Abstract
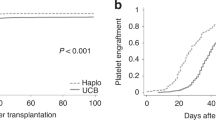
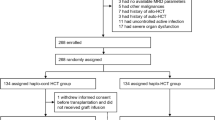
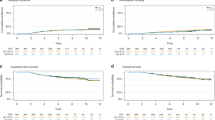
Hematopoietic stem cell transplantation (HCT) is the standard consolidation therapy for children with high-risk or relapsed acute myeloid leukemia (AML). In the absence of an human leukocyte antigen (HLA)-matched donor, both unrelated cord blood transplantation (UCBT) and haploidentical HCT with post-transplant cyclophosphamide (haplo-PTCy) serve as viable alternatives. This study analyzed outcomes of 254 pediatric AML patients (CR1/CR2) who underwent either single-unit UCBT (N = 127) without serotherapy or haplo-PTCy (N = 127) between 2011 and 2021. Propensity score weighting was applied to minimize baseline differences. With a median follow-up of 2.9 years, no significant differences were observed in overall survival, leukemia-free survival, relapse incidence, non-relapse mortality (NRM), or graft-versus-host disease (GVHD)-free relapse-free survival. However, UCBT recipients had a lower risk of chronic GVHD (7.1% vs. 19.8%; P = 0.019). These findings confirm comparable survival outcomes between UCBT and Haplo-PTCy. Given the higher risk of cGVHD in haplo-PTCy, further research is needed to refine GVHD prevention strategies while maintaining relapse-free survival. Both approaches remain safe and readily available alternatives for pediatric AML patients lacking matched donors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data cannot be shared unless a specific request is sent to the EBMT.
References
Puumala SE, Ross JA, Aplenc R, Spector LG. Epidemiology of childhood acute myeloid leukemia. Pediatr Blood Cancer. 2013;60:728–33.
Egan G, Tasian SK. Relapsed pediatric acute myeloid leukaemia: state-of-the-art in 2023. Haematologica. 2023;108:2275–88.
Wynn R, Nataraj R, Nadaf R, Poulton K, Logan A Strategies for success with umbilical cord haematopoietic stem cell transplantation in children with malignant and non-malignant disease indications. Front Cell Dev Biol. 2022; https://doi.org/10.3389/fcell.2022.836594.
Algeri M, Merli P, Locatelli F, Pagliara D. The role of allogeneic hematopoietic stem cell transplantation in pediatric leukemia. J Clin Med. 2021; https://doi.org/10.3390/jcm10173790.
O’Donnell PV, Luznik L, Jones RJ, Vogelsang GB, Leffell MS, Phelps M, et al. Nonmyeloablative bone marrow transplantation from partially HLA-mismatched related donors using posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2002;8:377–86.
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14:641–50.
Barkhordar M, Kasaeian A, Janbabai G, Mousavi SA, Fumani HK, Tavakoli S, et al. Outcomes of haploidentical peripheral stem cell transplantation with combination of post-transplant cyclophosphamide (PTCy) and anti-thymocyte globulin (ATG) compared to unrelated donor transplantation in acute myeloid leukemia: a retrospective 10-year experience. Leuk Res. 2022; https://doi.org/10.1016/j.leukres.2022.106918.
Bazarbachi A, Labopin M, Raiola AM, Blaise D, Arcese W, Santarone S, et al. Posttransplant cyclophosphamide versus anti-thymocyte globulin versus combination for graft-versus-host disease prevention in haploidentical transplantation for adult acute myeloid leukemia: a report from the European Society for Blood and Marrow Transplantation Acute Leukemia Working Party. Cancer. 2024;130:3123–36.
Passweg JR, Baldomero H, Chabannon C, Basak GW, de la Cámara R, Corbacioglu S, et al. Hematopoietic cell transplantation and cellular therapy survey of the EBMT: monitoring of activities and trends over 30 years. Bone Marrow Transplant. 2021;56:1651–64.
Giannotti F, Labopin M, Shouval R, Sanz J, Arcese W, Angelucci E, et al. Haploidentical transplantation is associated with better overall survival when compared to single cord blood transplantation: an EBMT-Eurocord study of acute leukemia patients conditioned with thiotepa, busulfan, and fludarabine. J Hematol Oncol. 2018;11:110.
Ruggeri A, Galimard JE, Labopin M, Rafii H, Blaise D, Ciceri F, et al. Comparison of outcomes after unrelated double-unit cord blood and haploidentical peripheral blood stem cell transplantation in adults with acute myelogenous leukemia: a study on behalf of Eurocord and the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Transplant Cell Ther. 2022;28:710.e1–710.e10.
