Abstract
Introduction
Cement extravasation (CE) during vertebroplasty or kyphoplasty for vertebral compression fracture (VCF) is not uncommon, though neurological deficits occur rarely and when paraparesis occurs severe cord compression has been described. We report a case of progressive paraparesis in the setting of non-compressive extradural CE during kyphoplasty with evidence for spinal artery syndrome and neurological recovery after treatment.
Case presentation
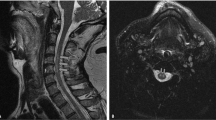
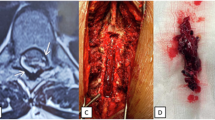
A 77-year-old female with T12 VCF failed conservative treatment and underwent kyphoplasty. In the recovery room, the patient was noted to have bilateral leg weakness, left worse than right, and had urgent CT scan that showed right paracentral CE without cord compression or arterial cement embolization. The patient was transferred to a tertiary hospital and had MRI of the spine that confirmed extradural CE and no cord compression. Because the patient had progression of lower extremity deficits despite medical management, she underwent surgical decompression, cement excision, and spinal fusion with instrumentation. Post op MRI showed T2 hyperintensities in the spinal cord consistent with spinal artery syndrome. One month post op, she had almost complete recovery of her neurological function.
Discussion
Spinal artery syndrome may be considered in patients with neurological deficit s/p kyphoplasty even if the extravasated cement does not compress the spinal cord and even if the deficits are worse contralateral to the cement extravasation. If spinal artery syndrome is present and medical management does not improve the deficits, surgery may be indicated even if there is no cord compression.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
All data from the above case report that was generated can be found within the article. Please contact the corresponding author with questions regarding any of the data included and/or details of the reported case.
References
Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557–68. https://doi.org/10.1056/NEJMoa0900429
Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569–79. https://doi.org/10.1056/NEJMoa0900563
Laredo JD, Hamze B. Complications of percutaneous vertebroplasty and their prevention. Skelet Radio. 2004;33:493–505. https://doi.org/10.1007/s00256-004-0776-8
Wardlaw D, Cummings SR, Van Meirhaeghe J, Bastian L, Tillman JB, Ranstam J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet. 2009;373:1016–24. https://doi.org/10.1016/S0140-6736(09)60010-6
Anderson PA, Froyshteter AB, Tontz WL Jr. Meta-analysis of vertebral augmentation compared with conservative treatment for osteoporotic spinal fractures. J Bone Min Res. 2013;28:372–82. https://doi.org/10.1002/jbmr.1762
Yeom JS, Kim WJ, Choy WS, Lee CK, Chang BS, Kang JW. Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. J Bone Jt Surg Br. 2003;85:83–9. https://doi.org/10.1302/0301-620x.85b1.13026
Sidhu GS, Kepler CK, Savage KE, Eachus B, Albert TJ, Vaccaro AR. Neurological deficit due to cement extravasation following a vertebral augmentation procedure. J Neurosurg Spine. 2013;19:61–70. https://doi.org/10.3171/2013.4.SPINE12978
Wilkes RA, Mackinnon JG, Thomas WG. Neurological deterioration after cement injection into a vertebral body. J Bone Jt Surg Br. 1994;76:155.
Lai PL, Tai CL, Chen LH, Nien NY. Cement leakage causes potential thermal injury in vertebroplasty. BMC Musculoskelet Disord. 2011;12:116. https://doi.org/10.1186/1471-2474-12-116
Tsai YD, Liliang PC, Chen HJ, Lu K, Liang CL, Wang KW. Anterior spinal artery syndrome following vertebroplasty: a case report. Spine. 2010;35:E134–6. https://doi.org/10.1097/BRS.0b013e3181b52221
Yazbeck PG, Al Rouhban RB, Slaba SG, Kreichati GE, Kharrat KE. Anterior spinal artery syndrome after percutaneous vertebroplasty. Spine J. 2011;11:e5–8. https://doi.org/10.1016/j.spinee.2011.06.020
Zou P, Gong HL, Wei JM, Wei DM, Qian LX, Liu P, et al. Spinal epidural hematoma after percutaneous kyphoplasty: case report and literature review. J Pain Res. 2020;13:2799–804. https://doi.org/10.2147/JPR.S280650
Bredow J, Oppermann J, Keller K, Beyer F, Boese CK, Zarghooni K, et al. Anterior spinal artery syndrome: reversible paraplegia after minimally invasive spine surgery. Case Rep Orthop. 2014;2014:205732. https://doi.org/10.1155/2014/205732
Premat K, Vande Perre S, Cormier É, Shotar E, Degos V, Morardet L, et al. Vertebral augmentation with the SpineJack® in chronic vertebral compression fractures with major kyphosis. Eur Radio. 2018;28:4985–91.
