Abstract
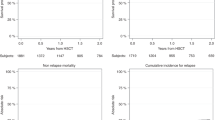
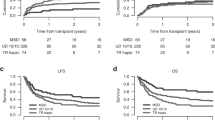
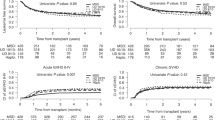
Primary refractory acute myeloid leukemia (prAML) is a poor prognosis disease, with allogeneic hematopoietic stem cell transplantation (allo-HSCT) being the only potentially curative option. We retrospectively evaluated outcomes in 1574 adult prAML patients who underwent allo-HSCT from matched sibling donors (MSD), 10/10 or 9/10 unrelated donors (UD), or haploidentical donors between 2015 and 2020. Median follow-up was 24, 30, 38, and 24 months for MSD, UD 10/10, UD 9/10, and haploidentical transplants, respectively. MSD recipients were younger (median age 53 vs. 58–59 years in other groups, p < 0.001), had better performance status, and proceeded to transplant more quickly (3.8 months vs. >4 months in other groups, p = 0.004). In multivariate analysis, haploidentical HSCT was associated with inferior leukemia-free survival (LFS) and overall survival (OS) compared to other donor types. Additional negative predictors included adverse cytogenetics and longer time from diagnosis to transplant. Conversely, reduced-intensity conditioning and good performance status of the patient were associated with improved LFS. Disease progression remained the leading cause of transplant failure, underscoring the urgent need for more effective early post-transplant strategies.
This is a preview of subscription content, access via your institution
Access options
Similar content being viewed by others
Data availability
The final analysis dataset will be available upon specific request to the Working Party chair.
References
Döhner H, Wei AH, Appelbaum FR, Craddock C, DiNardo CD, Dombret H, et al. Diagnosis and management of AML in adults: 2022 ELN recommendations from an International Expert Panel. Blood. 2022;140:1345–77.
Schlenk RF, Döhner H. Genomic applications in the clinic: use in treatment paradigm of acute myeloid leukemia. Hematol Am Soc Hematol Educ Program. 2013;2013:324–30.
Byrd J, Mrózek K, Dodge R, Carroll A, Edward C, Arthur D, et al. Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood. 2002;100:4325–36.
McMahon CM, Perl AE. Management of primary refractory acute myeloid leukemia in the era of targeted therapies. Christine Leuk Lymphoma. 2019;60:583–97.
Ferguson P, Craddock C. Allogeneic transplantation in primary refractory AML. Bone Marrow Transpl. 2017;52:950–1.
Ferguson P, Hills RK, Grech A, Betteridge S, Kjeldsen L, Dennis M, et al. An operational definition of primary refractory acute myeloid leukemia allowing early identification of patients who may benefit from allogeneic stem cell transplantation. Haematologica. 2016;101:1351–8.
Kantarjian H, Kadia T, DiNardo C, Daver N, Borthakur G, Jabbour E, et al. Acute myeloid leukemia: current progress and future directions. Blood Cancer J. 2021;11:41.
Jabbour E, Daver N, Champlin R, Mathisen M, Oran B, Ciurea S, et al. Allogeneic stem cell transplantation as initial salvage for patients with acute myeloid leukemia refractory to high-dose cytarabine-based induction chemotherapy. Am J Hematol. 2014;89:395–8.
Duval M, Klein JP, He W, Cahn JY, Cairo M, Camitta BM, et al. Hematopoietic stem-cell transplantation for acute leukemia in relapse or primary induction failure. J Clin Oncol. 2010;28:3730–8.
Begna KH, Kittur J, Gangat N, Alkhateeb H, Patnaik MS, Al-Kali A, et al. European LeukemiaNet-defined primary refractory acute myeloid leukemia: the value of allogeneic hematopoietic stem cell transplant and overall response. Blood Cancer J. 2022;12:1–8.
Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH, et al. Refinement of cytogenetic classification in acute myeloid leukemia: Determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010;116:354–65.
Schoemans HM, Lee SJ, Ferrara JL, Wolff D, Levine JE, Schultz KR, et al. EBMT−NIH−CIBMTR Task Force position statement on standardized terminology & guidance for graft-versus-host disease assessment. Bone Marrow Transpl. 2018;53:1401–15. https://doi.org/10.1038/s41409-018-0204-7.
