Abstract
Study design
Cross-sectional validation study.
Objectives
To conduct a literature search for existing energy expenditure (EE) predictive algorithms using ActiGraph activity monitors for manual wheelchairs users (MWUs) with spinal cord injury (SCI), and evaluate their validity using an out-of-sample dataset.
Setting
Research institution in Pittsburgh, USA.
Methods
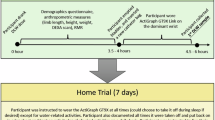
A literature search resulted in five articles containing five sets of predictive equations using an ActiGraph activity monitor for MWUs with SCI. Out-of-sample data were collected from 29 MWUs with chronic SCI who were asked to follow an activity protocol while wearing an ActiGraph GT9X Link on the dominant wrist. They also wore a portable metabolic cart which provided the criterion measure for EE. The out-of-sample dataset was used to evaluate the validity of the five sets of EE predictive equations.
Results
None of the five sets of predictive equations demonstrated equivalence within 20% of the criterion measure based on an equivalence test. The mean absolute error for the five sets of predictive equations ranged from 0.87 to 6.41 kilocalories per minute (kcal min−1) when compared with the criterion measure, and the intraclass correlation estimates ranged from 0.06 to 0.59. The range between the Bland–Altman upper and lower limits of agreement was from 4.70 kcal min−1 to 25.09 kcal min−1.
Conclusions
The existing EE predictive equations based on ActiGraph monitors for MWUs with SCI showed varied performance when compared with the criterion measure. Their accuracies may not be sufficient to support future clinical and research use. More work is needed to develop more accurate EE predictive equations for this population.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets supporting this study are available on reasonable request from the corresponding author.
Change history
17 August 2020
An amendment to this article has been published and can be accessed via a link at the top of the article.
18 August 2020
A Correction to this paper has been published: https://doi.org/10.1038/s41393-020-00534-z
References
WHO | Spinal Cord Injury. WHO, Fact sheet N°384 (2013). https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury.
Shields RK, Dudley-Javoroski S. Monitoring standing wheelchair use after spinal cord injury: a case report. Disabil Rehabil. 2005;27:142–6.
Buchholz AC, McGillivray CF, Pencharz PB. Physical activity levels are low in free-living adults with chronic paraplegia. Obes Res. 2003;11:563–70.
Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ 2006;174:801–9.
Chiauzzi E, Rodarte C, DasMahapatra P. Patient-centered activity monitoring in the self-management of chronic health conditions. BMC Med. 2015;13:77.
Hiremath SV, Amiri AM, Thapa-Chhetry B, Snethen G, Schmidt-Read M, Ramos-Lamboy M, et al. Mobile health-based physical activity intervention for individuals with spinal cord injury in the community: a pilot study. PloS ONE. 2019;14:e0223762.
Scott J, Grierson A, Gehue L, Kallestad H, MacMillan I, Hickie I. Can consumer grade activity devices replace research grade actiwatches in youth mental health settings? Sleep and Biological Rhythms. 2019;17:223–32.
Poehlman ET. A review: exercise and its influence on resting energy metabolism in man. Med Sci Sports Exerc. 1989;21:515–25.
Buchholz AC, Pencharz PB. Energy expenditure in chronic spinal cord injury. Curr Opin Clin Nutr Metab Care. 2004;7:635–9.
Nightingale TE, Rouse PC, Thompson D, Bilzon JLJ. Measurement of physical activity and energy expenditure in wheelchair users: methods, considerations and future directions. Sports Med Open. 2017;3:10.
Tsang K. Using wearable sensors for physical activity measurement and promotion in manual wheelchair users [Dissertation]. Pittsburgh (PA): University of Pittsburgh; 2018.
Nightingale TE, Walhim JP, Thompson D, Bilzon JL. Predicting physical activity energy expenditure in manual wheelchair users. Med Sci Sports Exerc. 2014;46:1849–58.
Nightingale TE, Walhin JP, Thompson D, Bilzon JL. Influence of accelerometer type and placement on physical activity energy expenditure prediction in manual wheelchair users. PLoS ONE. 2015;10:e0126086.
Garcia-Masso X, Serra-Ano P, Garcia-Raffi LM, Sanchez-Perez EA, Lopez-Pascual J, Gonzalez LM. Validation of the use of actigraph GT3X accelerometers to estimate energy expenditure in full time manual wheelchair users with spinal cord injury. Spinal Cord. 2013;51:898–903.
Learmonth YC, Kinnett-Hopkins D, Rice IM, Dysterheft JL, Motl RW. Accelerometer output and its association with energy expenditure during manual wheelchair propulsion. Spinal Cord. 2016;54:110–4.
