Abstract
Study design
Retrospective comparative study.
Objective
Clinical prediction rules (CPRs) are an effervescent topic in the medical literature. Recovering ambulation after a traumatic spinal cord injury (tSCI) is a priority for patients and multiple CPRs have been proposed for predicting ambulation outcomes. Our objective is to confront clinical judgment to an established CPR developed for patients with tSCI.
Settings
Level one trauma center specialized in tSCI and its affiliated rehabilitation center.
Method
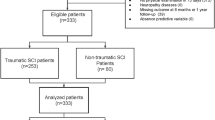
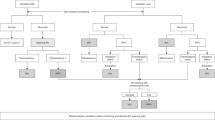
In this retrospective comparative study, six physicians had to predict the ambulation outcome of 68 patients after a tSCI based on information from the acute hospitalization. Ambulation was also predicted according to the CPR of van Middendorp (CPR-vM). The success rate of the CPR-vM and clinicians to predict ambulation was compared using criteria of 5% for defining clinical significance, and a level of statistical significance of 0.05 for bilateral McNemar tests.
Results
There was no statistical difference between the overall performance of physicians (success rate of 79%) and of the CPR-vM (81%) for predicting ambulation. The differences between the CPR-vM and physicians varied clinically and significantly with the level of experience, clinical setting, and field of expertise.
Conclusion
Confronting CPRs with the judgment of a group of clinicians should be an integral part of the design and validation of CPRs. Head-to-head comparison of CPRs with clinicians is also a cornerstone for defining the optimal strategy for translation into the clinical practice, and for defining which clinician and specific clinical context would benefit from using the CPR.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Cowley LE, Farewell DM, Maguire S, Kemp AM. Methodological standards for the development and evaluation of clinical prediction rules: a review of the literature. Diagn Progn Res. 2019;3:16.
Sanders S, Doust J, Glasziou P. A systematic review of studies comparing diagnostic clinical prediction rules with clinical judgment. PLoS One. 2015;10:e0128233.
Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ. 2015;350:g7594.
World Health Organization, International Spinal Cord Society, International Perspectives on Spinal Cord Injury. Geneva, Switzerland: World Health Organization. 2013.
van Middendorp JJ, Hosman AJF, Donders ART, Pouw MH, Ditunno JF Jr, Curt A, et al. A clinical prediction rule for ambulation outcomes after traumatic spinal cord injury: a longitudinal cohort study. Lancet.2011;377:1004–10.
Dalkilic T, Fallah N, Noonan VK, Salimi Elizei S, Dong K, Belanger L, et al. Predicting injury severity and neurological recovery after acute cervical spinal cord injury: a comparison of cerebrospinal fluid and magnetic resonance imaging biomarkers. J Neurotrauma. 2018;35:435–45.
Wilson JR, Grossman RG, Frankowski RF, Kiss A, Davis AM, Kulkarni AV, et al. A clinical prediction model for long-term functional outcome after traumatic spinal cord injury based on acute clinical and imaging factors. J Neurotrauma. 2012;29:2263–71.
Kaminski L, Cordemans V, Cernat E, M’Bra KI, Mac-Thiong JM. Functional outcome prediction after traumatic spinal cord injury based on acute clinical factors. J Neurotrauma. 2017;34:2027–33.
Facchinello Y, Beausejour M, Richard-Denis A, Thompson C, Mac-Thiong JM. The use of regression tree analysis for predicting the functional outcome following traumatic spinal cord injury. J Neurotrauma. 2017; https://doi.org/10.1089/neu.2017.5321.
Belliveau T, Jette AM, Seetharama S, Axt J, Rosenblum D, Larose D, et al. Developing artificial neural network models to predict functioning one year after traumatic spinal cord injury. Arch Phys Med Rehabil. 2016;97:1663–8.e3.
Simpson LA, Eng JJ, Hsieh JT, Wolfe DL. The health and life priorities of individuals with spinal cord injury: a systematic review. J Neurotrauma. 2012;29:1548–55.
