Abstract
Introduction
Of the 23 cases of spinal intradural-extramedullary ependymomas which have been reported to date, 11 were diagnosed as anaplastic. Here we present a very rare case of a thoracic intradural-extramedullary (not intramedullary) anaplastic ependymoma in an adult along with a literature review.
Case presentation
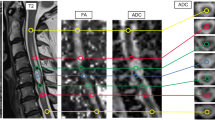
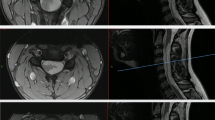
A 29-year-old man presented with rapidly progressive gait disturbance, a sensory-deficit below the trunk and urination disorders that had begun a few months earlier. Magnetic resonance imaging of his thoracic spine revealed a dorsal-located intradural-extramedullary tumor at T4-5. The rapid deterioration of his symptoms within several months led him to refer to our department for surgery. Within one month the size of tumor increased to involve the T4-6 level, consequently worsening his gait disturbance. He underwent surgery and tumor mass was resected. However, there was leptomeningeal dissemination of the tumor cells on the surface of cord. A near-total resection was therefore achieved. Histopathology revealed the resected specimen had immunoreactivity for EMA/Vimentin/CD56/CD99/S-100/GFAP, with a Ki-67 index of ~35%. These factors led to the diagnosis of anaplastic ependymoma. Seven weeks postoperatively he received adjuvant radiotherapy to the whole brain and the whole spinal cord. He recovered as an independent ambulator without recurrence 1 year postoperatively.
Discussion
Because of their rarity, there are no clear treatment or adjuvant therapy guidelines for spinal anaplastic ependymoma. Adjuvant radiotherapy to the whole brain and spinal cord was necessarily indicated after near-total resection. Although the patient’s condition has not recurred 1 year after surgery, careful and serial follow-up is necessary for this individual.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Guarnieri G, Tecame M, Izzo R, Zeccolini F, Genovese L, Muto M. Multisegmental diffuse intradural extramedullary ependymoma. An extremely rare case. Neuroradiol J. 2014;27:179–85.
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97–109.
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131:803–20.
Lee CH, Chung CK, Kim CH. Genetic differences on intracranial versus spinal cord ependymal tumors: a meta-analysis of genetic researches. Eur Spine J. 2016;25:3942–51.
Liu X, Sun B, Xu Q, Che X, Hu J, Gu S, et al. Outcomes in treatment for primary spinal anaplastic ependymomas: a retrospective series of 20 patients. J Neurosurg Spine. 2013;19:3–11.
Pomeraniec IJ, Dallapiazza RF, Sumner HM, Lopes MB, Shaffrey CI, Smith JS. Anaplastic extramedullary cervical ependymoma with leptomeningeal metastasis. J Clin Neurosci. 2015;22:1871–6.
Chakravorty A, Frydenberg E, Shein TT, Ly J, Earls P, Steel T. Multifocal intradural extramedullary anaplastic ependymoma of the spine. J Spine Surg. 2017;3:727–31.
Oliver B, de Castro A, Sarmiento MA, Arguello C, Blazquez MG. [Dorsal extramedullary ependymoma (author’s transl)]. Arch Neurobiol. 1981;44:215–24.
Katoh S, Ikata T, Inoue A, Takahashi M. Intradural extramedullary ependymoma. A case report. Spine (Philos Pa 1976). 1995;20:2036–8.
Robles SG, Saldana C, Boto GR, Martinez A, Zamarron AP, Jorquera M, et al. Intradural extramedullary spinal ependymoma: a benign pathology? Spine (Philos Pa 1976). 2005;30:E251–4.
Cerase A, Venturi C, Oliveri G, De Falco D, Miracco C. Intradural extramedullary spinal anaplastic ependymoma- case illustration. J Neurosurg Spine. 2006;5:476.
Schuurmans M, Vanneste JA, Verstegen MJ, van Furth WR. Spinal extramedullary anaplastic ependymoma with spinal and intracranial metastases. J Neurooncol. 2006;79:57–9.
Guppy KH, Hou L, Moes GS, Sahrakar K. Spinal intradural, extramedullary anaplastic ependymoma with an extradural component: case report and review of the literature. Surg Neurol Int. 2011;2:119.