Berger M, Lanino E, Cesaro S, Zecca M, Vassallo E, Faraci M, et al. Feasibility and outcome of haploidentical hematopoietic stem cell transplantation with post-transplant high-dose cyclophosphamide for children and adolescents with hematologic malignancies: an AIEOP-GITMO retrospective multicenter study. Biol Blood Marrow Transplant. 2016;22:902–9.
Symons HJ, Zahurak M, Cao Y, Chen A, Cooke K, Gamper C, et al. Myeloablative haploidentical BMT with posttransplant cyclophosphamide for hematologic malignancies in children and adults. Blood Adv. 2020;4:3913–25.
Saglio F, Berger M, Spadea M, Pessolano R, Carraro F, Barone M, et al. Haploidentical HSCT with post transplantation cyclophosphamide versus unrelated donor HSCT in pediatric patients affected by acute leukemia. Bone Marrow Transplant. 2021;56:586–95.
Ruggeri A, Galimard JE, Paina O, Fagioli F, Tbakhi A, Yesilipek A, et al. Outcomes of unmanipulated haploidentical transplantation using post-transplant cyclophosphamide (PT-Cy) in pediatric patients with acute lymphoblastic leukemia. Transplant Cell Ther. 2021; https://doi.org/10.1016/j.jtct.2021.01.016.
Srinivasan A, Raffa E, Wall DA, Schechter T, Ali M, Chopra Y, et al. Outcome of haploidentical peripheral blood allografts using post-transplantation cyclophosphamide compared to matched sibling and unrelated donor bone marrow allografts in pediatric patients with hematologic malignancies: a single-center analysis. Transplant Cell Ther. 2022; https://doi.org/10.1016/j.jtct.2021.01.016.
Hong KT, Park HJ, Kim BK, An HY, Choi JY, Kang HJ. Post-transplantation cyclophosphamide-based haploidentical versus matched unrelated donor peripheral blood hematopoietic stem cell transplantation using myeloablative targeted busulfan-based conditioning for pediatric acute leukemia. Transplant Cell Ther. 2022;28:195.e1–195.e7. https://doi.org/10.1016/j.jtct.2022.01.002.
Nishikawa T. Human leukocyte antigen–haploidentical haematopoietic stem cell transplantation using post-transplant cyclophosphamide for paediatric haematological malignancies. Cancers. 2024;16:600 https://doi.org/10.3390/cancers16030600.
Calvo C, Hautefeuille C, Vasseur L, Chevillon F, Nazon C, Bruno B, et al. Real-world outcomes of haplo-HSCT with post-transplant cyclophosphamide in pediatric hematologic malignancies: a study on behalf of SFGM-TC and SFCE. Bone Marrow Transplant. 2025; https://doi.org/10.1038/s41409-025-02584-4.
Ruggeri A, Santoro N, Galimard JE, Kalwak K, Algeri M, Zubarovskaya L, et al. Matched unrelated donor transplantation versus haploidentical transplantation with post-transplant cyclophosphamide in children with acute myeloid leukemia: a PDWP-EBMT study. Haematologica. 2024;109:2122–30.
Sisinni L, Monserrate GXA, Hurtado JMP, Panesso M, Molina B, Fuentes C, et al. Haploidentical versus cord blood transplantation in pediatric AML: a retrospective outcome analysis on behalf of the Pediatric Subcommittee of GETH (Grupo Español de Trasplante Hematopoyético). Transplant Cell Ther. 2024;30:1015.e1–1015.e13. https://doi.org/10.1016/j.jtct.2024.07.013.
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–47.
Ruggeri A, Labopin M, Ciceri F, Mohty M, Nagler A. Definition of GvHD-free, relapse-free survival for registry-based studies: an ALWP-EBMT analysis on patients with AML in remission. Bone Marrow Transplant. 2016;51:610–1.
Martino R, Romero P, Subirá M, Bellido M, Altés A, Sureda A, et al. Comparison of the classic Glucksberg criteria and the IBMTR Severity Index for grading acute graft-versus-host disease following HLA-identical sibling stem cell transplantation. Bone Marrow Transplant. 1999;24:283–7.
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: I. The 2014 Diagnosis and Staging Working Group Report. Biol Blood Marrow Transplant. 2015;21:389–401.e1. https://doi.org/10.1016/j.bbmt.2014.12.001.
Peters C, Matthes-Martin S, Poetschger U, Schrappe M, Schrauder A, von Stackelberg A, et al. Stem-cell transplantation in children with acute lymphoblastic leukemia: a prospective international multicenter trial comparing sibling donors with matched unrelated donors—the ALL-SCT-BFM-2003 trial. J Clin Oncol. 2015;33:1265–74.
