Abstract
Study design
Mixed-methods observational study.
Objective
To describe the sleep-disordered breathing (SDB) management models of three spinal cord injury (SCI) rehabilitation centres that are screening, diagnosing and treating uncomplicated SDB, and to determine their common elements.
Setting
Three specialist SCI rehabilitation centres.
Methods
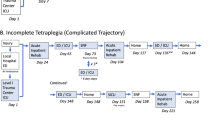
Data collection at each site included direct observations and interviews with lead clinical staff and an audit of SDB-related clinical practice in 2019. Detailed descriptions of the models of care, including process maps, were developed. A theory-based analysis of the common elements of the three care models was undertaken.
Results
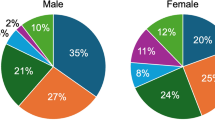
At each centre a multidisciplinary team, consisting of medical, allied health and/or nursing staff, provided a comprehensive SDB management service that included screening, diagnosis and treatment. Inpatients with SCI were assessed for SDB with overnight oximetry and/or polygraphy. Further assessment of patient symptoms, respiratory function, and hypercapnia supported the diagnostic process. Treatment with positive airway pressure was initiated on the ward. Having a collaborative, skilled team with strong leadership and adequate resources were the key, common enablers to providing the service.
Conclusion
It is feasible for multi-disciplinary SCI rehabilitation teams to independently diagnose and treat uncomplicated SDB without referral to specialist sleep services provided they are adequately resourced with equipment and skilled staff. Similar models of care could substantially improve access to SDB treatment for people with SCI. Further research is required to determine the non-inferiority of these alternatives to specialist care.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Graco M, McDonald L, Green SE, Jackson ML, Berlowitz DJ. Prevalence of sleep-disordered breathing in people with tetraplegia—a systematic review and meta-analysis. Spinal Cord. 2021;59:1–11.
Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81.
Berlowitz DJ, Spong J, Gordon I, Howard ME, Brown DJ. Relationships between objective sleep indices and symptoms in a community sample of people with tetraplegia. Arch Phys Med Rehabil. 2012;93:1246–52.
Schembri R, Spong J, Graco M, Berlowitz D. Neuropsychological function in patients with acute tetraplegia and sleep disordered breathing. Sleep. 2016;40:1–6.
Burns S, Kapur V, Yin K, Buhrer R. Factors associated with sleep apnea in men with spinal cord injury: a population-based case-control study. Spinal Cord. 2001;39:15–22.
Sankari A, Martin J, Badr M. A retrospective review of sleep-disordered breathing, hypertenstion and cardiovascular diseases in spinal cord injury patients. Spinal Cord. 2015;53:496.
Graco M, Berlowitz DJ, Green SE. Understanding the clinical management of obstructive sleep apnoea in tetraplegia: a qualitative study using the theoretical domains framework. BMC Health Serv Res. 2019;19:405.
Graco M, Green SE, Tolson J, Stevens B, Barnes M, Rigoni A, et al. Worth the effort? Weighing up the benefit and burden of continuous positive airway pressure therapy for the treatment of obstructive sleep apnoea in chronic tetraplegia. Spinal Cord. 2019;57:247.
Chai‐Coetzer CL, Antic NA, McEvoy RD. Ambulatory models of care for obstructive sleep apnoea: diagnosis and management. Respirology 2013;18:605–15.
Flemons WW, Douglas NJ, Kuna ST, Rodenstein DO, Wheatley J. Access to diagnosis and treatment of patients with suspected sleep apnea. Am J Respir Crit Care Med. 2004;169:668–72.
Antic NA, Buchan C, Esterman A, Hensley M, Naughton MT, Rowland S, et al. A randomized controlled trial of nurse-led care for symptomatic moderate–severe obstructive sleep apnea. Am J Respir Crit Care Med. 2009;179:501–8.
Chai-Coetzer CL, Antic NA, Rowland LS, Reed RL, Esterman A, Catcheside PG, et al. Primary care vs specialist sleep center management of obstructive sleep apnea and daytime sleepiness and quality of life: a randomized trial. JAMA 2013;309:997–1004.
Sánchez-Quiroga MÁ, Corral J, Gómez-de-Terreros FJ, Carmona-Bernal C, Asensio-Cruz MI, Cabello M, et al. Primary care physicians can comprehensively manage patients with sleep apnea. a noninferiority randomized controlled trial. Am J Respir Crit Care Med. 2018;198:648–56.
Chai-Coetzer C, Douglas J, McEvoy D. Guidelines for sleep studies in adults. a position statement of the Australasian Sleep Association. Sleep Med. 2017;36:S2–S22.
Respiratory Management Following Spinal Cord Injury: a Clinical Practice Guideline for Health-Care Professionals. Consortium for Spinal Cord Medicine; Paralyzed Veterans of America; 2005.
Graco M, Schembri R, Cross S, Thiyagarajan C, Shafazand S, Ayas NT, et al. Diagnostic accuracy of a two-stage model for detecting obstructive sleep apnoea in chronic tetraplegia. Thorax 2018;73:864–71.
Bauman KA, Kurili A, Schotland HM, Rodriguez GM, Chiodo AE, Sitrin RG. Simplified approach to diagnosing sleep-disordered breathing and nocturnal hypercapnia in individuals with spinal cord injury. Arch Phys Med Rehabil. 2016;97:363–71.
Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf health care. 2005;14:26–33.
Berlowitz DJ, Schembri R, Graco M, Ross JM, Ayas N, Gordon I, et al. Positive airway pressure for sleep-disordered breathing in acute quadriplegia: a randomised controlled trial. Thorax 2019;74:282–90.
Berlowitz DJ, Spong J, O’Donoghue FJ, Pierce RJ, Brown DJ, Campbell DA, et al. Transcutaneous measurement of carbon dioxide tension during extended monitoring: evaluation of accuracy and stability, and an algorithm for correcting calibration drift. Respir Care. 2011;56:442–8.
Sanders MH, Kern NB, Costantino JP, Stiller RA, Strollo PJ Jr, Studnicki KA, et al. Accuracy of end-tidal and transcutaneous PCO2 monitoring during sleep. Chest 1994;106:472–83.
Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, Caswell W, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof. 2006;26:13–24.
Michie S, Atkins L, West R. The behaviour change wheel. A guide to designing interventions 1st ed Great Britain: Silverback Publishing. 2014:1003–10.
Funding
MG’s travel to the three SCI rehabilitation centres was supported by the Queensland University of Technology (QuT) Alan-MacKay-Sim Spinal Cord Injury Travelling Fellowship.
Author information
Authors and Affiliations
Contributions
MG was responsible for designing the study, data collection and analysis, interpreting results, and writing the manuscript. DFO, CMO, MEB, GM, BD, BLK, HL were responsible for obtaining ethical approval and data collection at their sites. They all contributed to the interpretation of the results and manuscript preparation. DJB contributed to study design, interpretation of the results and manuscript preparation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Ethics approval was obtained from: • Horizon Health Network Research Ethics Board, New Brunswick, Canada (2020–2856). • Ethics Committee for Northwestern and Central Switzerland, Basil, Switzerland (2020–00180). • Medical ethics review committee, Amsterdam UMC, The Netherlands (2020.176). We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers/animals were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Graco, M., Gobets, D.F., M O’Connell, C. et al. Management of sleep-disordered breathing in three spinal cord injury rehabilitation centres around the world: a mixed-methods study. Spinal Cord 60, 414–421 (2022). https://doi.org/10.1038/s41393-022-00780-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-022-00780-3