Abstract
Study design
Retrospective chart review.
Objectives
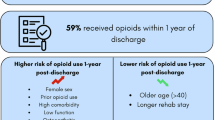
The objective of this study was to characterize opioid administration in people with acute SCI and examine the association between opioid dose and (1) changes in motor/functional scores from hospital to rehabilitation discharge, and (2) pain, depression, and quality of life (QOL) scores 1-year post injury.
Setting
Spinal Cord Injury Model System (SCIMS) inpatient acute rehabilitation facility.
Methods
Patients included in the SCIMS from 2008 to 2011 were linked to the National Trauma Registry and the electronic medical record. Three opioid dose groups (low, medium, and high) were defined based on the total morphine equivalence in milligrams at 24 h. The associations between opioid dose groups and functional/motor outcomes were assessed, as well as 1-year follow-up pain and QOL surveys.
Results
In all, 85/180 patients had complete medication records. By 24 h, all patients had received opioids. Patients receiving higher amounts of opioids had higher pain scores 1 year later compared with medium- and low-dose groups (pain levels 5.5 vs. 4 vs. 1, respectively, p = 0.018). There was also an 8× greater risk of depression 1 year later in the high-dose group compared with the low-dose group (OR: 8.1, 95% CI: 1.2–53.7). In analyses of motor scores, we did not find a significant interaction between opioid dose and duration of injury.
Conclusions
These preliminary findings suggest that higher doses of opioids administered within 24 h of injury are associated with increased pain in the chronic phase of people with SCI.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to large datasets without a comprehensive legend, but are available from the corresponding author on reasonable request.
References
Kumar R, Lim J, Mekary RA, Rattani A, Dewan MC, Sharif SY, et al. Traumatic spinal injury: global epidemiology and worldwide volume. World Neurosurg. 2018;113:e345–63.
Klingler HC, Pycha A, Schmidbauer J, Marberger M. Use of peripheral neuromodulation of the S3 region for treatment of detrusor overactivity: a urodynamic-based study. Urology. 2000;56:766–71.
Hook MA, Liu GT, Washburn SN, Ferguson AR, Bopp AC, Huie JR, et al. The impact of morphine after a spinal cord injury. Behav Brain Res. 2007;179:281–93.
Hook MA, Moreno G, Woller S, Puga D, Hoy K Jr., Balden R, et al. Intrathecal morphine attenuates recovery of function after a spinal cord injury. J Neurotrauma. 2009;26:741–52.
Hook MA, Washburn SN, Moreno G, Woller SA, Puga D, Lee KH, et al. An IL-1 receptor antagonist blocks a morphine-induced attenuation of locomotor recovery after spinal cord injury. Brain Behav Immun. 2011;25:349–59.
Woller SA, Moreno GL, Hart N, Wellman PJ, Grau JW, Hook MA. Analgesia or addiction?: implications for morphine use after spinal cord injury. J Neurotrauma. 2012;29:1650–62.
Woller SA, Malik JS, Aceves M, Hook MA. Morphine self-administration following spinal cord injury. J Neurotrauma. 2014;31:1570–83.
Hook MA, Woller SA, Bancroft E, Aceves M, Funk MK, Hartman J, et al. Neurobiological effects of morphine after spinal cord injury. J Neurotrauma. 2017;34:632–44.
Aceves M, Terminel MN, Okoreeh A, Aceves AR, Gong YM, Polanco A, et al. Morphine increases macrophages at the lesion site following spinal cord injury: protective effects of minocycline. Brain Behav Immun. 2019;79:125–38.
Scherrer JF, Salas J, Lustman PJ, Burge S, Schneider FD.Residency Research Network of Texas, et al. Change in opioid dose and change in depression in a longitudinal primary care patient cohort. Pain. 2015;156:348–55.
Scherrer JF, Svrakic DM, Freedland KE, Chrusciel T, Balasubramanian S, Bucholz KK, et al. Prescription opioid analgesics increase the risk of depression. J Gen Intern Med. 2014;29:491–9.