Saarinen-Pihkala UM, Gustafsson G, Ringdén O, Heilmann C, Glomstein A, Lönnerholm G, et al. No disadvantage in outcome of using matched unrelated donors as compared with matched sibling donors for bone marrow transplantation in children with acute lymphoblastic leukemia in second remission. J Clin Oncol. 2001;19:3406–14.
Doherty EE, Redell M, Sasa G, Yassine K, John TD, Craddock J, et al. Outcomes after allogeneic hematopoietic stem cell transplantation for pediatric acute myeloid leukemia in the contemporary era. Blood. 2019; https://doi.org/10.1182/blood-2019-131131.
Dalle JH, Balduzzi A, Bader P, Lankester A, Yaniv I, Wachowiak J, et al. Allogeneic stem cell transplantation from HLA-mismatched donors for pediatric patients with acute lymphoblastic leukemia treated according to the 2003 BFM and 2007 International BFM studies: impact of disease risk on outcomes. Biol Blood Marrow Transpl. 2018;24:1848–55.
Bertaina A, Zecca M, Buldini B, Sacchi N, Algeri M, Saglio F, et al. Unrelated donor vs HLA-haploidentical α/β T-cell- and B-cell-depleted HSCT in children with acute leukemia. Blood. 2018;132:2594–607.
Ballen KK, Lazarus H. Cord blood transplant for acute myeloid leukaemia. Br J Haematol. 2016;173:25–36.
Horgan C, Mullanfiroze K, Rauthan A, Patrick K, Butt NA, Mirci-Danicar O, et al. T-cell replete cord transplants give superior outcomes in high-risk and relapsed/refractory pediatric myeloid malignancy. Blood Adv. 2023;7:2155–65.
Martinez C, Aguayo-Hiraldo P, Chaimowitz N, Forbes L, Rider N, Nicholas S, et al. Cord blood transplantation for nonmalignant disorders: early functional immunity and high survival. Blood Adv. 2023;7:1823–30.
Merli P, Algeri M, Galaverna F, Bertaina V, Lucarelli B, Boccieri E, et al. TCRαβ/CD19 cell-depleted HLA-haploidentical transplantation to treat pediatric acute leukemia: updated final analysis. Blood. 2024;143:279–89.
Fierro-Pineda JC, Tsai HL, Blackford A, Cluster A, Caywood E, Dalal J, et al. Prospective PTCTC trial of myeloablative haplo-BMT with posttransplant cyclophosphamide for pediatric acute leukemias. Blood Adv. 2023;7:5639–48.
Bertaina A, Pitisci A, Sinibaldi M, Algeri M. T cell-depleted and T cell-replete HLA-haploidentical stem cell transplantation for non-malignant disorders. Curr Hematol Malig Rep. 2017;12:68–78.
Ramírez P, Brunstein CG, Miller B, Defor T, Weisdorf D. Delayed platelet recovery after allogeneic transplantation: a predictor of increased treatment-related mortality and poorer survival. Bone Marrow Transplant. 2011;46:981–6.
Shi PA, Luchsinger LL, Greally JM, Delaney CS. Umbilical cord blood: an undervalued and underutilized resource in allogeneic hematopoietic stem cell transplant and novel cell therapy applications. Curr Opin Hematol. 2022;29:317–26.
Christakopoulos GE, DeFor TE, Hage S, Wagner JE, Linden MA, Brunstein C, et al. Phase I dose-finding, safety, and tolerability trial of romiplostim to improve platelet recovery after UCB transplantation. Transplant Cell Ther. 2021;27:497.e1–497.e6. https://doi.org/10.1016/j.jtct.2021.02.033.
Shpall EJ, Rezvani K. Cord blood expansion has arrived. Blood. 2021;138:1381–2.
Vairy S, Louis I, Vachon MF, Richer J, Teira P, Cellot S, et al. Intrabone infusion for allogeneic umbilical cord blood transplantation in children. Bone Marrow Transplant. 2021;56:1937–43.
Author information
Authors and Affiliations
Contributions
AR and KK designed the study. BEDM wrote the manuscript. MA and JEG performed the statistical analysis. GL critically reviewed the paper. AD, BV, LZ, OMD, CJ, ST, RW, SL, GM, AB, RMH, AS, AAA, FR, MF, MA, JHD, CC, VR, EG, KaK and SC provided cases for the study. All authors edited and approved the manuscript. Full acknowledgement list of participating Centers is available in the Supplementary material.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Di Majo, B.E., Abouqateb, M., Galimard, JE. et al. Single unrelated umbilical cord blood versus unmanipulated haploidentical HCT using PTCy in pediatric AML: a retrospective study on behalf of the EBMT PDWP and CTIWP. Bone Marrow Transplant 60, 1635–1641 (2025). https://doi.org/10.1038/s41409-025-02720-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-025-02720-0