Goulet J, Richard-Denis A, Thompson C, Mac-Thiong JM. Relationships between specific functional abilities and health-related quality of life in chronic traumatic spinal cord injury. Am J Phys Med Rehabil. 2019;98:14–19.
Hicks KE, Zhao Y, Fallah N, Rivers CS, Noonan VK, Plashkes T, et al. A simplified clinical prediction rule for prognosticating independent walking after spinal cord injury: a prospective study from a Canadian multicenter spinal cord injury registry. Spine J. 2017;17:1383–92.
van Silfhout L, Peters AE, Graco M, Schembri R, Nunn AK, Berlowitz DJ. Validation of the Dutch clinical prediction rule for ambulation outcomes in an inpatient setting following traumatic spinal cord injury. Spinal Cord. 2016;54:614–8.
Phan P, Budhram B, Zhang Q, Rivers CS, Noonan VK, Plashkes T, et al. Highlighting discrepancies in walking prediction accuracy for patients with traumatic spinal cord injury: an evaluation of validated prediction models using a Canadian Multicenter Spinal Cord Injury Registry. Spine J. 2019;19:703–10.
NSCISC National Spinal Cord Injury Statistical Center. Spinal Cord Injury Model Systems. Annual Report—Complete Public Version. 2019.
Coughlin KW. Medical decision-making in paediatrics: infancy to adolescence. Paediatr Child Health. 2018;23:138–46.
Acknowledgements
This research was funded by the Fonds de recherche du Québec – Santé and by the Medtronic Research Chair in Spine Trauma at Université de Montréal. The study cohort was retrieved from a prospective database previously funded by the Rick Hansen Spinal Cord Injury Registry and by the US Department of Defense Spinal Cord Injury Research Program.
Funding
Rick Hansen Spinal Cord Injury Registry, Fonds de recherche du Québec – Santé, Medtronic Research Chair in Spine Trauma at Université de Montréal.
Author information
Authors and Affiliations
Contributions
JMMT participated in the study design, data measurement, data analysis, drafting of the paper, revision and final acceptance of the paper, and securing funding. RPR participated in the study design, data measurement, data analysis, drafting of the paper, and revision and final acceptance of the paper. ARD participated in the study design, data measurement, data analysis, revision and final acceptance of the paper. JB participated in the study design, data collection, statistical analysis, and revision and final acceptance of the paper. EBM, JF, and SJ participated in data measurement, data analysis, and revision and final acceptance of the paper. GBV participated in data analysis and revision and final acceptance of the paper.
Corresponding author
Ethics declarations
Conflict of interest
All authors have completed the revised version of the ICMJE’s unified disclosure form (available on request from the corresponding author) and declare: JMMT reports grants from Fonds de recherche du Québec - Santé, grants from Medtronic research chair in spinal trauma at Université de Montréal, grants from Praxis Spinal Cord Institute, during the conduct of the study; other from Spinologics Inc., other from Medtronic, other from DePuy-Synthes, grants from Canadian Institutes of Health Research, grants from Craig H Neilsen Foundation, grants from Natural Sciences and Engineering Research Council of Canada, grants from Social Sciences and Humanities Research Council, grants from Canada Foundation for Innovation, grants from U.S. Department of Defense, grants from Medline Industries, grants from Vertex Pharmaceutical, outside the submitted work; RPR has nothing to disclose; ARD has nothing to disclose; SJ has nothing to disclose; EBM reports grants from Medtronic, grants from Depuy-Synthes, outside the submitted work; JF has nothing to disclose; GBV has nothing to disclose; JB reports personal fees from Medtronic research chair in spinal trauma at Université de Montréal, during the conduct of the study.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional ethical research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pelletier-Roy, R., Richard-Denis, A., Jean, S. et al. Clinical judgment is a cornerstone for validating and using clinical prediction rules: a head-to-head study on ambulation outcomes for spinal cord injured patients. Spinal Cord 59, 1104–1110 (2021). https://doi.org/10.1038/s41393-021-00632-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-021-00632-6