Abstract
Study Design
Retrospective comparative study.
Objectives
To compare surgical and clinical outcomes of thoracic intradural extramedullary (IDEM) meningiomas based on tumor location, specifically between ventral and dorsal/lateral lesions.
Methods
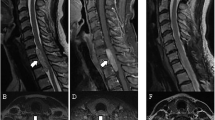
This study retrospectively analyzed 60 consecutive patients who underwent posterior surgical resection for thoracic IDEM meningiomas at a single institution between 2007 and 2022. Patients were stratified into two groups according to tumor location on preoperative MRI: Ventral group (n = 23) and Dorsal/Lateral group (n = 37). Clinical outcomes were assessed using the modified McCormick scale (MMCS). Surgical parameters and complications were also compared.
Results
Patients in the Ventral group had significantly larger sagittal tumor diameters and higher spinal canal occupancy rates than those in the Dorsal/Lateral group (p < 0.05). Preoperative motor deficits were more frequent in the Ventral group (86.9 vs. 51.3%, p < 0.01). Estimated blood loss was greater in the Ventral group (p = 0.01). Intraoperative motor evoked potential deterioration occurred more often (p = 0.04). Although both groups showed neurological improvement postoperatively, the percentage of patients reaching MMCS Grade I at final follow-up was significantly lower in the Ventral group (17.3 vs. 54.0%, p < 0.01). No tumor recurrence was observed in either group during the follow-up period (mean: 61.4 months).
Conclusions
Ventrally located thoracic IDEM meningiomas are associated with more severe preoperative motor dysfunction and inferior postoperative neurological recovery compared to dorsal/lateral lesions. These findings highlight the importance of early surgical intervention and tailored surgical planning for ventral tumors to optimize functional outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Riad H, Knafo S, Segnarbieux F, Lonjon N. Spinal meningiomas: surgical outcome and literature review. Neurochirurgie. 2013;59:30–4.
Ostrom QT, Price M, Neff C, Cioffi G, Waite KA, Kruchko C, et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the united states in 2015-2019. Neuro Oncol. 2022;24:v1–95.
Sandalcioglu IE, Hunold A, Muller O, Bassiouni H, Stolke D, Asgari S. Spinal meningiomas: critical review of 131 surgically treated patients. Eur Spine J. 2008;17:1035–41.
El-Hajj VG, Pettersson-Segerlind J, Fletcher-Sandersjoo A, Edstrom E, Elmi-Terander A. Current knowledge on spinal meningiomas epidemiology, tumor characteristics and non-surgical treatment options: a systematic review and pooled analysis (Part 1). Cancers. 2022;14:6251.
Dang DD, Mugge LA, Awan OK, Gong AD, Fanous AA. Spinal meningiomas: a comprehensive review and update on advancements in molecular characterization, diagnostics, surgical approach and technology, and alternative therapies. Cancers. 2024;16:1426.
Takami T, Naito K, Yamagata T, Yoshimura M, Arima H, Ohata K. Posterolateral approach for spinal intradural meningioma with ventral attachment. J Craniovertebr Junction Spine. 2015;6:173–8.
Notani N, Miyazaki M, Kanezaki S, Ishihara T, Kawano M, Tsumura H. Surgical management of ventrally located spinal meningiomas via posterior approach. Eur J Orthop Surg Traumatol. 2017;27:181–6.
Kobayashi K, Ando K, Matsumoto T, Sato K, Kato F, Kanemura T, et al. Clinical features and prognostic factors in spinal meningioma surgery from a multicenter study. Sci Rep. 2021;11:11630.
Simpson MT, Sneddon KJ. Extracranial meningioma of the oral cavity. Br J Oral Maxillofac Surg. 1987;25:520–5.
Nakamura M, Tsuji O, Fujiyoshi K, Hosogane N, Watanabe K, Tsuji T, et al. Long-term surgical outcomes of spinal meningiomas. Spine. 2012;37:E617–23.
Ridolfi D, Oyekan AA, Tang MY, Chen SR, Como CJ, Dalton J, et al. Modified clavien-dindo-sink classification system for operative complications in adult spine surgery. J Neurosurg Spine. 2024;40:669–73.
McCormick PC, Stein BM. Intramedullary tumors in adults. Neurosurg Clin N Am. 1990;1:609–30.
Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K. Interobserver and intraobserver reliability of the japanese orthopaedic association scoring system for evaluation of cervical compression myelopathy. Spine. 2001;26:1890–4.
Corell A, Cerbach C, Hoefling N, Bjorkman-Burtscher IM, Jakola AS. Spinal cord compression in relation to clinical symptoms in patients with spinal meningiomas. Clin Neurol Neurosurg. 2021;211:107018.
Ono K, Shimizu T, Fujibayashi S, Otsuki B, Murata K, Sakamoto A, et al. Predictive value of heterogeneously enhanced magnetic resonance imaging findings with computed tomography evidence of calcification for severe motor deficits in spinal meningioma. Neurospine. 2021;18:163–9.
Yamaguchi S, Menezes AH, Shimizu K, Woodroffe RW, Helland LC, Hitchon PW, et al. Differences and characteristics of symptoms by tumor location, size, and degree of spinal cord compression: a retrospective study on 53 surgically treated, symptomatic spinal meningiomas. J Neurosurg Spine. 2020;32:931–40.
Onishi E, Fujibayashi S, Otsuki B, Tsubouchi N, Tsutumi R, Ota M, et al. Risk factors for preoperative neurological impairment in patients with spinal meningioma: A retrospective multicenter study. J Clin Neurosci. 2024;126:187–93.
Gottfried ON, Gluf W, Quinones-Hinojosa A, Kan P, Schmidt MH. Spinal meningiomas: surgical management and outcome. Neurosurg Focus. 2003;14:e2.
Kim CH, Chung CK. Surgical outcome of a posterior approach for large ventral intradural extramedullary spinal cord tumors. Spine. 2011;36:E531–7.
Angevine PD, Kellner C, Haque RM, McCormick PC. Surgical management of ventral intradural spinal lesions. J Neurosurg Spine. 2011;15:28–37.
Fehlings MG, Quddusi A, Skelly AC, Brodt ED, Moghaddamjou A, Malvea A, et al. Definition, frequency and risk factors for intra-operative spinal cord injury: a knowledge synthesis. Glob Spine J. 2024;14:80S–104.
Evaniew N, Davies B, Farahbakhsh F, Fehlings MG, Ganau M, Graves D, et al. Interventions to optimize spinal cord perfusion in patients with acute traumatic spinal cord injury: an updated systematic review. Glob Spine J. 2024;14:58S–79.
Kwon BK, Tetreault LA, Martin AR, Arnold PM, Marco RAW, Newcombe VFJ, et al. A clinical practice guideline for the management of patients with acute spinal cord injury: recommendations on hemodynamic management. Glob Spine J. 2024;14:187S–211.
Saito T, Arizono T, Maeda T, Terada K, Iwamoto Y. A novel technique for surgical resection of spinal meningioma. Spine. 2001;26:1805–8.
Tominaga H, Kawamura I, Ijiri K, Yone K, Taniguchi N. Surgical results of the resection of spinal meningioma with the inner layer of dura more than 10 years after surgery. Sci Rep. 2021;11:4050.
Acknowledgements
In preparing this manuscript, ChatGPT (OpenAI) and Grammarly (Grammarly Inc.) were used to refine grammar and correct typographical errors. These tools were used solely to enhance clarity and readability without altering the scientific content or interpretation of the findings.
Funding
This study received no financial support for this research, authorship, and publication of this article.
Author information
Authors and Affiliations
Contributions
YS contributed to the data collection, data analysis, data interpretation and preparation of the initial draft of the manuscript. NN contributed to the study design, data analysis, data interpretation, and assistance with manuscript preparation. TO, MO, SS, KT, TI were responsible for the data collection and interpretation of the results. MM, MN, KW were responsible for the interpretation of the results, and supervision of the manuscript. All authors critically reviewed and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics Approval and Consent to Participate
This study received ethical approval from the institutional review board of the Ethics Committee of the Keio University School of Medicine (20110142). We certify that all applicable institutional regulations concerning the ethical use of human volunteers were followed during the research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Suematsu, Y., Nagoshi, N., Okubo, T. et al. Comparison of surgical and clinical outcomes between ventral and dorsal/lateral thoracic intradural extramedullary meningiomas: a retrospective study. Spinal Cord (2025). https://doi.org/10.1038/s41393-025-01132-7
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41393-025-01132-7