Abstract
Study design
A retrospective chart review.
Objectives
Total en bloc spondylectomy (TES) has been reported to decrease the rate of local recurrence and increase survival. Although it is important to achieve early recovery of physical functions after surgery, no studies have evaluated rehabilitation outcomes during the acute phase after TES. This study evaluated ambulatory functions and activities of daily living (ADLs) after surgery and analyzed the prognostic significance of variables affecting rehabilitation outcomes at 1 month after TES.
Setting
University hospital in Kanazawa, Japan.
Methods
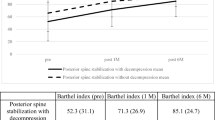
This study included 140 patients with spinal tumors who underwent TES between April 2010 and April 2017. Demographic characteristics, neurological functions, perioperative complications functional status as measured by the Functional Independent Measure, and independent indoor walking based on the Spinal Cord Independent Measure were extracted from medical records. Multivariate analyses were performed to assess factors associated with the recovery of ambulation and ADL at 1 month after TES.
Results
Preoperative neurological deficits were observed in 51 patients (36%), and postoperative neurological deterioration was found in 41 patients (29%). Multivariate analyses indicated that preoperative neurological deficits (odds ratio [OR], 5.23; 95% confidence interval [CI], 2.07–15.99), postoperative cerebrospinal fluid leakage (OR, 13.42; 95% CI, 2.93–78.82), surgical site infections (OR, 15.27; 95% CI, 2.26–127.7), and postoperative neurological deterioration (OR, 4.86; 95% CI, 1.33–19.99) were risk factors for walking ability and recovery of ADL (P < 0.01).
Conclusions
This study identified preoperative neurological dysfunction and perioperative complications as independent risk factors for poor recovery of ambulation and ADL early after TES.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Tomita K, Kawahara N, Baba H, Tsuchiya H, Nagata S, Toribatake Y. Total en bloc spondylectomy for solitary spinal metastases. Int Orthop. 1994;18:291–8.
Kawahara N, Tomita K, Murakami H, Demura S. Total en bloc spondylectomy for spinal tumors: surgical techniques and related basic background. Orthop Clin North Am. 2009;40:47–63.
Kato S, Murakami H, Demura S, Numbu Y, Yoshioka K, Kawahara N, et al. Spinal metastasectomy of renal cell carcinoma: a 16-year single center experience with a minimum 3-year follow-up. J Surg Oncol. 2016;113:587–92.
Kato S, Murakami H, Demura S, Fujimaki Y, Yoshioka K, Yokogawa N, et al. The impact of complete surgical resection of spinal metastases on the survival of patients with thyroid cancer. Cancer Med. 2016;5:2343–9.
Kato S, Murakami H, Demura S, Yoshioka K, Kawahara N, Tomita K, et al. More than 10-year follow-up after total en bloc spondylectomy for spinal tumors. Ann Surg Oncol. 2014;21:1330–6.
McKinley WO, Huang ME, Brunsvold KT. Neoplastic versus traumatic spinal cord injury: an outcome comparison after inpatient rehabilitation. Arch Phys Med Rehabil. 1999;80:1253–7.
Hayashi H, Murakami H, Demura S, Kato S, Yoshioka K, Shinmura K, et al. Surgical site infection after total en bloc spondylectomy: risk factors and the preventive new technology. Spine J. 2015;15:132–7.
Murakami H, Kawahara N, Demura S, Kato S, Yoshioka K, Tomita K. Neurological function after total en bloc spondylectomy for thoracic spinal tumors. J Neurosurg Spine. 2010;12:253–6.
Shimizu T, Murakami H, Demura S, Kato S, Yoshioka K, Yokogawa N, et al. Total en bloc spondylectomy for primary tumors of the lumbar spine. Medicine. 2018;97:e12366.
Loblaw DA, Laperriere NJ. Emergency treatment of malignant extradural spinal cord compression: an evidence-based guideline. J Clin Oncol. 1998;16:1613–24.
Tomita K, Kawahara N, Murakami H, Demura S. Total en bloc spondylectomy for spinal tumors: improvement of the technique and its associated basic background. J Orthop Sci. 2006;11:3–12.
Kato S, Murakami H, Demura S, Yoshioka K, Yokogawa N, Yonezawa N, et al. Kidney and thyroid cancer-specific treatment algorithm for spinal metastases: a validation study. World Neurosurg. 2019;122:e1305–e1311.
Maynard FM, Bracken MB, Creasey G, Ditunno JF, Donovan WH, Ducker TB, et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord 1997;35:266–74.
Yokogawa N, Murakami H, Demura S, Kato S, Yoshioka K, Hayashi H, et al. Postoperative cerebrospinal fluid leakage associated with total en bloc spondylectomy. Orthopedics. 2015;38:e561–e566.
Catz A, Itzkovich M, Steinberg F, Philo O, Ring H, Ronen J, et al. The Catz-Itzkovich SCIM: a revised version of the Spinal Cord Independence Measure. Disabil Rehabil. 2001;23:263–8.
van Middendorp JJ, Hosman AJF, Donders ART, Pouw MH, Ditunno JF, Curt A, et al. A clinical prediction rule for ambulation outcomes after traumatic spinal cord injury: a longitudinal cohort study. Lancet. 2011;377:1004–10.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT, et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord. 2007;45:275–91.
