Abstract
Objective
To systematically review the literature on penetrating spinal cord injury (PSCI) and evaluate current management strategies, their impact on patient functional outcomes, and treatment complications.
Methods
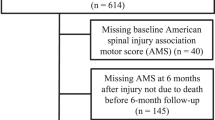
PubMed, Scopus, and Cochrane were searched based on the Preferred Reporting Items for Systematic-Reviews and Meta-Analyses (PRISMA) guidelines to include studies on penetrating spinal cord injury (PSCI).
Results
We included 10 articles comprising 1754 cases of PSCI. Mean age was 19.2 years (range, 16–70), and most patients were male (89.9%). Missile spinal cord injury (MSCI) was the most common type, affecting 1623 patients (92.6%), while non-missile spinal cord injury (NMSCI) accounted for only 131 cases (7.4%). Gunshots were the most common cause of MSCI, representing 87.2%, while knife stabs were the most common cause of NMSCI, representing 72.5%. A total of 425 patients (28.0%) underwent surgical intervention, and 1094 (72.0%) underwent conservative management. The conservative group had a higher rate of complete spine cord injury compared with the surgical group (61.5% vs. 49.2; p < 0.001). Although surgery yielded a higher score improvement rate compared with the conservative management (41.5% vs. 20.5%, p < 0.001), neither treatment strategy displayed superiority in improving neurological outcomes for neither complete SCIs (OR:0.7, 95% CI, 0.3–1.64; I2 = 44%, p = 0.13) nor for incomplete SCIs (OR:1.15, 95% CI, 0.64–2,06; I2 = 40%, p = 0.12).
Conclusion
Surgical and conservative management strategies proved to be equally effective on PSCI, irrespective of injury severity. Therefore, tailored treatment strategies for each patient and careful surgical selection is advised.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
Data were generated using the included articles’ reported data. Data are available from the corresponding author on reasonable request.
References
Morrow KD, Podet AG, Spinelli CP, Lasseigne LM, Crutcher CL, Wilson JD, et al. A case series of penetrating spinal trauma: Comparisons to blunt trauma, surgical indications, and outcomes. Neurosurg Focus. 2019;46:E4. https://doi.org/10.3171/2018.12.FOCUS18577.
Pedram H, Reza ZM, Reza RM, Vaccaro AR, Vafa RM. Spinal fractures resulting from traumatic injuries. Chin J Traumatol. 2010;13:3–9. https://doi.org/10.3760/cma.j.issn.1008-1275.2010.01.001.
Seroto PM, Harrington BM, Lombard C, Vlok AJ. The role of tertiary neurosurgical intervention in non-missile penetrating injuries of the spine. Eur Spine J. 2021;30:1397–401.
Hurlbert RJ. Editorial. penetrating spinal trauma: snapshot of the American epidemic. Neurosurg Focus FOC. 2019;46:E5.
Blair JA, Possley DR, Petfield JL, Schoenfeld AJ, Lehman RA, Hsu JR, et al. Military penetrating spine injuries compared with blunt. Spine J. 2012;12:762–8.
Iqbal N, Sharif S, Hafiz M, Ullah Khan A. Gunshot spinal injury: factors determining treatment and outcome. World Neurosurg. 2018;114:e706–e712.
Roach MJ, Chen Y, Kelly ML. Comparing blunt and penetrating trauma in spinal cord injury: analysis of long-term functional and neurological outcomes. Top Spinal Cord Inj Rehabil. 2018;24:121–32.
Scientific, Educational Abstracts, and Case-of-the-Day Presented at the ASER 2014 Annual Scientific Meeting and Postgraduate Course September 10–13, Portland, Oregon. Emerg Radiol. 2014;21:431–71.
Klimo PJ, Ragel BT, Rosner M, Gluf W, McCafferty R. Can surgery improve neurological function in penetrating spinal injury? a review of the military and civilian literature and treatment recommendations for military neurosurgeons. Neurosurg Focus. 2010;28:E4.
Gheban BA, Rosca IA, Crisan M. The morphological and functional characteristics of the pineal gland. Med Pharm Rep. 2019;92:226–34.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372. https://doi.org/10.1136/bmj.n71.
Joanna Briggs Institute Case Series. Checklist for Case Series. Joanna Briggs Inst. Crit. Apprais. tools use JBI Syst. Rev. 2017; 1–6.
Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, et al. The Oxford 2011 Levels of Evidence. Oxford Centre Evidence-Based Medicine. 2011.
Abbas A, Aziz HF, Rizvi R, Rehaman L, Javeed F, Afzal A, et al. Gunshot acquired spinal cord injury in civilians. Turk Neurosurg. 2019;29:506–12.
Kelly ML, Roach MJ, Nemunaitis G, Chen Y. Surgical and Nonsurgical Treatment of Penetrating Spinal Cord Injury: Analysis of Long-term Neurological and Functional Outcomes. Top Spinal Cord Inj Rehabil. 2019;25:186–93.
Waters RL, Sie I, Adkins RH, Yakura JS. Motor recovery following spinal cord injury caused by stab wounds: A multicenter study. Paraplegia. 1995;33:98–101.
Benzel EC, Hadden TA, Coleman JE. Civilian gunshot wounds to the spinal cord and cauda equina. Neurosurgery. 1987;20:281–5.
Robertson DP, Simpson RK. Penetrating injuries restricted to the cauda equina: a retrospective review. Neurosurgery. 1992;31:265–70.