Kinsman MJ, Callahan JD, Hattab EM, Cohen-Gadol AA. Extramedullary spinal ependymoma: a diagnostic challenge and review of the literature. Clin Neurol Neurosurg. 2011;113:661–4.
Kim BS, Kim SW, Kwak KW, Choi JH. Extra and intramedullary anaplastic ependymoma in thoracic spinal cord. Korean J Spine. 2013;10:177–80.
Matsuyama Y, Sakai Y, Katayama Y, Imagama S, Ito Z, Wakao N, et al. Surgical results of intramedullary spinal cord tumor with spinal cord monitoring to guide extent of resection. J Neurosurg Spine. 2009;10:404–13.
Nishikawa R. Pediatric and adult gliomas: how different are they? Neuro Oncol. 2010;12:1203–4.
Ellison DW, Kocak M, Figarella-Branger D, Felice G, Catherine G, Pietsch T, et al. Histopathological grading of pediatric ependymoma: reproducibility and clinical relevance in European trial cohorts. J Negat Results Biomed. 2011;10:7.
Li TY, Chu JS, Xu YL, Yang J, Wang J, Huang YH, et al. Surgical strategies and outcomes of spinal ependymomas of different lengths: analysis of 210 patients: clinical article. J Neurosurg Spine. 2014;21:249–59.
Manasa LP, Uppin MS, Sundaram C. Correlation of p53 and KI-67 expression with grade and subtype of ependymoma. Indian J Pathol Microbiol. 2012;55:308–13.
Zawrocki A, Izycka-Swieszewska E, Papierz W, Liberski PP, Zakrzewski K, Biernat W. Analysis of the prognostic significance of selected morphological and immunohistochemical markers in ependymomas, with literature review. Folia Neuropathol. 2011;49:94–102.
Tsuji O, Nagoshi N, Ishii R, Nori S, Suzuki S, Okada E et al. Poor prognostic factors for surgical treatment of spinal intramedullary ependymoma (World Health Organization Grade II). Asian Spine J. 2020. https://doi.org/10.31616/asj.2020.0064 [Epub ahead of print].
Karikari IO, Nimjee SM, Hodges TR, Cutrell E, Hughes BD, Powers CJ, et al. Impact of tumor histology on resectability and neurological outcome in primary intramedullary spinal cord tumors: a single-center experience with 102 patients. Neurosurgery. 2011;68:188–97. Discussion 197.
Volpp PB, Han K, Kagan AR, Tome M. Outcomes in treatment for intradural spinal cord ependymomas. Int J Radiat Oncol Biol Phys. 2007;69:1199–204.
Kobayashi K, Ando K, Kato F, Kanemura T, Sato K, Kamiya M, et al. Surgical outcomes of spinal cord and cauda equina ependymoma: Postoperative motor status and recurrence for each WHO grade in a multicenter study. J Orthop Sci. 2018;23:614–21.
Bonfield CM, Amin D, Hamilton RL, Gerszten PC. Extramedullary ependymoma near the conus medullaris with lumbar nerve root attachment: case report. Neurosurgery. 2011;68:E831–4.
Pulitzer DR, Martin PC, Collins PC, Ralph DR. Subcutaneous sacrococcygeal (“myxopapillary”) ependymal rests. Am J Surg Pathol. 1988;12:672–7.
Acknowledgements
We thank for Dr. Kota Kojima and Dr. Yuki Miwa for their critical advice. We also thank for Ms Makiko Miyazaki, Ms Yukari Yamanishi, and Ms Kaoru Yasumuro for their assistance.
Author information
Authors and Affiliations
Contributions
Writing – original draft: SA and OT. Writing – review and editing: NN, SN, SS, EO, MY, and KW. Data curation – SA, OT, MN, and MM. Pathological analyses – RI. OT was responsible for all working related to this submission as corresponding author. Also, all authors approved the final version manuscript and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ando, S., Tsuji, O., Nagoshi, N. et al. Grade III intradural extramedullary anaplastic ependymoma managed with near-complete resection and adjuvant radiotherapy: a case report. Spinal Cord Ser Cases 7, 1 (2021). https://doi.org/10.1038/s41394-020-00367-1
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41394-020-00367-1