Abstract
Depression is a prevalent mental health condition that frequently remains undiagnosed, highlighting the need for objective and scalable screening tools. Heart rate variability (HRV) has emerged as a potential physiological marker of depression, and facial video-based HRV measurement offers a novel, contactless approach that could facilitate widespread, non-invasive depression screening. We analyzed data from 1453 individuals who completed facial video recordings and the Patient Health Questionnaire-9 (PHQ-9). A stacking ensemble classifier was developed using HRV features and basic demographic information to classify individuals with depressive symptoms. The ensemble incorporated four base learners (logistic regression, gradient boosting, XGBoost, and SVM) with an SVM meta-learner. Model performance was evaluated using 5-fold cross-validation. The stacking model achieved its best discrimination of AUROC 0.64 (AUPRC 0.45 and MCC 0.21). Incorporating demographic features alongside HRV improved performance over HRV alone. Feature importance analysis revealed that smoking status, sex, and medical comorbidities were the strongest contributors to the predictions. Facial video-derived HRV, combined with simple demographic factors, can moderately distinguish individuals with depressive symptoms in a contactless manner. Although predictive performance was modest, this non-invasive approach shows promise for accessible, large-scale depression screening.
Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018:1789-858.
Radez J, Reardon T, Creswell C, Orchard F, Waite P Adolescents’ perceived barriers and facilitators to seeking and accessing professional help for anxiety and depressive disorders: a qualitative interview study. Eur Child Adolesc Psychiatry. 2021:1-17.
Aldarwish MM, Ahmad HF Predicting depression levels using social media posts. 2017 IEEE 13th international Symposium on Autonomous decentralized system (ISADS). 2017;277-80.
Byun S, Kim AY, Jang EH, Kim S, Choi KW, Yu HY, et al. Detection of major depressive disorder from linear and nonlinear heart rate variability features during mental task protocol. Comput Biol Med. 2019;112:103381.
Coutts LV, Plans D, Brown AW, Collomosse J. Deep learning with wearable based heart rate variability for prediction of mental and general health. J Biomed Inf. 2020;112:103610.
Liu Z, Hu B, Yan L, Wang T, Liu F, Li X, et al. Detection of depression in speech. 2015 international conference on affective computing and intelligent interaction (ACII). 2015;743-7.
Zhang D, Qu Y, Zhai S, Li T, Xie Y, Tao S, et al. Association between healthy sleep patterns and depressive trajectories among college students: a prospective cohort study. BMC Psychiatry. 2023;23:182.
Zhu J, Wang Z, Gong T, Zeng S, Li X, Hu B, et al. An improved classification model for depression detection using EEG and eye tracking data. IEEE Trans Nanobioscience. 2020;19:527–37.
Hartmann R, Schmidt FM, Sander C, Hegerl U. Heart rate variability as indicator of clinical state in depression. Front Psychiatry. 2019;9:735.
Cygankiewicz, I & Zareba, W in Autonomic Nervous System: Chapter 31. Heart rate variability (Elsevier Inc., 2013).
Chalmers JA, Quintana DS, Abbott MJ-A, Kemp AH. Anxiety disorders are associated with reduced heart rate variability: a meta-analysis. Front Psychiatry. 2014;5:80.
Kemp AH, Quintana DS, Gray MA, Felmingham KL, Brown K, Gatt JM. Impact of depression and antidepressant treatment on heart rate variability: a review and meta-analysis. Biol Psychiatry. 2010;67:1067–74.
Koch C, Wilhelm M, Salzmann S, Rief W, Euteneuer F. A meta-analysis of heart rate variability in major depression. Psychol Med. 2019;49:1948–57.
Wu Q, Miao X, Cao Y, Chi A, Xiao T. Heart rate variability status at rest in adult depressed patients: a systematic review and meta-analysis. Front Public Health. 2023;11:1243213.
Geng D, An Q, Fu Z, Wang C, An H. Identification of major depression patients using machine learning models based on heart rate variability during sleep stages for pre-hospital screening. Comput Biol Med. 2023;162:107060.
Kim EY, Lee MY, Kim SH, Ha K, Kim KP, Ahn YM. Diagnosis of major depressive disorder by combining multimodal information from heart rate dynamics and serum proteomics using machine-learning algorithm. Prog Neuropsychopharmacol Biol Psychiatry. 2017;76:65–71.
Sun G, Shinba T, Kirimoto T, Matsui T. An objective screening method for major depressive disorder using logistic regression analysis of heart rate variability data obtained in a mental task paradigm. Front Psychiatry. 2016;7:180.
Zhang Z-X, Tian X-W, Lim J New algorithm for the depression diagnosis using HRV: A neuro-fuzzy approach. International Symposium on Bioelectronics and Bioinformatics. 2011;283-6.
Hornstein S, Seiler M, Hoffman V, Nelson B, Aschbacher K, Ritter K, et al. Association of depressive symptoms with resting heart rate variability recorded from a wearable device under naturalistic conditions: a machine learning study. Preprint at https://osf.io/preprints/psyarxiv/9z3pr_v1 (2022).
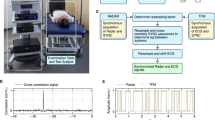
Odinaev I, Wong KL, Chin JW, Goyal R, Chan TT, So RHY. Robust Heart Rate Variability Measurement from Facial Videos. Bioengineering. 2023;10:851.
