Abstract
Study design
Prospective, quasi-experimental study, pre- and post-design, single arm study.
Objectives
Investigate whether persons affected by SCI can safely experience walking function using Robotic Exoskeletons and Functional Electrical Stimulation (FES).
Setting
Inpatient
Methods
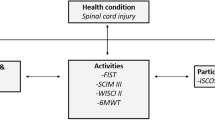
52 persons with SCI were recruited (36 completed the protocol) and assigned to one of two groups based on their Lower Limb Motor Scores (LEMS): Group A: LEMS ≥ 10 and Group B: LEMS < 10. Participants in Group A (n = 19) underwent 20 sessions of Robot-Assisted Gait Training (RAGT) on a treadmill followed by 20 sessions of FES during Overground Gait (FES-OG). Participants in Group B (n = 17) received 20 sessions of FES-cycling followed by 20 sessions of overground RAGT. The main outcome measures were: WISCI-II, 10MWT, 6MWT, TUG and SCIM-II.
Results
36 persons completed the study with no complications; only 4 of the 16 dropped out because of mild complications during the RAGT. Participants in Group A exhibited significant improvements in WISCI-II, 10MWT, 6MWT and TUG (p < 0.05), while those in Group B did not significantly improve their gait function but their walking velocity and resistance with the assistance of the robotic exoskeleton increased. SCIM-II scores increased followed therapy only in Group A.
Conclusions
Persons affected by SCI can safely experience their walking function with RAGT and FES therapy; only few mild complications were observed. Our data provides initial evidence of the potential value of these technologies, especially in persons with SCI having LEMS > 10.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Stevens S, Caputo J, Fuller D, Morgan DW. Physical activity and quality of life in adults with spinal cord injury. J Spinal Cord Med. 2008;31:373–8.
Simpson LA, Eng JJ, Hsieh JT, Wolfe DL, and the SCIRE Research Team. The health and life priorities of individuals with spinal cord injury: a systematic review. J Neurotrauma. 2012;29:1548–55.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2011;34:535–46.
Moon J, Yu J, Choi J, Kim MY, Min K. Degree of contributions of motor sensory scores to predict gait ability in patients with incomplete spinal cord injury. Rehabil Med. 2017;41:969–78.
Van Middendorp JJ, Hosman AJ, Pouw MH, EM-SCI Study Group, Van de Meent H. ASIA impairment scale conversion in traumatic SCI: is it related with the ability to walk? A descriptive comparison with functional ambulation outcome measures in 273 patients. Spinal Cord. 2009;47:555–60.
Visintin M, Barbeau H. The effect of body weight support on the locomotor pattern of spastic paretic patients. Can J Neurol Sci. 1989;16:315–25.
Colombo G, Joerg M, Schreier R, Dietz V. Treadmill training of paraplegic patients using a robotic orthosis. J Rehabil Res Dev. 2000;37:693–700.
Mazzoleni S, Boldrini E, Laschi C, Carrozza MC, Stampacchia G, Rossi B. Change on EMG activation in healthy subjects and incomplete SCI patients following a robot-assisted locomotor training, in Proc. International Conference on Rehabilitation Robotics 2011, Zurich, Switzerland, pp. 864–9.
Winchester P, McColl R, Querry R. Changes in supraspinal activation patterns following robotic locomotor therapy in motor-incomplete spinal cord injury. NeuroRehab Neural Repair. 2005;19:313–24.
Hubli M, Dietz V. The physiological basis of neurorehabilitation–locomotor training after spinal cord injury. J Neuroeng Rehabil. 2013;10:5. https://doi.org/10.1186/1743-0003-10-5.
Baunsgaard CB, Nissen UV, Brust AK, Frotzler A, Ribeill C, Kalke YB, et al. Gait training after spinal cord injury: safety, feasibility and gait function following 8 weeks of training with the exoskeletons from Ekso Bionics. Spinal Cord. 2018;56:106–16.
Stampacchia G, Rustici A, Bigazzi S, Gerini A, Tombini T, Mazzoleni S. Walking with a powered robotic exoskeleton: subjective experience, spasticity and pain in spinal cord injured persons. NeuroRehab. 2016;39:277–83.
Kressler J, Thomas CK, Field-Fote EC, Sanchez J, Widerström-Noga E, Cilien DC, et al. Understanding therapeutic benefits of overground bionic ambulation: exploratory case series in persons with chronic, complete spinal cord injury. Arch Phys Med Rehabil. 2015;21:122–32.
Kapandia N, Masani K, Craven BC, Giangregorio ML, Hitzig SL, Richards K, et al. A randomized trial of functional electrical stimulation for walking in incomplete spinal cord injury: effects on walking competency. J Spinal Cord Med. 2014;37:511–24.
Frotzler A, Coupaud S, Perrett C, Kakebeeke TH, Hunt KJ, Donaldson NN, et al. High-Volume FES-Cycling partially reverses bone loss in people with chronic spinal cord injury. Bone. 2008;43:169–76.
Yasar E, Yilmaz B, Goktepe S, Kesikburun S. The effect of functional electrical stimulation cycling on late functional improvement in patients with chronic incomplete spinal cord injury. Spinal Cord. 2015;53:866–9.
Dolbow DR, Gorgey AS, Ketchum JM, Gater DR. Home-based functional electrical stimulation cycling enhance quality of life in individuals with spinal cord injury. Top Spinal Cord Inj Rehabil. 2013;19:324–9.
