 year were computed and compared between matched pairs (buspirone and mean national SCIMs cohort). A local control cohort not treated with buspirone was similarly compared to a matched mean national SCIMs group to identify location-specific effects.
Results
From admission to discharge from inpatient rehabilitation, 95% confidence intervals of changes in UEMS (−2.43 to +2.78), LEMS (−1.02 to +6.02), AIS (−0.04 to +0.35), NLI (−0.42 to +1.08), and FIM (−4.42 to +6.40) were not significantly different between those individuals who received buspirone and their propensity-matched SCIMS cohort. Similarly, changes in these metrics were not significantly different at 1-year follow up. Buspirone group individuals with initial clinically complete SCI demonstrated a higher 1-year conversion rate to incomplete injury (6 out of 14; 42.9%) compared to the matched national SCIMS cohort (14 out of 70; 21.2%, p = 0.047) though this was not significantly different from non-buspirone local controls (p = 0.25).
Conclusions
Retrospective analysis shows no statistically significant difference in gross markers of neurorecovery following acute traumatic SCI when buspirone is initiated indiscriminately during acute inpatient rehabilitation. In individuals with clinically complete SCI, findings suggest possible increased rates of 1-year conversion to incomplete injury.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated during and/or analyzed during the current study are available in the National Spinal Cord Injury Model Systems (SCIMS) Database and can be requested per their internal policy upon approval [https://www.nscisc.uab.edu/Research/PublicDataRegister].
References
Jordan LM, Liu J, Hedlund PB, Akay T, Pearson KG. Descending command systems for the initiation of locomotion in mammals. Brain Res Rev. 2008;57:183–91.
Jacobs BL. Martı́n-Cora FJ, Fornal CA. Activity of medullary serotonergic neurons in freely moving animals. Brain Res Rev. 2002;40:45–52.
Carlsson A, Magnusson T, Rosengren E. 5-Hydroxytryptamine of the spinal cord normally and after transection. Experientia. 1963;19:359–359.
Cazalets JR, Sqalli‐Houssaini Y, Clarac F. Activation of the central pattern generators for locomotion by serotonin and excitatory amino acids in neonatal rat. J Physiol. 1992;455:187–204.
Madriaga MA, McPhee LC, Chersa T, Christie KJ, Whelan PJ. Modulation of locomotor activity by multiple 5-HT and dopaminergic receptor subtypes in the neonatal mouse spinal cord. J Neurophysiol. 2004;92:1566–76.
Hayashi Y, Jacob-Vadakot S, Dugan EA, McBride S, Olexa R, Simansky K, et al. 5-HT precursor loading, but not 5-HT receptor agonists, increases motor function after spinal cord contusion in adult rats. Exp Neurol. 2010;221:68–78.
Jeffrey-Gauthier R, Josset N, Bretzner F, Leblond H. Facilitation of locomotor spinal networks activity by buspirone after a complete spinal cord lesion in mice. J Neurotrauma. 2018;35:2208–21.
Gerasimenko YP, Lu DC, Modaber M, Zdunowski S, Gad P, Sayenko DG, et al. Noninvasive reactivation of motor descending control after paralysis. J Neurotrauma. 2015;32:1968–80.
Moshonkina TR, Shapkova EY, Sukhotina IA, Emeljannikov DV, Gerasimenko YP. Effect of combination of non-invasive spinal cord electrical stimulation and serotonin receptor activation in patients with chronic spinal cord lesion. Bull Exp Biol Med. 2016;161:749.
Guertin PA, Brochu C. Preliminary evidence of safety following administration of L-DOPA and buspirone in an incomplete monoplegic patient. Spinal Cord. 2009;47:91–2.
Freyvert Y, Yong NA, Morikawa E, Zdunowski S, Sarino ME, Gerasimenko Y, et al. Engaging cervical spinal circuitry with non-invasive spinal stimulation and buspirone to restore hand function in chronic motor complete patients. Sci Rep. 2018;8:1–10.
Chen Y, DeVivo MJ, Richards JS, SanAgustin TB. Spinal cord injury model systems: review of program and national database from 1970 to 2015. Arch Phys Med Rehabil. 2016;97:1797–804.
Chen Y. National spinal cord injury model systems database. Version 2016ARPublic. Birmingham, AL: National Spinal Cord Injury Statistical Center [distributor]. 2016. https://doi.org/10.17605/OSF.IO/NP24C.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
Sekhon JS. Multivariate and propensity score matching software with automated balance optimization: the matching package for R. J Stat Softw. 2011;42:1–52.
