Abstract
Study design
Randomised double-blind placebo-controlled trial.
Objectives
Multi-resistant organism (MRO) colonisation is common in people with SCI. We aimed to determine whether Lactobacillus reuteri RC-14 + Lactobacillus GR-1 (RC14-GR1) and/or Lactobacillus rhamnosus GG + Bifidobacterium BB-12 (LGG-BB12) are effective in preventing or clearing MRO colonisation.
Setting
New South Wales, Australia.
Methods
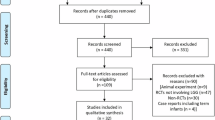
The 207 SCI participants were randomised to one of four arms: (i) RC14-GR1 + LGG-BB12, (ii) RC14-GR1 + placebo, (iii) LGG-BB12 + placebo or (iv) double placebos for 6 months. Microbiological samples of nose, groin, urine and bowel were taken at baseline, 3 and 6 months. Analysis was conducted for the presence of methicillin-resistant Staphylococcus aureus (MRSA), multi-resistant gram-negative organisms (MRGNs) and vancomycin-resistant enterococcus (VRE). The outcomes were clearance of, or new colonisation with MRSA, MRGN, VRE or MROs and whether participants remained free of MRSA, MRGN, VRE or MROs throughout the study. Risk factors associated with an outcome were adjusted for using nominal or binary logistic regression.
Results
There was a significant reduction in new MRGN colonisation compared with placebo for participants treated with RC14-GR1 (OR 0.10, 95% CI, 0.01–0.88, P = 0.04), after allowing that inpatients were more likely to be newly colonised (OR 21.41, 95% CI, 3.98–115.13, P < 0.0001). Participants who intermittent self-catheterised (IMC) were more likely to remain MRO-free than those utilising SPC or IDCs (OR 2.80, 95% CI, 1.41–5.54, P = 0.009).
Conclusions
Probiotics are ineffective at clearing MROs in people with SCI. However, RC14-GR1 is effective at preventing new colonisation with MRGNs. The use of IMC significantly improves the chance of remaining MRO-free.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
Raw data and datasets generated or extracted are archived in NEURA for 15 years. More detailed extracted data can be found in Supplementary Table 3–5.
References
Shallcross LJ, Davies SC. The World Health Assembly resolution on antimicrobial resistance. J Antimicrob Chemother. 2014;69:2883–5.
Casadevall A, Pirofski L-A. Host–pathogen interactions: basic concepts of microbial commensalism, colonization, infection, and disease. Infect Immun. 2000;68:6511–8.
Schwarz S, Silley P, Simjee S, Woodford N, van Duijkeren E, Johnson AP, et al. Assessing the antimicrobial susceptibility of bacteria obtained from animals. J Antimicrob Chemother. 2010;65:601–4.
NSW Department of Health. PD2007 084: Infection control policy: prevention and management of multi-resistant organisms. NSW Department of Health: New South Wales, Australia; 2007.
Girard R, Mazoyer M, Plauchu M, Rode G. High prevalence of nosocomial infections in rehabilitation units accounted for by urinary tract infections in patients with spinal cord injury. J Hospital Infect. 2006;62:473–9.
Lepainteur M, Ogna A, Clair B, Dinh A, Tarragon C, Prigent H, et al. Risk factors for respiratory tract bacterial colonization in adults with neuromuscular or neurological disorders and chronic tracheostomy. Respir Med. 2019;152:32–6.
Mylotte JM, Kahler L, Graham R, Young L, Goodnough S. Prospective surveillance for antibiotic-resistant organisms in patients with spinal cord injury admitted to an acute rehabilitation unit. Am J Infect Control. 2000;28:291–7.
Waites KB, Y-yC, DeVivo MJ, Canupp KC, Moser SA. Antimicrobial resistance in gram-negative bacteria isolated from the urinary tract in community-residing persons with spinal cord injury. Arch Phys Med Rehabil. 2000;81:764–9.
Suda K, Patel U, Sabzwari R, Cao L, Ramanathan S, Hill J, et al. Bacterial susceptibility patterns in patients with spinal cord injury and disorder (SCI/D): an opportunity for customized stewardship tools. Spinal Cord. 2016;54:1001.
Gallard J, Greig S. Management of Multi-resistant Organisms (MROs). New South Wales: South Eastern Sydney Illawarra Area Health Service Infection Control Manual Working Party; 2010.
Paterson DL, Bonomo RA. Extended-spectrum β-lactamases: a clinical update. Clin Microbiol Rev. 2005;18:657–86.
Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, et al. The International Scientific Association for probiotics and prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11:506–14.