Craddock C, Labopin M, Pillai S, Finke J, Bunjes D, Greinix H, et al. Factors predicting outcome after unrelated donor stem cell transplantation in primary refractory acute myeloid leukaemia. Leukemia. 2011;25:808–13.
Todisco E, Ciceri F, Boschini C, Giglio F, Bacigalupo A, Patriarca F, et al. Factors predicting outcome after allogeneic transplant in refractory acute myeloid leukemia: a retrospective analysis of Gruppo Italiano Trapianto di Midollo Osseo (GITMO). Bone Marrow Transpl. 2017;52:955–61.
Stelljes M, Middeke JM, Bug G, Wagner-Drouet EM, Müller LP, Schmid C, et al. Remission induction versus immediate allogeneic haematopoietic stem cell transplantation for patients with relapsed or poor responsive acute myeloid leukaemia (ASAP): a randomised, open-label, phase 3, non-inferiority trial. Lancet 2024;11:324–35.
Passweg JR, Baldomero H, Atlija M, Kleovoulou I, Witaszek A, Alexander T, et al. The 2023 EBMT report on hematopoietic cell transplantation and cellular therapies. Increased use of allogeneic HCT for myeloid malignancies and of CAR-T at the expense of autologous HCT. Bone Marrow Transplant. 2025;60:519–28.
Passweg JR, Baldomero H, Alexander T, Angelucci E, Averbuch D, Bazarbachi A, et al. Utilization of hematopoietic cell transplantation and cellular therapy technology in Europe and associated Countries. Using the 2022 activity survey data to correlate with economic and demographic factors. A report from the EBMT. Bone Marrow Transplant. 2024. Available from: https://doi.org/10.1038/s41409-024-02459-0
Brissot E, Labopin M, Stelljes M, Ehninger G, Schwerdtfeger R, Finke J, et al. Comparison of matched sibling donors versus unrelated donors in allogeneic stem cell transplantation for primary refractory acute myeloid leukemia: A study on behalf of the Acute Leukemia Working Party of the EBMT. J Hematol Oncol. 2017;10:1–10.
Battipaglia G, Boumendil A, Labopin M, Ciceri F, Tischer J, Stelljes M, et al. Unmanipulated haploidentical versus HLA-matched sibling allogeneic hematopoietic stem cell transplantation in relapsed/refractory acute myeloid leukemia: a retrospective study on behalf of the ALWP of the EBMT. Bone Marrow Transpl. 2019;54:1499–510. https://doi.org/10.1038/s41409-019-0459-7.
Baron F, Labopin M, Tischer J, Ciceri F, Raiola AM, Blaise D, et al. Comparison of HLA-mismatched unrelated donor transplantation with post-transplant cyclophosphamide versus HLA-haploidentical transplantation in patients with active acute myeloid leukemia. Bone Marrow Transpl. 2022;57:1657–63.
Brissot E, Labopin M, Ehninger G, Stelljes M, Brecht A, Ganser A, et al. Haploidentical versus unrelated allogeneic stem cell transplantation for relapsed/ refractory acute myeloid leukemia: a report on 1578 patients from the Acute leukemia working party of the EBMT. Haematologica. 2019;104:524–32.
Ciotti G, Marconi G, Martinelli G. Hypomethylating agent-based combination therapies to treat post-hematopoietic stem cell transplant relapse of acute myeloid leukemia. Front Oncol. 2022;11:1–9.
DeWolf S, Tallman MS. How I treat relapsed or refractory AML. Blood. 2020;136:1023–32.
Poiani M, Labopin M, Battipaglia G, Beelen DW, Tischer J, Finke J, et al. The impact of cytogenetic risk on the outcomes of allogeneic hematopoietic cell transplantation in patients with relapsed/refractory acute myeloid leukemia: On behalf of the acute leukemia working party (ALWP) of the European group for blood and marrow tr. Am J Hematol. 2021;96:40–50.
Nagler A, Labopin M, Dholaria B, Ciceri F, Fraccaroli A, Blaise D, et al. Impact of cytogenetic risk on outcomes of non-T cell depleted haploidentical hematopoietic cell transplantation in patients with relapsed or refractory acute myeloid leukemia. Transplant Cell Ther. 2022;28:773.e1–773.e8.
