Abstract
Study design
Cross sectional.
Objectives
To identify variables associated with severe bowel symptoms in spinal cord injured people.
Setting
National cohort.
Methods
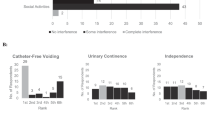
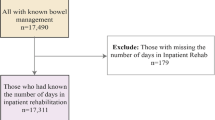
Adult spinal cord injured (SCI) people were recruited for an online registry and 1373 were included for analysis. Univariate analysis and logistic regression was used to evaluate associations between severity of bowel symptoms and variables. Bowel symptoms were assessed by the Neurogenic Bowel Dysfunction (NBD) score and patients scoring ≥14 were categorized as having severe bowel symptoms. Autonomic dysreflexia (AD) severity was measured using a six item questionnaire and reported as total AD score (0–24). Bladder management was categorized as: voiding, clean intermittent catheterization (CIC), surgery (augmentation/diversion) or indwelling catheter.
Results
Severe bowel symptoms were reported in 570 (42%) On multivariable logistic regression, every point increase of AD total score was associated with 5% increased odds of having more severe bowel symptoms [OR 1.05 95% CI 1.03–1.10]. Type of bladder management was also associated with more severe symptoms (p = 0.0001). SCI people with indwelling catheters (OR = 2.16, 95% CI 1.40–3.32) or reconstructive surgery (OR = 1.79, 95% CI 1.08–3.32) were almost twice as likely to report more severe bowel symptoms than those performing CIC.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
Data from this study are archived at the University of Utah and the University of Michigan.
References
Singh A, Tetreault L, Kalsi-Ryan S, Nouri A, Fehlings MG. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol. 2014;6:309–31.
Jain NB, Ayers GD, Peterson EN, Harris MB, Morse L, O’Connor KC, et al. Traumatic spinal cord injury in the United States, 1993-2012. JAMA. 2015;313:2236–43.
Crescenze IM, Lenherr SM, Myers JB, Elliott SP, Welk B, O’Dell D, et al. Self-reported urologic hospitalizations or emergency room visits in a contemporary spinal cord injury cohort. J Urol. 2020. https://doi.org/10.1097/JU.0000000000001386.
Chan BC, Cadarette SM, Wodchis WP, Krahn MD, Mittmann N. The lifetime cost of spinal cord injury in Ontario, Canada: a population-based study from the perspective of the public health care payer. J Spinal Cord Med. 2019;42:184–93.
Ng C, Prott G, Rutkowski S, Li Y, Hansen R, Kellow J, et al. Gastrointestinal symptoms in spinal cord injury: relationships with level of injury and psychologic factors. Dis Colon Rectum. 2005;48:1562–8.
Tate DG, Forchheimer M, Rodriguez G, Chiodo A, Cameron AP, Meade M, et al. Risk factors associated with neurogenic bowel complications and dysfunction in spinal cord injury. Arch Phys Med Rehabil. 2016;97:1679–86.
Stoffel JT, Van der Aa F, Wittmann D, Yande S, Elliott S. Neurogenic bowel management for the adult spinal cord injury patient. World J Urol. 2018;36:1587–92.
Cameron AP, Rodriguez GM, Gursky A, He C, Clemens JQ, Stoffel JT. The severity of bowel dysfunction in patients with neurogenic bladder. J Urol. 2015;194:1336–41.
Myers JB, Lenherr SM, Stoffel JT, Elliott SP, Presson AP, Zhang C, et al. Patient reported bladder related symptoms and quality of life after spinal cord injury with different bladder management strategies. J Urol. 2019;202:574–84.
Patel DP, Lenherr SM, Stoffel JT, Elliott SP, Welk B, Presson AP, et al. Study protocol: patient reported outcomes for bladder management strategies in spinal cord injury. BMC Urol. 2017;17:95.
Krogh K, Christensen P, Sabroe S, Laurberg S. Neurogenic bowel dysfunction score. Spinal Cord. 2006;44:625–31.
Welk B, Morrow S, Madarasz W, Baverstock R, Macnab J, Sequeira K. The validity and reliability of the neurogenic bladder symptom score. J Urol. 2014;192:452–7.
Ware J Jr., Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33.
Hubli M, Gee CM, Krassioukov AV. Refined assessment of blood pressure instability after spinal cord injury. Am J Hypertens. 2015;28:173–81.
Liu CW, Huang CC, Yang YH, Chen SC, Weng MC, Huang MH. Relationship between neurogenic bowel dysfunction and health-related quality of life in persons with spinal cord injury. J Rehabil Med. 2009;41:35–40.
Elmelund M, Klarskov N, Biering-Sorensen F. Fecal incontinence and neurogenic bowel dysfunction in women with traumatic and nontraumatic spinal cord injury. Dis Colon Rectum. 2019;62:1095–104.
White AR, Holmes GM. Anatomical and functional changes to the colonic neuromuscular compartment after experimental spinal cord injury. J Neurotrauma. 2018;35:1079–90.
Weld KJ, Dmochowski RR. Association of level of injury and bladder behavior in patients with post-traumatic spinal cord injury. Urology. 2000;55:490–4.
Musco S, Bazzocchi G, Martellucci J, Amato MP, Manassero A, Putignano D, et al. Treatments in neurogenic bowel dysfunctions: evidence reviews and clinical recommendations in adults. Eur J Phys Rehabil Med. 2020;56:741–55.
Hoen L, Ecclestone H, Blok BFM, Karsenty G, Phe V, Bossier R, et al. Long-term effectiveness and complication rates of bladder augmentation in patients with neurogenic bladder dysfunction: a systematic review. Neurourol Urodyn. 2017;36:1685–702.
Krassioukov A, Warburton DE, Teasell R, Eng JJ.Spinal Cord Injury Rehabilitation Evidence Research Team. A systematic review of the management of autonomic dysreflexia after spinal cord injury. Arch Phys Med Rehabil. 2009;90:682–95.
Guillot-Tantay C, Chartier-Kastler E, Perrouin-Verbe MA, Denys P, Leon P, Phe V. Complications of non-continent cutaneous urinary diversion in adults with spinal cord injury: a retrospective study. Spinal Cord. 2018;56:856–62.
Inskip JA, Lucci VM, McGrath MS, Willms R, Claydon VE. A community perspective on bowel management and quality of life after spinal cord injury: the influence of autonomic dysreflexia. J Neurotrauma. 2018;35:1091–105.
Author contributions
PBR—data analysis, manuscript writing. SML and JBM—study design, data analysis, manuscript edit. SPE, BW, and JTS—study design, data analysis. DO—data analysis.
Funding
Grant funding was obtained through Patient Centered Outcomes Research Institute (PCORI).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
PBR, SML, JBM, SPE and DO—no conflict. JTS—Editorial Board—J Urology, Leadership—Neurogenic Bladder Research Group.
Ethics approval
This study was approved and overseen by the University of Utah Internal Review Board. At each Co Investigator’s participating site (University of Michigan, University of Minnesota), institutional approval was obtained for the study IRB.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stoffel, J.T., Barboglio-Romo, P., Lenherr, S.M. et al. Factors impacting bowel symptoms in a contemporary spinal cord injury cohort: results from the Neurogenic Bladder Research Group Registry. Spinal Cord 59, 997–1002 (2021). https://doi.org/10.1038/s41393-021-00667-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-021-00667-9