Fyffe DC, Deutsch A, Botticello AL, Kirshblum S, Ottenbacher KJ. Racial and ethnic disparities in functioning at discharge and follow-up among patients with motor complete spinal cord injury. Arch Phys Med Rehab. 2014;95:2140–51.
Horn SD, Smout RJ, DeJong G, Dijkers MP, Hsieh CH, Lammertse D, et al. Association of various comorbidity measures with spinal cord injury rehabilitation outcomes. Arch Phys Med Rehab. 2013;94:S75–86.
Eide PK, Hole K. The role of 5‐hydroxytryptamine (5‐HT) receptor subtypes and plasticity in the 5‐HT systems in the regulation of nociceptive sensitivity. Cephalalgia. 1993;13:75–85.
Kayser V, Bourgoin S, Viguier F, Michot B, Hamon M. Toward deciphering the respective roles of multiple 5-HT receptors in the complex serotonin-mediated control of pain. Pharmacol Pain. 2010:185–207.
Murray KC, Nakae A, Stephens MJ, Rank M, D'amico J, Harvey PJ, et al. Recovery of motoneuron and locomotor function after spinal cord injury depends on constitutive activity in 5-HT 2C receptors. Nat Med. 2010;16:694.
Fouad K, Rank MM, Vavrek R, Murray KC, Sanelli L, Bennett DJ. Locomotion after spinal cord injury depends on constitutive activity in serotonin receptors. J Neurophysiol. 2010;104:2975–84.
Kong XY, Wienecke J, Hultborn H, Zhang M. Robust upregulation of serotonin 2A receptors after chronic spinal transection of rats: an immunohistochemical study. Brain Res. 2010;1320:60–8.
Gorassini MA, Knash ME, Harvey PJ, Bennett DJ, Yang JF. Role of motoneurons in the generation of muscle spasms after spinal cord injury. Brain. 2004;127:2247–58.
Loane C, Politis M. Buspirone: what is it all about? Brain Res. 2012;1461:111–8.
Sramek JJ, Hong WW, Hamid S, Nape B, Cutler NR. Meta‐analysis of the safety and tolerability of two dose regimens of buspirone in patients with persistent anxiety. Depression Anxiety. 1999;9:131–4.
Perrin FE, Gerber YN, Teigell M, Lonjon N, Boniface G, Bauchet L, et al. Anatomical study of serotonergic innervation and 5-HT 1A receptor in the human spinal cord. Cell Death Dis. 2011;2:e218–e218.
Dunbar MJ, Tran MA, Whelan PJ. Endogenous extracellular serotonin modulates the spinal locomotor network of the neonatal mouse. J Physiol. 2010;588:139–56.
Lee JY, Kang SR, Yune TY. Fluoxetine prevents oligodendrocyte cell death by inhibiting microglia activation after spinal cord injury. J Neurotrauma. 2015;32:633–44.
Scali M, Begenisic T, Mainardi M, Milanese M, Bonifacino T, Bonanno G, et al. Fluoxetine treatment promotes functional recovery in a rat model of cervical spinal cord injury. Sci Rep. 2013;3:2217.
Leech KA, Kinnaird CR, Hornby TG. Effects of serotonergic medications on locomotor performance in humans with incomplete spinal cord injury. J Neurotrauma. 2014;31:1334–42.
Acknowledgements
The authors would like to specifically acknowledge the collective work of the National Spinal Cord Injury Statistical Center and Model Systems contributors, without whom this study would not have been possible.
Author information
Authors and Affiliations
Contributions
JWM was responsible for conducting literature review, designing the study protocol, extracting and analyzing data, interpreting results, and writing the report. RS was responsible for designing the study protocol, extracting and analyzing data, creating tables and figures, interpreting results, and writing the report.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
This study has been reviewed and approved by the Partners Human Research Committee (Protocol #: 2018P000667/PHS). In addition, The IRB has reviewed and approved to use research data obtained from Protocol 2011P002173 and HIPAA de-identified data obtained from the National Spinal cord Injury Statistical Center controlled access research database. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Morgan, J.W., Solinsky, R. Buspirone for functional improvement after acute traumatic spinal cord injury: a propensity score-matched cohort study. Spinal Cord 59, 563–570 (2021). https://doi.org/10.1038/s41393-020-00606-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-020-00606-0