Gagelmann N, Kröger N. Dose intensity for conditioning in allogeneic hematopoietic cell transplantation: can we recommend “when and for whom” in 2021?. Haematologica. 2021;106:1794–804.
Nagler A, Savani BN, Labopin M, Polge E, Passweg J, Finke J, et al. Outcomes after use of two standard ablative regimens in patients with refractory acute myeloid leukaemia: a retrospective, multicentre, registry analysis. Lancet Haematol. 2015;2:e384–92.
Bonifazi F, Pavoni C, Peccatori J, Giglio F, Arpinati M, Busca A, et al. Myeloablative conditioning with thiotepa-busulfan-fludarabine does not improve the outcome of patients transplanted with active leukemia: final results of the GITMO prospective trial GANDALF-01. Bone Marrow Transpl. 2022;57:949–58.
Sawyer J, Elliott T, Orton L, Sowell H, Gatwood K, Shultes K. Prevention and management of acute toxicities from conditioning regimens during hematopoietic stem cell transplantation. Clin Hematol Int. 2024;6:1–10.
Rubio MT, Savani BN, Labopin M, Piemontese S, Polge E, Ciceri F, et al. Impact of conditioning intensity in T-replete haplo-identical stem cell transplantation for acute leukemia: a report from the acute leukemia working party of the EBMT. J Hematol Oncol [Internet]. 2016;9:1–12. https://doi.org/10.1186/s13045-016-0248-3.
Sweeney C, Vyas P. The graft-versus-leukemia effect in AML. Front Oncol. 2019;9:1–19.
Lee SJ, Vogelsang G, Flowers MED. Chronic graft-versus-host disease. Biol Blood Marrow Transpl. 2003;9:215–33.
Kolb HJ, Schmid C. The FLAMSA concept—past and future. Ann Hematol. 2020;99:1979–88.
Schmid C, Labopin M, Schaap N, Veelken H, Brecht A, Stadler M, et al. Long-term results and GvHD after prophylactic and preemptive donor lymphocyte infusion after allogeneic stem cell transplantation for acute leukemia. Bone Marrow Transpl. 2022;57:215–23.
Mohty M, Malard F, Blaise D, Milpied N, Socié G, Huynh A, et al. Sequential regimen of clofarabine, cytosine arabinoside and reduced-intensity conditioned transplantation for primar y refractor y acute myeloid Leukemia. Haematologica. 2017;102:184–91.
Duléry R, Ménard AL, Chantepie S, El-Cheikh J, François S, Delage J, et al. Sequential conditioning with thiotepa in T cell- replete hematopoietic stem cell transplantation for the treatment of refractory hematologic malignancies: comparison with matched related, Haplo-mismatched, and unrelated donors. Biol Blood Marrow Transpl. 2018;24:1013–21. https://doi.org/10.1016/j.bbmt.2018.01.005.
Heinicke T, Labopin M, Polge E, Stelljes M, Ganser A, Tischer J, et al. Evaluation of six different types of sequential conditioning regimens for allogeneic stem cell transplantation in relapsed/refractory acute myelogenous leukemia–a study of the Acute Leukemia Working Party of the EBMT. Leuk Lymphoma. 2021;62:399–409. https://doi.org/10.1080/10428194.2020.1827248.
Decroocq J, Itzykson R, Vigouroux S, Michallet M, Yakoub-Agha I, Huynh A, et al. Similar outcome of allogeneic stem cell transplantation after myeloablative and sequential conditioning regimen in patients with refractory or relapsed acute myeloid leukemia: a study from the Société Francophone de Greffe de Moelle et de Thérapie Cellula. Am J Hematol. 2018;93:416–23.
Rodríguez-Arbolí E, Labopin M, Tischer J, Brecht A, Ganser A, Finke J, et al. FLAMSA-based reduced-intensity conditioning versus myeloablative conditioning in younger patients with relapsed/refractory acute myeloid leukemia with active disease at the time of allogeneic stem cell transplantation: an analysis from the acute leukemia. Biol Blood Marrow Transpl. 2020;26:2165–73.
Rodríguez-Arbolí E, Labopin M, Eder M, Brecht A, Blau IW, Huynh A, et al. Augmented FLAMSA-Bu versus FluBu2 reduced-intensity conditioning in patients with active relapsed/refractory acute myeloid leukemia: an EBMT analysis. Bone Marrow Transpl. 2022;57:934–41.
