Abstract
Study design
Retrospective, cohort study of a prospectively collected database.
Objectives
In a cohort of patients with traumatic spine injury (TSI) in Tanzania who did not undergo surgery, we sought to: (1) describe this nonoperative population, (2) compare outcomes to operative patients, and (3) determine predictors of nonoperative treatment.
Setting
Tertiary referral hospital.
Methods
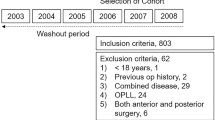
All patients admitted for TSI over a 33-month period were reviewed. Variables included demographics, fracture morphology, neurologic exam, indication for surgery, length of hospitalization, and mortality. Regression analyses were used to report outcomes and predictors of nonoperative treatment.
Results
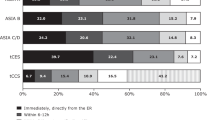
270 patients met inclusion criteria, of which 145 were managed nonoperatively. Demographics between groups were similar. The nonoperative group was young (mean = 35.5 years) and primarily male (n = 125, 86%). Nonoperative patients had 7.39 times the odds of death (p = 0.003). Patients with AO type A0/1/2/3 fractures (p < 0.001), ASIA E exams (p = 0.016), cervical spine injuries (p = 0.005), and central cord syndrome (p = 0.016) were more commonly managed nonoperatively. One hundred and twenty-four patients (86%) had indications for but did not undergo surgery. After multivariate analysis, the only predictor of nonoperative management was sustaining a cervical injury (p < 0.001).
Conclusions
Eighty-six percent of nonoperative TSI patients had an indication for surgery. Nonoperative management was associated with an increased risk of mortality. Cervical injury was the single independent risk factor for not undergoing surgery. The principle reason for nonoperative management was cost of implants. While a causal relationship between nonoperative management and inferior outcomes cannot be made, efforts should be made to provide surgery when indicated, regardless of a patient’s ability to pay.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
GBD Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:56–87.
Kumar R, Lim J, Mekary RA, Rattani A, Dewan MC, Sharif SY, et al. Traumatic spinal injury: global epidemiology and worldwide volume. World Neurosurg. 2018;113:e345–63.
La Rosa G, Conti A, Cardali S, Cacciola F, Tomasello F. Does early decompression improve neurological outcome of spinal cord injured patients? Appraisal of the literature using a meta-analytical approach. Spinal Cord. 2004;42:503–12.
Rashid SM, Jusabani MA, Mandari FN, Dekker MCJ. The characteristics of traumatic spinal cord injuries at a referral hospital in Northern Tanzania. Spinal Cord Ser Cases. 2017;3:17021.
Nwankwo OE, Uche EO. Epidemiological and treatment profiles of spinal cord injury in southeast Nigeria. Spinal Cord. 2013;51:448–52.
Ametefe MK, Bankah PE, Yankey KP, Akoto H, Janney D, Dakurah TK. Spinal cord and spine trauma in a large teaching hospital in Ghana. Spinal Cord. 2016;54:1164–8.
Lehre MA, Eriksen LM, Tirsit A, Bekele S, Petros S, Park KB, et al. Outcome in patients undergoing surgery for spinal injury in an Ethiopian hospital. J Neurosurg Spine. 2015;23:772–9.
Rabiu TB. Clinical outcomes of posterior spinal stabilization with rigid vertical strut and spinal process wires (the Adeolu’s technique) in a developing country. Pan Afr Med J. 2017;26:84.
Choi JH, Park PJ, Din V, Sam N, Iv V, Park KB. Epidemiology and clinical management of traumatic spine injuries at a major government hospital in Cambodia. Asian Spine J. 2017;11:908–16.
Ojo OA, Poluyi EO, Owolabi BS, Kanu OO, Popoola MO. Surgical decompression for traumatic spinal cord injury in a tertiary center. Niger J Clin Pr. 2017;20:1455–60.