Unursaikhan B, Tanaka N, Sun G, Watanabe S, Yoshii M, Funahashi K, et al. Development of a novel web camera-based contact-free major depressive disorder screening system using autonomic nervous responses induced by a mental task and its clinical application. Front Physiol. 2021;12:642986.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13.
William G. (eds) ECDEU assessment manual for psychopharmacology (US Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs; 1976).
de Haan G, Jeanne V. Robust pulse rate from chrominance-based rPPG. IEEE Trans Biomed Eng. 2013;60:2878–86.
Pham T, Lau ZJ, Chen SHA, Makowski D. Heart rate variability in psychology: a review of HRV indices and an analysis tutorial. Sensors. 2021;21:3998.
Soleymani M, Lichtenauer J, Pun T, Pantic M. A multimodal database for affect recognition and implicit tagging. IEEE Trans Affect Comput. 2012;3:42–55.
Akiba T, Sano S, Yanase T, Ohta T, Koyama M. Optuna: a next-generation hyperparameter optimization framework. Proceeding of the 25th ACM SIGKDD international conference on knowledge discovery & data mining. 2019;2623-31.
Watanabe S. Tree-Structured Parzen Estimator: Understanding Its Algorithm Components and Their Roles for Better Empirical Performance. arxiv [Preprint]. Available from: https://arxiv.org/abs/2304.11127 (2023).
Lundberg SM, Lee S-I. A unified approach to interpreting model predictions. Proceedings of the 31st International Conference on Neural Information Processing Systems. 2017;4768–77.
Hu Z, Cui E, Chen B, Zhang M. Association between cigarette smoking and the risk of major psychiatric disorders: a systematic review and meta-analysis in depression, schizophrenia, and bipolar disorder. Front Med. 2025;12:1529191.
Albert PR. Why is depression more prevalent in women?. J Psychiatry Neurosci. 2015;40:219–21.
Benton T, Staab J, Evans DL. Medical co-morbidity in depressive disorders. Ann Clin Psychiatry. 2007;19:289–303.
Eriksson A, Kimmel MC, Furmark T, Wikman A, Grueschow M, Skalkidou A, et al. Investigating heart rate variability measures during pregnancy as predictors of postpartum depression and anxiety: an exploratory study. Transl Psychiatry. 2024;14:203.
Kwong AS, López-López JA, Hammerton G, Manley D, Timpson NJ, Leckie G, et al. Genetic and environmental risk factors associated with trajectories of depression symptoms from adolescence to young adulthood. JAMA Netw Open. 2019;2:e196587–e87.
Saveanu RV, Nemeroff CB. Etiology of depression: genetic and environmental factors. Psychiatr Clin North Am. 2012;35:51–71.
Burchert S, Kerber A, Zimmermann J, Knaevelsrud C. Screening accuracy of a 14-day smartphone ambulatory assessment of depression symptoms and mood dynamics in a general population sample: Comparison with the PHQ-9 depression screening. PLoS One. 2021;16:e0244955.
Wei Y, Qin S, Liu F, Liu R, Zhou Y, Chen Y, et al. Acoustic-based machine learning approaches for depression detection in Chinese university students. Front Public Health. 2025;13:1561332.
Bai Y, Liu Y, Zhang Y, Tolba A. Smartphone sensor-based depression detection in campus environments: a proof-of-concept study with small-sample behavioral analysis. Front Psychiatry. 2025;16:1468334.
Sato S, Hiratsuka T, Hasegawa K, Watanabe K, Obara Y, Kariya N, et al. Screening for major depressive disorder using a wearable ultra-short-term hrv monitor and signal quality indices. Sensors. 2023;23:3867.
Wang Z, Zou Y, Liu J, Peng W, Li M, Zou Z. Heart rate variability in mental disorders: an umbrella review of meta-analyses. Transl Psychiatry. 2025;15:104.
Acknowledgements
The authors are grateful to the staff of the CNUH and CNUHH psychiatry research teams for assisting in the collection of patient data, and to Dr. Kim Jae Chang and Dr. Kim Sun Hee for providing the space for data analysis and data collection.
Funding
This research was supported by the Bio&Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (No. RS-2024-00440371) to Jae-Min Kim and the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (NRF-2020M3A9G3080281) to Yoonjoo Choi.
Author information
Authors and Affiliations
Contributions
MJ: designed the study, contributed to the conceptualization, and drafted and revised the manuscript. JWK: designed the study, contributed to the conceptualization, and drafted and revised the manuscript. KL: contributed to the conceptualization, performed the formal analysis, and drafted the manuscript. DK: contributed to the conceptualization and performed the formal analysis. SHP: curated the data and validated the findings. CHK: curated the data and performed the formal analysis. BTL: curated the data and validated the findings. SYK: curated the data and validated the findings. SWK: curated the data and validated the findings. JMK: contributed to the conceptualization, validated the findings, and reviewed and edited the manuscript. ISS: contributed to the conceptualization, validated the findings, and reviewed and edited the manuscript. YC: designed the study, contributed to the conceptualization, and drafted and revised the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Statement of ethics
All patients gave written informed consent to participate in the study and use their data. The study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2008 and approved by the Ethics Commission of the Chonnam National University Hopital Institutional Review Board (CNUH-2021-243, CNUH-2022-216) and the Chonnam National University Hwasun Hospital Institutional Review Board (CNUHH-2021-117, and CNUHH-2022-126) as it uses de-identified data.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jhon, M., Kim, JW., Lee, K. et al. Contactless depression screening via facial video-derived heart rate variability. Transl Psychiatry (2026). https://doi.org/10.1038/s41398-026-03831-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-026-03831-y