Battipaglia G, Labopin M, Kröger N, Vitek A, Afanasyev B, Hilgendorf I, et al. Posttransplant cyclophosphamide vs antithymocyte globulin in HLA-mismatched unrelated donor transplantation. Blood. 2019;134:892–9.
Shah R, Murphy D, Logue M, Jerkins J, Jallouk A, Adetola K, et al. Multidisciplinary management of morbidities associated with chronic graft-versus-host disease. Clin Hematol Int. 2024;6:1–15.
Kröger N, Solano C, Wolschke C, Bandini G, Patriarca F, Pini M, et al. Antilymphocyte globulin for prevention of chronic graft-versus-host disease. N Engl J Med. 2016;374:43–53.
Schmaelter AK, Labopin M, Socié G, Itälä-Remes M, Blaise D, Yakoub-Agha I, et al. Inferior outcome of allogeneic stem cell transplantation for secondary acute myeloid leukemia in first complete remission as compared to de novo acute myeloid leukemia. Blood Cancer J. 2020;10. Available from: https://doi.org/10.1038/s41408-020-0296-3.
Kreidieh F, Abou Dalle I, Moukalled N, El-Cheikh J, Brissot E, Mohty M, et al. Relapse after allogeneic hematopoietic stem cell transplantation in acute myeloid leukemia: an overview of prevention and treatment. Int J Hematol. 2022;116:330–40. https://doi.org/10.1007/s12185-022-03416-7.
Schlenk RF, Weber D, Fiedler W, Salih HR, Wulf G, Salwender H, et al. Midostaurin added to chemotherapy and continued single-agent maintenance therapy in acute myeloid leukemia with FLT3-ITD. Blood. 2019;133:840–51.
Burchert A, Bug G, Fritz LV, Finke J, Stelljes M, Röllig C, et al. Sorafenib maintenance after allogeneic hematopoietic stem cell transplantation for acute myeloid leukemia with FLT3-internal tandem duplication mutation (SORMAIN). J Clin Oncol. 2020;38:2993–3002.
Craddock C, Jilani N, Siddique S, Yap C, Khan J, Nagra S, et al. Tolerability and clinical activity of post-transplantation azacitidine in patients allografted for acute myeloid leukemia treated on the RICAZA trial. Biol Blood Marrow Transpl. 2016;22:385–90. https://doi.org/10.1016/j.bbmt.2015.09.004.
Wei Y, Xiong X, Li X, Lu W, He X, Jin X, et al. Low-dose decitabine plus venetoclax is safe and effective as post-transplant maintenance therapy for high-risk acute myeloid leukemia and myelodysplastic syndrome. Cancer Sci. 2021;112:3636–44.
Guillaume T, Malard F, Magro L, Labopin M, Tabrizi R, Borel C, et al. Prospective phase II study of prophylactic low-dose azacitidine and donor lymphocyte infusions following allogeneic hematopoietic stem cell transplantation for high-risk acute myeloid leukemia and myelodysplastic syndrome. Bone Marrow Transpl. 2019;54:1815–26. https://doi.org/10.1038/s41409-019-0536-y.
Nagler A, Tsirigotis P. Donor lymphocyte infusion (DLI) post haploidentical stem cell transplantation (Haplo) with post-transplant cyclophosphamide (PTCy): crossing the human leukocyte antigen (HLA) barrier. Bone Marrow Transpl. 2022;57:1640–1.
Acknowledgements
We thank all the EBMT participating centers for providing patients to the study.
Author information
Authors and Affiliations
Contributions
KB, ML, and MM designed the study and/or analyzed the data. KB wrote the manuscript. NK, JF, MS, AG, WB, HE, JS, RF, PJ, TS, JC, ME, JP, EF, JT were the principal investigators at the centers recruiting the highest number of patients for the study, provided important clinical data and critically revised the manuscript. MM, FC and AN approved the final version of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All methods were performed in accordance with the relevant guidelines and regulations. The scientific board of the ALWP of the EBMT approved this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barbullushi, K., Labopin, M., Kröger, N. et al. Outcomes of allogeneic hematopoietic stem cell transplantation from different donor types in primary refractory acute myeloid leukemia: a report from the ALWP of the EBMT. Bone Marrow Transplant (2025). https://doi.org/10.1038/s41409-025-02740-w
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41409-025-02740-w