Weir JBDB. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949;109:1–9.
McClave SA, Spain DA, Skolnick JL, Lowen CC, Kieber MJ, Wickerham PS, et al. Achievement of steady state optimizes results when performing indirect calorimetry. JPEN J Parenter Enter Nutr. 2003;27:16–20.
Schlein KM, Coulter SP. Best practices for determining resting energy expenditure in critically ill adults. Nutr Clin Pr. 2014;29:44–55.
Reeves MM, Davies PS, Bauer J, Battistutta D. Reducing the time period of steady state does not affect the accuracy of energy expenditure measurements by indirect calorimetry. J Appl Physiol. 2004;97:130–4.
Compher C, Frankenfield D, Keim N, Roth-Yousey L. Best practice methods to apply to measurement of resting metabolic rate in adults: a systematic review. J Acad Nutr Diet. 2006;106:881–903.
Dixon PM, Saint-Maurice PF, Kim Y, Hibbing P, Bai Y, Welk GJ. A primer on the use of equivalence testing for evaluating measurement agreement. Med Sci Sports Exerc. 2018;50:837–45.
Robinson AP, Duursma RA, Marshall JD. A regression-based equivalence test for model validation: shifting the burden of proof. Tree Physiol. 2005;25:903–13.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–63.
Giavarina D. Understanding Bland Altman analysis. Biochem Med. 2015;25:141–51.
Collins EG, Gater D, Kiratli J, Butler J, Hanson K, Langbein WE. Energy cost of physical activities in persons with spinal cord injury. Med Sci Sports Exerc. 2010;42:691–700.
Nightingale TE, Gorgey AS. Predicting basal metabolic rate in men with motor complete spinal cord injury. Med Sci Sports Exerc. 2018;50:1305–12.
Xie J, Wen D, Liang L, Jia Y, Gao L, Lei J. Evaluating the validity of current mainstream wearable devices in fitness tracking under various physical activities: comparative study. JMIR mHealth uHealth. 2018;6:e94.
Chowdhury EA, Western MJ, Nightingale TE, Peacock OJ, Thompson D. Assessment of laboratory and daily energy expenditure estimates from consumer multi-sensor physical activity monitors. PloS ONE. 2017;12:e0171720.
O’Driscoll R, Turicchi J, Beaulieu K, Scott S, Matu J, Deighton K, Finlayson G, Stubbs J. How well do activity monitors estimate energy expenditure? A systematic review and meta-analysis of the validity of current technologies. Br J Sports Med. 2018. https://doi.org/10.1136/bjsports-2018-099643.
Maijers MC, Verschuren O, Stolwijk-Swüste JM, van Koppenhagen CF, de Groot S, Post MWM. Is Fitbit Charge 2 a feasible instrument to monitor daily physical activity and handbike training in persons with spinal cord injury? A pilot study. Spinal Cord Ser Cases. 2018;4:84.
Nightingale TE, Walhin JP, Thompson D, Bilzon JLJ. Predicting physical activity energy expenditure in wheelchair users with a multisensor device. BMJ Open Sport Exerc Med. 2015;1:bmjsem-2015-000008.
Acknowledgements
We would like to acknowledge and thank Steven Knezevic, Dr Eunkyoung Hong, and Dr Ann Spungen at the James J. Peters VA Medical Center for their assistance in collecting a portion of the out-of-sample datasets.
Funding
This study was funded by the VA Rehabilitation Research & Development under Grant #1I01RX000971-01A. The content is solely the responsibility of the authors and does not represent the official views of the VA.
Author information
Authors and Affiliations
Contributions
YJS was responsible for conducting data analysis, obtaining results, and writing the paper in its entirety. ALV was responsible for designing the protocol, screening potential participants, and performing data collection. She also contributed to data analysis and interpretation of results. ZH was responsible for developing the search criteria used to obtain publications of existing energy expenditure equations as mentioned in the methods. He also contributed to data analysis and interpretation of results. DD provided guidance throughout the study including formulating the paper plan, supervising the literature search, data collection, data analysis, and result interpretation, as well as editing the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the US Department of Veterans Affairs (VA) Central Institutional Review Board and the local Institutional Review Boards at the VA Pittsburgh Healthcare System and the James J. Peters VA Medical Center, respectively. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Shwetar, Y.J., Veerubhotla, A.L., Huang, Z. et al. Comparative validity of energy expenditure prediction algorithms using wearable devices for people with spinal cord injury. Spinal Cord 58, 821–830 (2020). https://doi.org/10.1038/s41393-020-0427-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-020-0427-5