Noriega DC, Rodrίguez-Monsalve F, Ramajo R, Sánchez-Lite I, Toribio B, Ardura F. Long-term safety and clinical performance of kyphoplasty and SpineJack® procedures in the treatment of osteoporotic vertebral compression fractures: a pilot, monocentric, investigator-initiated study. Osteoporos Int. 2019;30:637–45. https://doi.org/10.1007/s00198-018-4773-5
Loher TJ, Bassetti CL, Lövblad KO, Stepper FP, Sturzenegger M, Kiefer C, et al. Diffusion-weighted MRI in acute spinal cord ischaemia. Neuroradiology. 2003;45:557–61. https://doi.org/10.1007/s00234-003-1023-z
Catapano JS, John Hawryluk GW, Whetstone W, Saigal R, Ferguson A, Talbott J, et al. Higher mean arterial pressure values correlate with neurologic improvement in patients with initially complete spinal cord injuries. World Neurosurg. 2016;96:72–9. https://doi.org/10.1016/j.wneu.2016.08.053
Rahman M, Rahman S, Siddik AB, Hossain MD, Musa J, Hamjah R, et al. A review on the pathophysiology and management of anterior spinal artery syndrome. J Spine Res Surg. 2020;2:085–96.
Guest JD, Griesdale DE, Marotta T. Thoracic disc herniation presenting with transient anterior spinal artery syndrome. A case report. Inter Neuroradiol. 2000;6:327–31.
Reynolds JM, Belvadi YS, Kane AG, Poulopoulos M. Thoracic disc herniation leads to anterior spinal artery syndrome demonstrated by diffusion-weighted magnetic resonance imaging (DWI): a case report and literature review. Spine J. 2014;14:e17–22. https://doi.org/10.1016/j.spinee.2013.10.050
Aalbers MW, Groen RJM, Appelman APA, Heersema TDJ, Wokke BHA, Oterdoom DLM. Spinal cord ischemia related to disc herniation: case report and a review of the literature. Int Med Case Rep J. 2021;14:429–33. https://doi.org/10.2147/IMCRJ.S316797
Santillan A, Goldberg JL, Carnevale JA, Kirnaz S, Hartl R, Knopman J. Anterior spinal artery syndrome caused by thoracic disc herniation. J Clin Neurosci. 2020;77:211–2. https://doi.org/10.1016/j.jocn.2020.05.040
Kesornsak W, Wasinpongwanich K, Kuansongtham V. Posterior epidural sequestrated disc presenting with contralateral radiculopathy: a very rare case. Spinal Cord Ser Cases. 2021;7:98. https://doi.org/10.1038/s41394-021-00460-z
Ruschel LG, Agnoletto GJ, Aragão A, Duarte JS, de Oliveira MF, Teles AR. Lumbar disc herniation with contralateral radiculopathy: a systematic review on pathophysiology and surgical strategies. Neurosurg Rev. 2021;44:1071–81. https://doi.org/10.1007/s10143-020-01294-3
Yeung JT, Johnson JI, Karim AS. Cervical disc herniation presenting with neck pain and contralateral symptoms: a case report. J Med Case Rep. 2012;6:166. https://doi.org/10.1186/1752-1947-6-166
Momomura R, Shimamura Y, Kaneko K. Postoperative clinical outcomes of balloon kyphoplasty treatment: would adherence to indications and contraindications prevent complications? Asian Spine J. 2020;14:198–203. https://doi.org/10.31616/asj.2019.0010
Wong W, Mathis JM. Vertebroplasty and kyphoplasty: techniques for avoiding complications and pitfalls. Neurosurg Focus. 2005;18:e2. https://doi.org/10.3171/foc.2005.18.3.3
Acknowledgements
The authors would like to thank the patient and her family for generously allowing us to present this case.
Author information
Authors and Affiliations
Contributions
Primary manuscript drafting was carried out by BMS and BCG. Manuscript editing as well as concept review/generation was a group task split equally among all authors. Direct care of the patient involved was provided by CZ and senior author, SK.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Consent for publication of this patient case was obtained from the index patient’s husband. Unfortunately, the patient had deceased prior to the drafting of the manuscript from an unrelated cause.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Striano, B.M., Goh, B.C., Ziino, C. et al. Spinal artery syndrome following kyphoplasty in the setting of a non-compressive extradural cement extravasation: a case report. Spinal Cord Ser Cases 9, 18 (2023). https://doi.org/10.1038/s41394-023-00574-6
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41394-023-00574-6