Ouwehand AC, Forssten S, Hibberd AA, Lyra A, Stahl B. Probiotic approach to prevent antibiotic resistance. Ann Med. 2016;48:246–55.
Manley KJFM, Maynall BC, Power DA. treatment of vancomycin-resistant enterococci: a randomised controlled trial. Med J Aust. 2007;186:454–7.
Szachta P, Ignys I, Cichy W. An evaluation of the ability of the probiotic strain Lactobacillus rhamnosus GG to eliminate the gastrointestinal carrier state of vancomycin-resistant enterococci in colonized children. J Clin Gastroenterol. 2011;45:872–7.
Plummer SF, Garaiova I, Sarvotham T, Cottrell SL, Le Scouiller S, Weaver MA, et al. Effects of probiotics on the composition of the intestinal microbiota following antibiotic therapy. Int J Antimicrob Agents. 2005;26:69–74.
Sheu B-S, Cheng H-C, Kao A-W, Wang S-T, Yang Y-J, Yang H-B, et al. Pretreatment with Lactobacillus-and Bifidobacterium-containing yogurt can improve the efficacy of quadruple therapy in eradicating residual Helicobacter pylori infection after failed triple therapy. Am J Clin Nutr. 2006;83:864–9.
Sýkora J, Valecková K, Amlerová J, Siala K, Dedek P, Watkins S, et al. Effects of a specially designed fermented milk product containing probiotic Lactobacillus casei DN-114 001 and the eradication of H. pylori in children: a prospective randomized double-blind study. J Clin Gastroenterol. 2005;39:692–8.
Forestier C, Guelon D, Cluytens V, Gillart T, Sirot J, De Champs C. Oral probiotic and prevention of Pseudomonas aeruginosa infections: a randomized, double-blind, placebo-controlled pilot study in intensive care unit patients. Crit Care. 2008;12:R69.
Lee BB, Toh S-L, Ryan S-L,Simpson JM, Clezy K, Bossa L. et al. Probiotics [LGG-BB12 or RC14-GR1] versus placebo as prophylaxis for urinary tract infection in persons with spinalcord injury [ProSCIUTTU]: a study protocol for a randomised controlled trial. BMC Urol. 2016;16:18
Toh S-L, Lee BB, Ryan S, Simpson JM, Clezy K, Bossa L, et al. Probiotics [LGG-BB12 or RC14-GR1] versus placebo as prophylaxis for urinary tract infection in persons with spinal cord injury [ProSCIUTTU]: a randomised controlled trial. Spinal Cord. 2019;57:550–61.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
Kang MS, Lee BS, Lee HJ, Hwang SW, Han ZA. Prevalence of and risk factors for multidrug-resistant bacteria in urine cultures of spinal cord injury patients. Ann Rehabil Med. 2015;39:686–95.
Almomani BA, Hayajneh WA, Ayoub AM, Ababneh MA, Al Momani MA. Clinical patterns, epidemiology and risk factors of community-acquired urinary tract infection caused by extended-spectrum beta-lactamase producers: a prospective hospital case-control study. Infection. 2018;46:495–501.
García-Tello A, Gimbernat H, Redondo C, Meilán E, Arana DM, Cacho J, et al. Prediction of infection caused by extended-spectrum beta-lactamase-producing Enterobacteriaceae: development of a clinical decision-making nomogram. Scand J Urol. 2018;52:70–5.
Malcolm W, Fletcher E, Kavanagh K, Deshpande A, Wiuff C, Marwick C, et al. Risk factors for resistance and MDR in community urine isolates: population-level analysis using the NHS Scotland Infection Intelligence Platform. J Antimicrob Chemother. 2017;73:223–30.
Giske CG, Monnet DL, Cars O, Carmeli Y. Clinical and economic impact of common multidrug-resistant gram-negative bacilli. Antimicrob Agents Chemother. 2008;52:813–21.
Tabak YP, Sung AH, Ye G, Vankeepuram L, Gupta V, McCann E. Attributable clinical and economic burden of carbapenem-non-susceptible Gram-negative infections in patients hospitalized with complicated urinary tract infections. J Hospital Infect. 2019;102:37–44.
Vallejo-Torres L, Pujol M, Shaw E, Wiegand I, Vigo JM, Stoddart M, et al. Cost of hospitalised patients due to complicated urinary tract infections: a retrospective observational study in countries with high prevalence of multidrug-resistant Gram-negative bacteria: the COMBACTE-MAGNET, RESCUING study. BMJ Open. 2018;8:e020251.
Engler-Hüsch S, Heister T, Mutters NT, Wolff J, Kaier K. In-hospital costs of community-acquired colonization with multidrug-resistant organisms at a German teaching hospital. BMC Health Serv Res. 2018;18:737.
