Abstract
Introduction
Postural hypotension (PH) is common in patients with spinal cord injury (SCI), especially those with tetraplegia. To effectively treat PH, identifying and eliminating treatable predisposing factors of PH are prerequisites before applying any interventions.
Case presentation
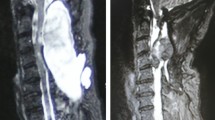
We report a patient with post-acute cervical SCI who suffered from intractable PH resulting from pseudomeningocele causing unfavorable rehabilitation outcomes. A previously healthy 34-year-old man with complete C6 SCI resulting from C6-C7 fracture dislocation developed PH in the first week of the rehabilitation program. No specific predisposing factors including anemia, hyponatremia, and dehydration were identified. Non-pharmacological interventions and pharmacological treatment were administered to the patient without satisfactory result, causing a delay in rehabilitation progression. In the fourth week of rehabilitation program, a mass at the surgical site was detected. A cervical MRI revealed a large fluid collection at the posterior aspect of cervical spines with a size of 7.9 × 6.8 × 5.0 cm. A diagnosis of pseudomeningocele was made and surgical site debridement with closing dura by grafting was immediately conducted. One day after surgery, PH disappeared, and the patient could progress in his rehabilitation program and achieve his short-term goal within three weeks.
Conclusion
Pseudomeningocele could be one of the precipitating factors of PH in patients with tetraplegia. Healthcare providers should consider investigating pseudomeningocele in patients who have intractable and unexplainable PH.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Popa C, Popa F, Grigorean VT, Onose G, Sandu AM, Popescu M, et al. Vascular dysfunctions following spinal cord injury. J Med Life. 2010;3:275–85.
Claydon VE, Steeves JD, Krassioukov A. Orthostatic hypotension following spinal cord injury: understanding clinical pathophysiology. Spinal Cord. 2006;44:341–51.
Krassioukov A, Wecht JM, Teasell RW, Eng JJ. Orthostatic hypotension following spinal cord injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, et al., editors. Spinal Cord Injury Rehabilitation Evidence. (2014). Version 5.0. Vancouver: p 1–26.
Ong ET, Yeo LK, Kaliya-Perumal AK, Oh JY. Orthostatic hypotension following cervical spine surgery: prevalence and risk factors. Glob Spine J. 2020;10:578–82.
Höfler M. The Bradford Hill considerations on causality: a counterfactual perspective. Emerg Themes Epidemiol. 2005;2:11.
Houtman S, Colier WN, Oeseburg B, Hopman MT. Systemic circulation and cerebral oxygenation during head-up tilt in spinal cord injured individuals. Spinal Cord. 2000;38:158–63.
Krassioukov AV, Weaver LC. Morphological changes in sympathetic preganglionic neurons after spinal cord injury in rats. Neuroscience 1996;70:211–25.
Frisbie JH, Steele DJ. Postural hypotension and abnormalities of salt and water metabolism in myelopathy patients. Spinal Cord. 1997;35:303–7.
Claydon VE, Krassioukov AV. Orthostatic hypotension and autonomic pathways after spinal cord injury. J Neurotrauma. 2006;23:1713–25.
Hopman MT, Groothuis JT, Flendrie M, Gerrits KH, Houtman S. Increased vascular resistance in paralyzed legs after spinal cord injury is reversible by training. J Appl Physiol. 2002;93:1966–72.
Faghri PD, Yount J. Electrically induced and voluntary activation of physiologic muscle pump: a comparison between spinal cord-injured and able-bodied individuals. Clin Rehabil. 2002;16:878–85.
Wecht JM, De Meersman RE, Weir JP, Spungen AM, Bauman WA. Cardiac autonomic responses to progressive head-up tilt in individuals with paraplegia. Clin Auton Res. 2003;13:433–8.
Mathias CJ. Autonomic diseases: management. J Neurol Neurosurg Psychiatry. 2003;74:iii42–7.
Raudenbush BL, Molinari A, Molinari RW. Large Compressive Pseudomeningocele Causing Early Major Neurologic Deficit After Spinal Surgery. Glob Spine J. 2017;7:206–12.
Blank RS, Waldrop CS, Balestrieri PJ. Pseudomeningocele: an unusual cause of intraoperative tracheal compression and expiratory obstruction. Anesth Analg. 2008;107:226–8.
Weng YJ, Cheng CC, Li YY, Huang TJ, Hsu RW. Management of giant pseudomeningoceles after spinal surgery. BMC Musculoskelet Disord. 2010;11:53.
Corona-Cedillo R, Saavedra-Navarrete MT, Espinoza-Garcia JJ, Mendoza-Aguilar AN, Ternovoy SK, Roldan-Valadez E. Imaging Assessment of the Postoperative Spine: An Updated Pictorial Review of Selected Complications. Biomed Res Int. 2021;18:9940001.
Solomon P, Sekharappa V, Krishnan V, David KS. Spontaneous resolution of postoperative lumbar pseudomeningoceles: A report of four cases. Indian J Orthop. 2013;47:417–21.
Gandhi J, DiMatteo A, Joshi G, Smith NL, Khan SA. Cerebrospinal fluid leaks secondary to dural tears: a review of etiology, clinical evaluation, and management. Int J Neurosci. 2021;131:689–95.
Ryken TC, Hadley MN, Walters BC, Aarabi B, Dhall SS, Gelb DE, et al. Radiographic assessment. Neurosurgery. 2013;72:54–72.
Aarabi B, Olexa J, Chryssikos T, Galvagno SM, Hersh DS, Wessell A, et al. Extent of spinal cord decompression in motor complete (American Spinal Injury Association Impairment Scale grades A and B) traumatic spinal cord injury patients: post-operative magnetic resonance imaging analysis of standard operative approaches. J Neurotrauma. 2019;36:862–76.
Acknowledgements
A part of this study was presented in the International Spinal Cord Society (ISCoS) 59th Annual Scientific Meeting (ISCoS 2020: VIRTUAL).
Author information
Authors and Affiliations
Contributions
BR and SP designed the research question, collected and analyzed the data, and wrote and revised the final version of the manuscripts.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
We certify that in our institute, a single, deidentification case report is waived from ethical approval.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rajchagool, B., Pattanakuhar, S. Intractable postural hypotension resulting from cervical pseudomeningocele after a posterior cervical spinal surgery: a case report. Spinal Cord Ser Cases 9, 14 (2023). https://doi.org/10.1038/s41394-023-00572-8
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41394-023-00572-8