Ilgen MA, Bohnert AS, Ganoczy D, Bair MJ, McCarthy JF, Blow FC. Opioid dose and risk of suicide. Pain. 2016;157:1079–84.
Salas J, Scherrer JF, Schneider FD, Sullivan MD, Bucholz KK, Burroughs T, et al. New-onset depression following stable, slow, and rapid rate of prescription opioid dose escalation. Pain. 2017;158:306–12.
Hoffman JM, Bombardier CH, Graves DE, Kalpakjian CZ, Krause JS. A longitudinal study of depression from 1 to 5 years after spinal cord injury. Arch Phys Med Rehabil. 2011;92:411–8.
Cao Y, Massaro JF, Krause JS, Chen Y, Devivo MJ. Suicide mortality after spinal cord injury in the United States: injury cohorts analysis. Arch Phys Med Rehabil. 2014;95:230–5.
Neighbor ML, Honner S, Kohn MA. Factors affecting emergency department opioid administration to severely injured patients. Acad Emerg Med. 2004;11:1290–6.
Archer KR, Heins SE, Abraham CM, Obremskey WT, Wegener ST, Castillo RC. Clinical significance of pain at hospital discharge following traumatic orthopedic injury: general health, depression, and PTSD outcomes at 1 year. Clin J Pain. 2016;32:196–202.
Katz J, Seltzer Z. Transition from acute to chronic postsurgical pain: risk factors and protective factors. Expert Rev Neurother. 2009;9:723–44.
Kyranou M, Puntillo K. The transition from acute to chronic pain: might intensive care unit patients be at risk? Ann Intensive Care. 2012;2:36.
Opioid Coversion Calculator. 2016. https://www.practicalpainmanagement.com.
Poritz JMP, Mignogna J, Christie AJ, Holmes SA, Ames H. The Patient Health Questionnaire depression screener in spinal cord injury. J Spinal Cord Med. 2018;41:238–44.
Chen A, Ashburn MA. Cardiac effects of opioid therapy. Pain Med. 2015;16:S27–31.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7.
Chamberlain JD, Brinkhof MWG. Using strong inference to answer causal questions in spinal cord injury research. Spinal Cord. 2019;57:907–8.
Harvey LA. Relationships, associations, risk factors and correlations: nebulous phrases without obvious clinical implications. Spinal Cord. 2020;58:1–2.
Acknowledgements
We would like to acknowledge the Memorial Hermann—The Woodlands Trauma Services (Trauma Registry) for their assistance.
Funding
The research efforts of AS are supported by Mission Connect, a project of the TIRR Foundation. Further support was provided to AS and MH by Mission Connect Grants 016-104 and 016-115.
Author information
Authors and Affiliations
Contributions
AS was responsible for designing the study, linking the databases, extracting and analyzing data, interpreting results, writing the paper, and respondinging to revisions. CP was responsible for analyzing the data, interpreting results, writing the paper, and responding to revisions. JNB was responsible for extracting data and writing the paper. ARF and JLKK were responsible for guidance in statistical analyses and paper edits. MH was responsible for interpreting results, writing the paper, and respondinging to revisions.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
AS received approval for this study from the Institutional Review Board.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stampas, A., Pedroza, C., Bush, J.N. et al. The first 24 h: opioid administration in people with spinal cord injury and neurologic recovery. Spinal Cord 58, 1080–1089 (2020). https://doi.org/10.1038/s41393-020-0483-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-020-0483-x
This article is cited by
-
Impact of commonly administered drugs on the progression of spinal cord injury: a systematic review
Communications Medicine (2024)
-
Pharmacological management of acute spinal cord injury: a longitudinal multi-cohort observational study
Scientific Reports (2023)
-
Morphine-induced changes in the function of microglia and macrophages after acute spinal cord injury
BMC Neuroscience (2022)