Salomão MCC, Heluany-Filho MA, Menegueti MG, Kraker MEAD, Martinez R, Bellissimo-Rodrigues F. A randomized clinical trial on the effectiveness of a symbiotic product to decolonize patients harboring multidrug-resistant Gram-negative bacilli. Rev da Soc Brasileira de Med Tropical. 2016;49:559–66.
Tannock GW, Tiong S, Priest P, Munro K, Taylor C, Richardson A, et al. Testing probiotic strain Escherichia coli Nissle 1917 (Mutaflor) for its ability to reduce carriage of multidrug-resistant E. coli by elderly residents in long-term care facilities. J Med Microbiol. 2011;60:366–70.
Dall LB, Lausch KR, Gedebjerg A, Fuursted K, Storgaard M, Larsen CS. Do probiotics prevent colonization with multi-resistant Enterobacteriaceae during travel? A randomized controlled trial. Travel Med Infect Dis. 2019;27:81–6.
de Regt MJ, Willems RJ, Hené RJ, Siersema PD, Verhaar HJ, Hopmans TE, et al. Effects of probiotics on acquisition and spread of multiresistant enterococci. Antimicrob Agents Chemother. 2010;54:2801–5.
Kappel C, Widmer A, Geng V, Von Arx P, Frei R, Koch H, et al. Successful control of methicillin-resistant Staphylococcus aureus in a spinal cord injury center: a 10-year prospective study including molecular typing. Spinal Cord. 2008;46:438.
Donskey CJ, Deshpande A. Effect of chlorhexidine bathing in preventing infections and reducing skin burden and environmental contamination: a review of the literature. Am J Infect Control. 2016;44:e17–e21.
Cassir N, Thomas G, Hraiech S, Brunet J, Fournier P-E, La Scola B, et al. Chlorhexidine daily bathing: Impact on health care–associated infections caused by gram-negative bacteria. Am J Infect Control. 2015;43:640–3.
Acknowledgements
The authors would like to thank other members of the ProSCIUTTU team—Dr Kate Clezy (KC), Dr Laetitia Bossa (LB), Dr Gerard Weber (GW), Dr Jasbeer Kaur (JK), Dr Claire Boswell-Ruys (CBR), Dr Stephen Goodall (SG), Dr James Middleton (JM), Mr Mark Tudehope (MT), Dr Marcella Kwan and Ms Elizabeth Rose.
Funding
National Health and Medical Research Council (NHMRC) is the organisation responsible for funding the supply of probiotics and matching placebo selected by the researchers for this study and budgeted within the NHMRC grant. CHR Hansen, Horsholm, Denmark has been paid commercial rates for providing the intervention product and placebo. The company had no input into the design of the trial.
Author information
Authors and Affiliations
Contributions
Trial protocol was developed by S-LT, BBL, JMS, OM, GK, SR, KC, GW, JK, CBR, SG, JM and MT over a series of teleconferences and workshops in Sydney, Australia in the late 2009 and early 2010 from an original study design developed by BBL and JMS. OM was responsible for designing and maintaining trial database. Data analysis was conducted by S-LT and checked by JMS. S-LT was responsible for initial manuscript preparation. All authors reviewed and were involved in writing up the final version of the manuscript prior to submission.
Corresponding author
Ethics declarations
Conflict of interest
BBL, JMS, SG and JM have received competitive research funding support from the NHMRC. BBL, CBR, JMS, KC and S-LT are also authors on the Cochrane review—probiotics for preventing UTI in people with neuropathic bladder. The Coloplast company has provided nursing support to several of BBL’s community patients with recurrent UTIs from January 2018 to July 2019 and continues to provide occasional community support to some of these patients. However, Coloplast has had no financial or editorial input into the design, analysis or write up of this trial. The rest of the authors have no competing financial or non-financial interests.
Ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were following during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Toh, SL., Lee, B.B., Simpson, J.M. et al. Effect of probiotics on multi-resistant organism colonisation in persons with spinal cord injury: secondary outcome of ProSCIUTTU, a randomised placebo-controlled trial. Spinal Cord 58, 755–767 (2020). https://doi.org/10.1038/s41393-020-0420-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-020-0420-z
This article is cited by
-
Gut Microbes and Inflammation: Their Role in Spinal Cord Injury Progression and Secondary Damage
Current Microbiology (2025)
-
A comprehensive look at the psychoneuroimmunoendocrinology of spinal cord injury and its progression: mechanisms and clinical opportunities
Military Medical Research (2023)
-
Mapping of Dietary Interventions Beneficial in the Prevention of Secondary Health Conditions in Spinal Cord Injured Population: A Systematic Review
The Journal of nutrition, health and aging (2023)