Magogo JLA, Mango M, Zuckerman SL, Leidinger A, Msuya S, Rutabasibwa N, et al. Operative treatment of traumatic spinal injuries in Tanzania: surgical management, neurologic outcomes, and time to surgery. Global Spine J. 2020. https://doi.org/10.1177/2192568219894956.
Schnake KJ, Schroeder GD, Vaccaro AR, Oner C. AOSpine classification systems (subaxial, thoracolumbar). J Orthop Trauma. 2017;31(Suppl 4):S14–S23.
Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M, et al. Reference for the 2011 revision of the international standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2011;34:547–54.
Aleem IS, DeMarco D, Drew B, Sancheti P, Shetty V, Dhillon M, et al. The burden of spine fractures in india: a prospective multicenter study. Glob Spine J. 2017;7:325–33.
Obalum DC, Giwa SO, Adekoya-Cole TO, Enweluzo GO. Profile of spinal injuries in Lagos, Nigeria. Spinal Cord. 2009;47:134–7.
Moshi H, Sundelin G, Sahlen KG, Sorlin A. Traumatic spinal cord injury in the north-east Tanzania—describing incidence, etiology and clinical outcomes retrospectively. Glob Health Action. 2017;10:1355604.
Admasu AK, Buno E. Short-term outcome in subaxial spine injury patients operated on in a resource-limited setting, Addis Ababa, Ethiopia. World Neurosurg. 2018;113:e702–6.
Lenehan B, Fisher CG, Vaccaro A, Fehlings M, Aarabi B, Dvorak MF. The urgency of surgical decompression in acute central cord injuries with spondylosis and without instability. Spine (Philos Pa 1976). 2010;35(21 Suppl):S180–S186.
Anderson KK, Tetreault L, Shamji MF, Singh A, Vukas RR, Harrop JS, et al. Optimal timing of surgical decompression for acute traumatic central cord syndrome: a systematic review of the literature. Neurosurgery. 2015;77(Suppl 4):S15–S32.
Roth EJ, Lawler MH, Yarkony GM. Traumatic central cord syndrome: clinical features and functional outcomes. Arch Phys Med Rehabil. 1990;71:18–23.
Adeolu AA, Komolafe EO, Kolawole OA. The technique of using rigid vertical strut and spinal process wire for posterior spinal stabilization. J Spinal Disord Tech. 2011;24:406–8.
Adeolu AA, Komolafe EO. Outcome of a posterior spinal fusion technique using spinous process wire and vertical strut. Ann Afr Med. 2014;13:30–34.
Thompson C, Mutch J, Parent S, Mac-Thiong JM. The changing demographics of traumatic spinal cord injury: an 11-year study of 831 patients. J Spinal Cord Med. 2015;38:214–23.
Leidinger A, Kim EE, Navarro-Ramirez R, Rutabasibwa N, Msuya SR, Askin G, et al. Spinal trauma in Tanzania: current management and outcomes. J Neurosurg Spine. 2019;31:103–11.
Author information
Authors and Affiliations
Contributions
NLL was responsible for statistical analysis, interpretation of the results, and writing the manuscript. AL was responsible for collection of data, interpretation of the results, and writing the manuscript. SLZ was responsible for conception of study design, interpretation of the results, and editing the manuscript. AL, NR, and HKS were responsible for interpretation of the results and editing the manuscript. RH was responsible for conception of study design, interpretation of the results, editing the manuscript, and supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed, including institutional review board approval.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lessing, N.L., Lazaro, A., Zuckerman, S.L. et al. Nonoperative treatment of traumatic spinal injuries in Tanzania: who is not undergoing surgery and why?. Spinal Cord 58, 1197–1205 (2020). https://doi.org/10.1038/s41393-020-0474-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-020-0474-y
This article is cited by
-
Central cord syndrome definitions, variations and limitations
Spinal Cord (2023)
-
Variation in global treatment for subaxial cervical spine isolated unilateral facet fractures
European Spine Journal (2021)