Aarabi B, Alibaii E, Taghipur M, Kamgarpur A. Comparative study of functional recovery for surgically explored and conservatively managed spinal cord missile injuries. Neurosurgery. 1996;39:1133–40.
Kahraman S, Gonul E, Kayali H, Sirin S, Duz B, Beduk A, et al. Retrospective analysis of spinal missile injuries. Neurosurg Rev. 2004;27:42–45.
Bhatoe HS, Singh P. Missile injuries of the spine. Neurol India. 2003;51:507–11.
Rathore FA, Ayub A, Farooq S, New PW. Suicide bombing as an unusual cause of spinal cord injury: a case series from Pakistan. Spinal Cord. 2011;49:851–4.
Crutcher CL II, Wilson JM, DiGiorgio AM, Fannin ES, Shields JA, Morrow KD, et al. Minimally invasive management of civilian gunshot wounds to the lumbar spine: A case series and technical report. Oper Neurosurg. 2020;19:219–25.
Heary RF, Vaccaro AR, Mesa JJ, Balderston RA. Thoracolumbar infections in penetrating injuries to the spine. Orthop Clin North Am. 1996;27:69–81.
Platt A, Dafrawy MH EL, Lee MJ, H Herman M, Ramos E, et al. Gunshot Wounds to the Lumbosacral Spine: Systematic Review and Meta-Analysis. Glob spine J. 2021;21925682211030870. https://pubmed.ncbi.nlm.nih.gov/34275384/
Khorasanizadeh M, Yousefifard M, Eskian M, Lu Y, Chalangari M, Harrop JS, et al. Neurological recovery following traumatic spinal cord injury: a systematic review and meta-analysis. J Neurosurg Spine 2019;30:683–99.
Bumpass DB, Buchowski JM, Park A, Gray BL, Agarwal R, Baty J, et al. An Update on Civilian Spinal Gunshot Wounds: Treatment, Neurological Recovery, and Complications. Spine. 2015;40:450–61.
Bono CM, Heary RF. Gunshot wounds to the spine. Spine J. 2004;4:230–40.
Lawless MH, Lytle EJ, McGlynn AF, Engler JA. Surgical management of penetrating spinal cord injury primarily due to shrapnel and its effect on neurological outcome: a literature review and meta-analysis. J Neurosurg Spine. 2018;28:63–71.
Ahuja CS, Wilson JR, Nori S, Kotter MRN, Druschel C, Curt A, et al. Traumatic spinal cord injury. Nat Rev Dis Prim. 2017;3:17018.
Schwartz G, Fehlings MG. Secondary injury mechanisms of spinal cord trauma: a novel therapeutic approach for the management of secondary pathophysiology with the sodium channel blocker riluzole. Prog Brain Res. 2002;137:177–90.
Badhiwala JH, Ahuja CS, Fehlings MG. Time is spine: a review of translational advances in spinal cord injury. J Neurosurg Spine. 2018;30:1–18.
Choo AM, Liu J, Lam CK, Dvorak M, Tetzlaff W, Oxland TR, et al. Contusion, dislocation, and distraction: primary hemorrhage and membrane permeability in distinct mechanisms of spinal cord injury. J Neurosurg Spine. 2007;6:255–66.
LaPlaca MC, Simon CM, Prado GR, Cullen DK. CNS injury biomechanics and experimental models. Prog Brain Res. 2007;161:13–26.
Li S, Mealing GA, Morley P, Stys PK. Novel injury mechanism in anoxia and trauma of spinal cord white matter: glutamate release via reverse Na+-dependent glutamate transport. J Neurosci. 1999;19:RC16.
Kwon BK, Tetzlaff W, Grauer JN, Beiner J, Vaccaro AR. Pathophysiology and pharmacologic treatment of acute spinal cord injury. Spine J. 2004;4:451–64.
Cafferty WBJ, Duffy P, Huebner E, Strittmatter SM. MAG and OMgp synergize with Nogo-A to restrict axonal growth and neurological recovery after spinal cord trauma. J Neurosci. 2010;30:6825–37.
Chen MS, Huber AB, van der Haar ME, Frank M, Schnell L, Spillmann AA, et al. Nogo-A is a myelin-associated neurite outgrowth inhibitor and an antigen for monoclonal antibody IN-1. Nature. 2000;403:434–9.
Stefanopoulos PK, Soupiou OT, Pazarakiotis VC, Filippakis K. Wound ballistics of firearm-related injuries—part 2: mechanisms of skeletal injury and characteristics of maxillofacial ballistic trauma. Int J Oral Maxillofac Surg. 2015;44:67–78.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The study idea was proposed by [Othman Bin Alamer, MBBS] and [Ali S. Haider, BS]. The literature search, articles screen, and data extraction were perfumed by [Caren Stuebe, MSc], [Paolo Palmisciano, MD], [Lokeshwar S. Bhenderu, BS], [Navraj S. Sagoo, MD], [Maryam Haider, MD], and [Ali S. Haider, BS]. Data analysis was performed by [Othman Bin Alamer, MBBS]. The manuscript was drafted by [Othman Bin Alamer, MBBS]. All authors critically revised and edited the first draft and commented on all versions of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bin-Alamer, O., Bhenderu, L.S., Stuebe, C. et al. Penetrating spinal cord injury: a systematic review and meta-analysis of clinical features and treatment outcomes. Spinal Cord 60, 845–853 (2022). https://doi.org/10.1038/s41393-022-00813-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-022-00813-x