Abstract
Study design
Systematic Review and Meta-analysis.
Setting
Canada.
Objectives
Fatigue is one of the most common consequences of spinal cord injury (SCI). In this systematic review and meta-analysis, we examined interventions for fatigue in SCI and evaluated their effectiveness.
Methods
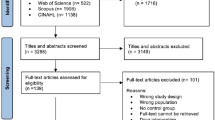
MEDLINE, EMBASE, CINAHL, and PsycINFO databases were searched up to January 2024 inclusive. Randomized controlled trials (RCTs) that assessed any intervention for at least one fatigue outcome in people with SCI were included. Study quality was assessed using the Cochrane Risk of Bias Tool.
Results
Initial screening identified 282 studies from which six RCTs were included in the review (N = 249). One study found that moderate-intensity arm-crank exercise significantly improved fatigue compared to a control group (p = 0.036) with a large effect size (standard mean difference [SMD] = 1.05; 95% confidence interval [CI], 0.10–2.00). Two studies assessing behavioral interventions found a moderate effect on fatigue (SMD = 0.46; 95% CI, −0.00–0.92; p = 0.05). Two studies did not find an effect of massage therapy on fatigue (SMD = 0.06; 95% CI, −0.38–0.50; p = 0.80). The risk of bias was classified as High for all but two of the RCTs.
Conclusions
These findings suggest that exercise and behavioral interventions promoting an active lifestyle may have a positive effect on fatigue. More research with larger sample sizes, including controls for co-morbid conditions like pain and depression, is needed to establish evidence-based treatments for reducing fatigue in people with SCI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
Anton HA, Miller WC, Townson AF, Imam B, Silverberg N, Forwell S. The course of fatigue after acute spinal cord injury. Spinal Cord. 2017;55:94–7.
Overman CL, Kool MB, Da Silva JAP, Geenen R. The prevalence of severe fatigue in rheumatic diseases: An International study. Clin Rheumatol. 2016;35:409–15.
Barone P, Antonini A, Colosimo C, Marconi R, Morgante L, Avarello TP, et al. The PRIAMO study: A multicenter Assessment of Nonmotor Symptoms and their impact on quality of life in Parkinson’s disease. Mov Disord. 2009;24:1641–9.
Oliva Ramirez A, Keenan A, Kalau O, Worthington E, Cohen L, Singh S. Prevalence and burden of multiple sclerosis-related fatigue: a systematic literature review. BMC Neurol. 2021;21:468.
Lidal IB, Lundberg Larsen K. Anxiety, depression, and fatigue in middle-aged and older persons with spina bifida: A Cross-sectional Study. Disabil Rehabil. 2022;44:7936–46.
Cumming TB, Packer M, Kramer SF, English C. The prevalence of fatigue after stroke: a systematic review and meta-analysis. Int J Stroke Off J Int Stroke Soc. 2016;11:968–77.
Fawkes-Kirby TM, Wheeler MA, Anton HA, Miller WC, Townson AF, Weeks CAO. Clinical correlates of fatigue in spinal cord injury. Spinal Cord. 2008;46:21–5.
Nooijen CFJ, Vogels S, Bongers-Janssen HMH, Bergen MP, Stam HJ, van den Berg-Emons HJG, et al. Fatigue in persons with subacute spinal cord injury who are dependent on a manual wheelchair. Spinal Cord. 2015;53:758–62.
Lidal IB, Jensen AE, Larsen TW, Stanghelle JK. Fatigue in persons who have lived with spinal cord injury for >20 years. Spinal Cord. 2013;51:103–8.
Kluger BM, Krupp LB, Enoka RM. Fatigue and fatigability in neurologic illnesses: proposal for a unified taxonomy. Neurology. 2013;80:409–16.
Hammell KW, Miller WC, Forwell SJ, Forman BE, Jacobsen BA. Fatigue and spinal cord injury: a qualitative analysis. Spinal Cord. 2009;47:44–9.
Hoogenes B, Querée M, Miller WC, Mortenson WB, Townson A, Eng JJ. Evidence on definitions, concepts, outcome instruments, and interventions for chronic fatigue in spinal cord injury: a scoping review protocol. JBI Evid Synth. 2021;19:1999.
Ibitoye MO, Hamzaid NA, Hasnan N, Abdul Wahab AK, Davis GM. Strategies for rapid muscle fatigue reduction during FES exercise in individuals with spinal cord injury: a systematic review. PloS One. 2016;11:e0149024.