Granger CV, Hamilton BB, Keith RA, Zielezny M, Sherwin FS. Advances in functional assessment for medical rehabilitation. Top Geriatr Rehabil. 1986;1:59.
Scivoletto G, Lapenna LM, Di Donna V, Laurenza L, Sterzi S, Foti C, et al. Neoplastic myelopathies and traumatic spinal cord lesions: an Italian comparison of functional and neurological outcomes. Spinal Cord. 2011;49:799–805.
Quan GMY, Vital JM, Aurouer N, Obeid I, Palussière J, Diallo A, et al. Surgery improves pain, function and quality of life in patients with spinal metastases: a prospective study on 118 patients. Eur Spine J. 2011;20:1970–8.
Demura S, Kawahara N, Murakami H, Nambu K, Kato S, Yoshioka K, et al. Surgical site infection in spinal metastasis: risk factors and countermeasures. Spine. 2009;34:635–9.
Yokogawa N, Murakami H, Demura S, Kato S, Yoshioka K, Hayashi H, et al. Perioperative complications of total en bloc spondylectomy: adverse effects of preoperative irradiation. PLoS ONE. 2014;9:e98797.
Beninato M, Gill-Body KM, Salles S, Stark PC, Black-Schaffer RM, Stein J. Determination of the minimal clinically important difference in the FIM instrument in patients with stroke. Arch Phys Med Rehabil. 2006;87:32–39.
Boriani S, Bandiera S, Donthineni R, Amendola L, Cappuccio M, De Iure F, et al. Morbidity of en bloc resections in the spine. Eur Spine J. 2010;19:231–41.
Murakami H, Kawahara N, Demura S, Kato S, Yoshioka K, Sasagawa T, et al. Perioperative complications and prognosis for elderly patients with spinal metastases treated by surgical strategy. Orthopedics. 2010;10:165–8.
Amandola L, Cappuccio M, Federico DI, Bandiera S, Gasbarrini A, Boriani S. En bloc resections for primary spinal tumors in 20 years of experience: effectiveness and safety. Spine J. 2014;14:2608–17.
Ehresman J, Ahmad AK, Schilling A, Pennington Z, Lubelski D, Cottrill E, et al. Preoperative nutrition consults associated with decreased postoperative complication rate and decreased length of hospital stay after spine metastasis surgery. World Neurosurg. 2019;19. https://doi.org/10.1016/j.wneu.2019.08.197.
Buck JS, Yoon ST. The incidence of durotomy and its clinical and economic impact in primary, short-segment lumbar fusion: an analysis of 17,232 cases. Spine. 2015;40:1444–50.
Casadei R, Mavrogenis AF, De Paolis M, Ruggieri P. Two-stage, combined, three-level en bloc spondylectomy for a recurrent post-radiation sarcoma of the lumbar spine. Eur J Orthop Surg Traumatol. 2013;23(Suppl 1):S93–100.
Suetta C, Frandsen U, Jensen L, Jensen MM, Jespersen JG, Hvid LG, et al. Aging affects the transcriptional regulation of human skeletal muscle disuse atrophy. PLoS ONE. 2012;7:e51238.
Saotome T, Klein L, Faux S. Cancer rehabilitation: a barometer for survival? Support Care Cancer. 2015;23:3033–41.
Chaichana KL, Woodworth GF, Sciubba DM, McGirt MJ, Witham TJ, Bydon A, et al. Predictors of ambulatory function after decompressive surgery for metastatic epidural spinal cord compression. Neurosurgery. 2008;62:683–92. discussion 683-92.
Helweg-Larsen S, Sørensen PS, Kreiner S. Prognostic factors in metastatic spinal cord compression: a prospective study using multivariate analysis of variables influencing survival and gait function in 153 patients. Int J Radiat Oncol Biol Phys. 2000;46:1163–9.
Acknowledgements
We would like to thank Editage (www.editage.jp) for English language editing.
Author information
Authors and Affiliations
Contributions
YK was responsible for designing the review protocol, conducting the search, screening potentially eligible studies, extracting and analyzing data, interpreting results, creating tables, creating figures, and writing the report. HM and SD were responsible for designing the review protocol, screening potentially eligible studies, and extracting and analyzing data, and interpreting results. SK contributed to writing the report, extracting and analyzing data, interpreting results, and providing feedback regarding the report. NY, KS, TS, and HT contributed to data extraction and provided feedback regarding the report.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the ethics committee of our University Hospital.
Informed consent
Informed consent for inclusion in this study was obtained from the patients and/or their guardians.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kurokawa, Y., Murakami, H., Demura, S. et al. Risk factors for poor outcomes of early rehabilitation after total en bloc spondylectomy: a retrospective chart review of 140 patients. Spinal Cord 58, 900–907 (2020). https://doi.org/10.1038/s41393-020-0440-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-020-0440-8
This article is cited by
-
Comprehensive Management of Spine Metastasis in Cancer Patients: From Identification to Rehabilitation
Current Physical Medicine and Rehabilitation Reports (2024)