Abstract
Study design
Cross-sectional observational study.
Objectives
Deep-tissue injury (DTI) originates in subcutaneous soft tissue and progresses outward without early skin changes, making diagnosis difficult in people with spinal-cord injury (SCI). We evaluated the incidence of DTI with magnetic resonance imaging (MRI) and sought associated risk factors.
Setting
Kibikogen Rehabilitation Center for Employment Injuries, Japan.
Methods
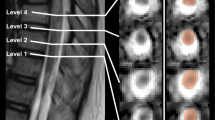
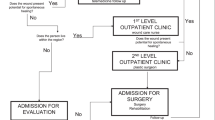
Fifty-six wheelchair-dependent adults with SCI of at least 1 month’s duration underwent pelvic sagittal STIR MRI screening. DTI-positive sites were defined by signal changes in subcutaneous fat or muscle. Ultrasonography, body composition, seating-related variables, and laboratory data were collected concurrently. Univariate and multivariate logistic-regression analyses identified independent risk factors.
Results
MRI detected subclinical DTI in 33 of 112 ischial regions (29.5%). Ultrasonography was concordant in only 15 sites (45.5%). Multivariable analysis showed that longer daily wheelchair use (p = 0.018), greater subcutaneous-tissue thickness at the ischial tuberosities (p = 0.028), and less-frequent pressure-relief manoeuvres (p = 0.031; protective) were independently associated with DTI. BMI, peak interface pressure, and routine haematologic or nutritional markers were not significant.
Conclusions
MRI screening revealed subclinical DTI in nearly one-third of wheelchair-dependent patients with SCI and outperformed ultrasonography for early detection. Extended sitting time, thicker subcutaneous fat at the ischial tuberosity, and infrequent pressure relief emerged as modifiable risk factors. A risk-based MRI surveillance strategy may enable timely preventive interventions and reduce progression to overt pressure ulcers.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
De-identified data are available from the corresponding author upon reasonable request and with IRB approval.
References
Kottner J, Cuddigan J, Carville K, Balzer K, Berlowitz D, Law S, et al. Prevention and treatment of pressure ulcers/injuries: The protocol for the second update of the international Clinical Practice Guideline 2019. J Tissue Viability. 2019;28:51–8.
Agam L, Gefen A. Pressure ulcers and deep tissue injury: a bioengineering perspective. J Wound Care. 2007;16:336–42.
Ankrom MA, Bennett RG, Sprigle S, Langemo D, Black JM, Berlowitz DR, et al. National pressure ulcer advisory panel. pressure-related deep tissue injury under intact skin and the current pressure ulcer staging systems. Adv Skin Wound Care. 2005;18:35–42.
Elsner JJ, Gefen A. Is obesity a risk factor for deep tissue injury in patients with spinal cord injury? J Biomech. 2008;41:3322–31.
Quintavalle PR, Lyder CH, Mertz PJ, Phillips-Jones C, Dyson M. Use of high-resolution, high-frequency diagnostic ultrasound to investigate the pathogenesis of pressure ulcer development. Adv Skin Wound Care. 2006;19:498–505.
Tsokos M, Heinemann A, Püschel K. Pressure sores: epidemiology, medico-legal implications and forensic argumentation concerning causality. Int J Leg Med. 2000;113:283–7.
Aoi N, Yoshimura K, Kadono T, Nakagami G, Iizuka S, Higashino T, et al. Ultrasonographic assessment of deep tissue injury. J Tissue Viability. 2009;18:67–74.
Swaine JM, Breidahl W, Bader DL, Oomens CWJ, O’Loughlin E, Santamaria N, et al. Ultrasonography detects deep tissue injuries in the subcutaneous layers of the buttocks following spinal cord injury. Top Spinal Cord Inj Rehabil. 2018;24:371–8.
Sakata Y, Namba T, Umemoto Y, Yoshikawa T, Furusawa K, Asamura S. “Comparing ultrasonography with magnetic resonance imaging in the detection of deep tissue injury”. Wounds. 2024;36:366–70.
Linder-Ganz E, Gefen A. Mechanical compression-induced pressure sores in rat hindlimb: Muscle stiffness, histology, and computational models. J Appl Physiol. 2007;102:2002–13.
Kanno N, Nakamura T, Yamanaka M, Kouda K, Nakamura T, Tajima F. Low-echoic lesions underneath the skin in subjects with spinal-cord injury. Spinal Cord. 2009;47:225–9.
Doridam J, Macron A, Vergari C, Verney A, Rohan PY, Pillet H. Feasibility of sub-dermal soft tissue deformation assessment using B-mode ultrasound for pressure ulcer prevention. J Tissue Viability. 2018;27:238–43.
Gefen A, Farid KJ, Shaywitz I. A review of deep tissue injury development, detection, and prevention: shear savvy. Ostomy Wound Manage. 2013;59:26–35.
Gefen A. Deep tissue injury from a bioengineering point of view. Ostomy Wound Manage. 2009;55:26–36.
Stekelenburg A, Gawlitta D, Bader DL, Oomens CW. Deep tissue injury: how deep is our understanding? Arch Phys Med Rehabil. 2008;89:1410–3.
Gawlitta D, Li W, Oomens CW, Baaijens FP, Bader DL, Bouten CV. The relative contributions of compression and hypoxia to development of muscle tissue damage: an in vitro study. Ann Biomed Eng. 2007;35:273–84.
Doughty D, Ramundo J, Bonham P, Beitz J, Erwin-Toth P, Anderson R, et al. Issues and challenges in staging of pressure ulcers. J Wound Ostomy Cont Nurs. 2006;33:125–30.
Berlowitz DR, Brienza DM. Are all pressure ulcers the result of deep tissue injury? a review of the literature. Ostomy Wound Manage. 2007;53:34–38.
Kawasaki S, Nishimura Y, Kouda K, Umemoto Y, Kinoshita T, Hashizaki T, et al. Follow-up study of subdermal low-echoic lesions in the ischial region in wheelchair users with spinal cord injuries. Front Med. 2022;9:848338.
Honaker J, Brockopp D, Moe K. Suspected deep tissue injury profile: a pilot study. Adv Skin Wound Care. 2014;27:133–40.
Author information
Authors and Affiliations
Contributions
YS designed the study, performed MRI and ultrasonographic evaluations, analyzed data, and drafted the manuscript. TN contributed to study design, patient recruitment, and data interpretation. YU and TY contributed to data collection, clinical assessment, and critical review of the manuscript. KF supervised the clinical and statistical analysis and contributed to manuscript revision. GY assisted with data analysis and figure preparation. SA supervised the entire project, provided critical revisions, and approved the final version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Approved by the Institutional Review Board of Wakayama Medical University (Approval No. 3303). All methods were performed in accordance with the relevant guidelines and regulations, including the Declaration of Helsinki. Written informed consent was obtained from all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sakata, Y., Namba, T., Umemoto, Y. et al. Deep tissue injury in patients with spinal cord injury: a magnetic resonance imaging–based risk assessment study. Spinal Cord (2025). https://doi.org/10.1038/s41393-025-01150-5
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41393-025-01150-5