Craig A, Tran Y, Guest R, Middleton J. Excessive daytime sleepiness in adults with spinal cord injury and Associations with Pain Catastrophizing and Pain Intensity. Spinal Cord. 2020;58:831–9.
Jensen MP, Kuehn CM, Amtmann D, Cardenas DD. Symptom burden in persons with spinal cord injury. Arch Phys Med Rehabil. 2007;88:638–45.
Wijesuriya N, Tran Y, Middleton J, Craig A. Impact of fatigue on the health-related quality of life in persons with spinal cord injury. Arch Phys Med Rehabil. 2012;93:319–24.
Christofi AASN, Tate DG, Witter C, Alonso AC, Greve JMD. Predictors of quality of life of individuals living in Brazil with spinal cord injury/disease. Spinal Cord. 2023;61:253–9.
Craig AR, Tran YH, Lovas JM, Middleton J. Spinal cord injury and its association with negative psychological states. Int J Psychosoc Rehabil. 2008;12:115–21.
van Diemen T, van Lankveld W, van Leeuwen C, Post M, van Nes I. Multidimensional fatigue during rehabilitation in persons with recently acquired spinal cord injury. J Rehabil Med. 2016;48:27–32.
Smith EM, Imam B, Miller WC, Silverberg ND, Anton HA, Forwell SJ, et al. The relationship between fatigue and participation in spinal cord injury. Spinal Cord. 2016;54:457–62.
Saunders LL, Krause JS, DiPiro ND, Kraft S, Brotherton S. Ambulation and complications related to assistive devices after spinal cord injury. J Spinal Cord Med. 2013;36:652–9.
McColl MA, Arnold R, Charlifue S, Glass C, Savic G, Frankel H. Aging, spinal cord injury, and quality of life: structural relationships. Arch Phys Med Rehabil. 2003;84:1137–44.
Alschuler KN, Jensen MP, Sullivan-Singh SJ, Borson S, Smith AE, Molton IR. The association of age, pain, and fatigue with physical functioning and depressive symptoms in persons with spinal cord injury. J Spinal Cord Med. 2013;36:483–91.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Ryan R. Cochrane consumers and communication group: meta-analysis. Cochrane Consumers and Communication Review Group: meta-analysis http://cccrg.cochrane.org, 2016 (accessed 11-12-2023)
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135.
Deeks J, Higgins JPT, Altman DG. Chapter 10: analysing data and under-taking meta-analyses. In: Cochrane handbook for systematic reviews of interventions version. 63 Cochrane; 2022. Available from https://training.cochrane.org/handbook/current
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions version 6.4. Cochrane; 2023. Available from https://training.cochrane.org/handbook/current
Nightingale TE, Rouse PC, Walhin JP, Thompson D, Bilzon JLJ. Home-based exercise enhances health-related quality of life in persons with spinal cord injury: a randomized controlled trial. Arch Phys Med Rehabil. 2018;99:1998–2006.e1.
Kooijmans H, Post MWM, Stam HJ, van der Woude LHV, Spijkerman DCM, Snoek GJ, et al. Effectiveness of a self-management intervention to promote an active lifestyle in persons with long-term spinal cord injury: The HABITS randomized clinical trial. Neurorehabil Neural Repair. 2017;31:991–1004.
Pourjafari Jorjafaki B, Hovanloo F, Mohammadi F. Effect of six weeks virtual reality-based rehabilitation exercise and reflexology on fatigue rate of paralyzed veterans. Iran J War Public Health. 2022;14:19–24.
Lovas J, Tran Y, Middleton J, Bartrop R, Moore N, Craig A. Managing pain and fatigue in people with spinal cord injury: a randomized controlled trial feasibility study examining the efficacy of massage therapy. Spinal Cord. 2017;55:162–6.
Chase T, Jha A, Brooks CA, Allshouse A. A pilot feasibility study of massage to reduce pain in people with spinal cord injury during acute rehabilitation. Spinal Cord. 2013;51:847–51.
Nooijen CFJ, Stam HJ, Schoenmakers I, Sluis TAR, Post MWM, Twisk JWR, et al. Working mechanisms of a behavioural intervention promoting physical activity in persons with subacute spinal cord injury. J Rehabil Med. 2016;48:583–8.
Curtis KJB, Hitzig SL, Leong N, Wicks CE, Ditor DS, Katz J. Evaluation of a modified yoga program for persons with spinal cord injury. Ther Recreation J. 2015;49:99–117.
Anton HA, Miller WC, Townson AF. Measuring fatigue in persons with spinal cord injury. Arch Phys Med Rehabil. 2008;89:538–42.