Mazzoleni S, Stampacchia G, Gerini A, Tombini T, Carrozza MC. FES-cycling training in spinal cord injured patients. Conf Proc IEEE Eng Med Biol Soc. 2013;2013:5339–41.
Fisahn C, Aach M, Jansen O, Moisi M, Mayadev A, Pagarigan KT, et al. The effectiveness and safety of exoskeletons as assistive and rehabilitation devices in the treatment of neurologic gait disorders in patients with spinal cord injury: a systematic review. Glob Spine J. 2016;6:822–41.
Shackleton C, Evans R, Shamley D, West S, Albertus Y. Effectiveness of over-ground robotic locomotor training in improving walking performance, cardiovascular demands, secondary complications and user-satisfaction in individuals with spinal cord injuries: a systematic review. J Rehabil Med. 2019;51:723–33.
Morawietz C, Moffat F. Effects of locomotor training after incomplete spinal cord injury: a systematic review. Arch Phys Med Rehabil. 2013;94:2297–308.
Catz A, Itzkovich M, Steinberg F, Philo O, Ring H, Ronen J, et al. The Catz-Itzkovich SCIM: a revised version of the spinal cord independence measure. Disabil Rehabil. 2001;23:263–8.
Ditunno P, Ditunno J. Walking index for spinal cord injury (WISCI II): scale revision. Spinal Cord. 2001;39:654–6.
Van Hedel HJ, Wirz M, Dietz V. Assessing walking ability in subjects with spinal cord injury: validity and reliability of 3 walking tests. Arch Phys Med Rehabil. 2005;86:190–6.
Ferro S, Cecconi L, Bonavita J, Pagliacci MC, Biggeri A, Franceschini M. Incidence of traumatic spinal cord injury in Italy during 2013-2014: a popoulation-based study. Spinal Cord. 2017;55:1103–7.
Citterio A, Franceschini M, Spizzichino L, Reggio A, Rossi B, Stampacchia G, for the Gruppo Italiano Studio Epidemiologico Mielolesioni. Nontraumatic spinal cord injury: an Italian survey. Arch Phys Med Rehabil. 2004;85:1483–7.
Benson I, Hart K, Tussler D, Van Middendorp JJ. Lower-limb exoskeletons for individuals with chronic spinal cord injury: findings from a feasibility study. Clin Rehabil. 2016;30:73–84.
Louie DR, Eng JJ, Lam T, and Spinal Cord Injury Research Evidence (SCIRE) Research Team. Gait speed using powered robotic exoskeletons after spinal cord injury: a systematic review and correlational study. J NeuroEng Rehab. 2015;12:1–10.
Yang A, Asselin P, Knezevic S, Kornfeld S, Spungen AM. Assessment of in-hospital walking velocity and level of assistance in powered exoskeletons in persons with spinal cord injury. Top Spinal Cord Inj Rehabil. 2015;21:100–9.
Heinemann AW, Jayaraman A, Mummydisetty CK, Spraggins J, Pinto D, Charlifue S, et al. Experience of robotic exoskeleton use at four spinal cord injury model systems centers. JNPT. 2018;42:256–67.
Fornusek C, Davis GM, Russold MF. Pilot study of the effect of low-cadence functional electrical stimulation cycling after spinal cord injury on thigh girth and strength. Arch Phys Med Rehab. 2013;94:990–3.
Andrews B, Shippen J, Armegol M, Gibbons R, Holderbaum W, Harwin W. A design method for FES bone health therapy in SCI. Eur J Transl Myol. 2016;26:297–300.
Acknowledgements
The authors would like to thank Zach McKinney for his linguistic expertise in reviewing this paper.
Funding
Italian Health Ministry founded the project: “Clinical and healthcare strategies for improving quality of life in persons affected by SCI: Tuscany regional network and use of innovative technologies devices”. Code Project: RF-2011-02346770.
Author information
Authors and Affiliations
Contributions
GS was responsible of the study protocol, carried out patients’ selection, supervised clinical evaluations and treatments, supervised dataset production and analysed data, interpreted results, and drafted the paper. MO was responsible of dataset production, contributed to statistical analysis and contributed to drafted the paper. AR carried out patients’ physiotherapy evaluation and treatments, contributed to dataset production. CDA contributed to clinical evaluations. AG carried out clinical evaluations. SM contributed to design the study protocol, supervised statistical analysis, analysed the data, interpreted results and drafted the paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study followed the guidelines of the Declaration of Helsinki. All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. All the necessary approvals were obtained, including local ethic committee (protocol number 410699).
Informed consent
All participants received oral, as well as written information about the study, before informed consent was obtained.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stampacchia, G., Olivieri, M., Rustici, A. et al. Gait rehabilitation in persons with spinal cord injury using innovative technologies: an observational study. Spinal Cord 58, 988–997 (2020). https://doi.org/10.1038/s41393-020-0454-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-020-0454-2
This article is cited by
-
Human-machine Interface using functional electrostimulation and inertial sensors for lower limb rehabilitation in spinal cord injury individuals: a proof of concept
Medical & Biological Engineering & Computing (2026)
-
Biomaterials and cell-based therapy post spinal cord injury
Journal of Translational Medicine (2025)
-
Exoskeleton-based exercises for overground gait and balance rehabilitation in spinal cord injury: a systematic review of dose and dosage parameters
Journal of NeuroEngineering and Rehabilitation (2024)
-
Functional electrical stimulation cycling exercise after spinal cord injury: a systematic review of health and fitness-related outcomes
Journal of NeuroEngineering and Rehabilitation (2021)