Craig A, Tran Y, Siddall P, Wijesuriya N, Lovas J, Bartrop R, et al. Developing a model of associations between chronic pain, depressive mood, chronic fatigue, and self-efficacy in people with spinal cord injury. J Pain. 2013;14:911–20.
Chalder T, Berelowitz G, Pawlikowska T, Watts L, Wessely S, Wright D, et al. Development of a fatigue scale. J Psychosom Res. 1993;37:147–53.
Kooijmans H, Post MWM, van der Woude LHV, de Groot S, Stam HJ, Bussmann JBJ. Randomized controlled trial of a self-management intervention in persons with spinal cord injury: design of the HABITS (Healthy Active Behavioural Intervention in SCI) study. Disabil Rehabil. 2013;35:1111–8.
Vestergaard M, Jensen K, Juul-Kristensen B. Hybrid high-intensity interval training using functional electrical stimulation leg cycling and arm ski ergometer for people with spinal cord injuries: A Feasibility study. Pilot Feasibility Stud. 2022;8:43.
Boutilier G, Sawatzky BJ, Grant C, Wiefelspuett S, Finlayson H. Spasticity changes in SCI following a dynamic standing program using the segway. Spinal Cord. 2012;50:595–8.
Shem K, Karasik D, Carufel P, Kao MC, Zheng P. Seated tai chi to alleviate pain and improve quality of life in individuals with spinal cord disorder. J Spinal Cord Med. 2016;39:353–8.
Postol N, Spratt NJ, Bivard A, Marquez J. Physiotherapy using a free-standing robotic exoskeleton for patients with spinal cord injury: A Feasibility study. J Neuroeng Rehabil. 2021;18:180.
Tawashy AE, Eng JJ, Lin KH, Tang PF, Hung C. Physical activity is related to lower levels of pain, fatigue and depression in individuals with spinal cord injury: A Correlational study. Spinal Cord. 2009;47:301–6.
Onate-Figuérez A, Avendaño-Coy J, Fernández-Canosa S, Soto-León V, López-Molina MI, Oliviero A. Factors associated with fatigue in people with spinal cord injury: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2023;104:132–42.
Neefkes-Zonneveld CR, Bakkum AJ, Bishop NC, van Tulder MW, Janssen TW. Effect of long-term physical activity and acute exercise on markers of systemic inflammation in persons with chronic spinal cord injury: a systematic review. Arch Phys Med Rehabil. 2015;96:30–42.
Tomasone JR, Wesch NN, Ginis KAM, Noreau L. Spinal cord injury, physical activity, and quality of life: a systematic review. Kinesiol Rev. 2013;2:113–29.
van der Scheer JW, Martin Ginis KA, Ditor DS, Goosey-Tolfrey VL, Hicks AL, West CR, et al. Effects of exercise on fitness and health of adults with spinal cord injury: a systematic review. Neurology. 2017;89:736–45.
Heine M, van de Port I, Rietberg MB, van Wegen EEH, Kwakkel G. Exercise therapy for fatigue in multiple sclerosis. Cochrane Database Syst Rev. 2015;2015:CD009956.
White PD, Goldsmith KA, Johnson AL, Potts L, Walwyn R, DeCesare JC, et al. Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome (PACE): a randomised trial. Lancet Lond Engl. 2011;377:823–36.
Estévez-López F, Maestre-Cascales C, Russell D, Álvarez-Gallardo IC, Rodriguez-Ayllon M, Hughes CM, et al. Effectiveness of exercise on fatigue and sleep quality in fibromyalgia: a systematic review and meta-analysis of randomized trials. Arch Phys Med Rehabil. 2021;102:752–61.
Zedlitz AMEE, Rietveld TCM, Geurts AC, Fasotti L. Cognitive and graded activity training can alleviate persistent fatigue after stroke: a randomized, controlled trial. Stroke. 2012;43:1046–51.
Ahlberg K, Ekman T, Gaston-Johansson F, Mock V. Assessment and management of cancer-related fatigue in adults. Lancet Lond Engl. 2003;362:640–50.
Wender CLA, Manninen M, O’Connor PJ. The effect of chronic exercise on energy and fatigue states: a systematic review and meta-analysis of randomized trials. Front Psychol. 2022;13:907637.
Puetz TW. Physical activity and feelings of energy and fatigue: epidemiological evidence. Sports Med. 2006;36:767–80.
Rosenthal TC, Majeroni BA, Pretorius R, Malik K. Fatigue: an overview. Am Fam Physician. 2008;78:1173–9.
Dukes JC, Chakan M, Mills A, Marcaurd M. Approach to fatigue: best practice. Med Clin North Am. 2021;105:137–48.
Wong AWK, Tomazin R, Walker K, Heeb Desai R, Hollingsworth H, Newland PK, et al. Text messaging intervention for fatigue self-management in people with stroke, spinal cord injury, and multiple sclerosis: A pilot study. Disabil Health J. 2024;17. https://doi.org/10.1016/j.dhjo.2023.101549
Vincent C, Gagnon DH, Dumont F, ADMI group. Pain, fatigue, function and participation among long-term manual wheelchair users partnered with a mobility service dog. Disabil Rehabil Assist Technol. 2019;14:99–108.
Bombardier CH, Cunniffe M, Wadhwani R, Gibbons LE, Blake KD, Kraft GH. The Efficacy of telephone counseling for health promotion in people with multiple sclerosis: a randomized controlled trial. Arch Phys Med Rehabil. 2008;89:1849–56.
Turner AP, Hartoonian N, Sloan AP, Benich M, Kivlahan DR, Hughes C, et al. Improving fatigue and depression in individuals with multiple sclerosis using telephone-administered physical activity counseling. J Consult Clin Psychol. 2016;84:297–309.
Pöttgen J, Moss-Morris R, Wendebourg JM, Feddersen L, Lau S, Köpke S, et al. Randomised controlled trial of a self-guided online fatigue intervention in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2018;89:970–6.
Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215.
Wang E, Chang JHC, Plow M. Predictors of fatigue self-management behaviors in adults with multiple sclerosis. NeuroRehabilitation. 2022;50:75–87.
Zhang T, Yan HX, An Y, Yin L, Sun PP, Zhao JN, et al. The efficacy and safety of manual therapy for symptoms associated with multiple sclerosis: a systematic review and meta-analysis. J Integr Complement Med. 2022;28:780–90.
Chiodo AE, Sitrin RG, Bauman KA. Sleep disordered breathing in spinal cord injury: a systematic review. J Spinal Cord Med. 2016;39:374–82.
Proserpio P, Lanza A, Sambusida K, Fratticci L, Frigerio P, Sommariva M, et al. Sleep apnea and periodic leg movements in the first year after spinal cord injury. Sleep Med. 2015;16:59–66.
Levine J, Greenwald BD. Fatigue in parkinson disease, stroke, and traumatic brain injury. Phys Med Rehabil Clin N Am. 2009;20:347–61.
Lee AKY, Miller WC, Townson AF, Anton HA, F2N2 Research Group. Medication use is associated with fatigue in a sample of community-living individuals who have a spinal cord injury: a chart review. Spinal Cord. 2010;48:429–33.
Hourihan SJ. Managing fatigue in adults with multiple sclerosis. Nurs Stand. 2015;29:51–8. https://doi.org/10.7748/ns.29.43.51.e9654.
Craig A, Tran Y, Wijesuriya N, Middleton J. Fatigue and tiredness in people with spinal cord injury. J Psychosom Res. 2012;73:205–10.
Hammell KW, Miller WC, Forwell SJ, Forman BE, Jacobsen BA. Managing fatigue following spinal cord injury: a qualitative exploration. Disabil Rehabil. 2009;31:1437–45.
Acknowledgements
We thank Paul Mackie for providing valuable feedback during the preparation of the draft of this manuscript.
Funding
The authors disclose receipt of financial support for the research, authorship, and publication of this article: Praxis Spinal Cord Institute [Praxis Grant # G2023-22-A1].
Author information
Authors and Affiliations
Consortia
Contributions
GM, MQ, and JE were responsible for the conceptualization and design of the study. JE is responsible for the overall content as guarantor. GM and CLCH were responsible for the selection of articles and data extraction. GM, CLCH, and MQ were responsible for further data extraction and risk of bias assessment with justification. GM, MQ, JE, and CLCH were responsible for assessing study methodologies. CLCH and MQ were responsible for preparing the tables. CLCH and JE were responsible for the meta-analysis. CLCH, GM, MQ, BH, EAB, EL, WCM, WBM, AT, and JE were responsible for writing and editing the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cano-Herrera, C.L., Manhas, G., Querée, M. et al. Treatments of fatigue after spinal cord injury: a systematic review and meta-analysis. Spinal Cord 63, 149–158 (2025). https://doi.org/10.1038/s41393-025-01067-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41393-025-01067-z