Abstract
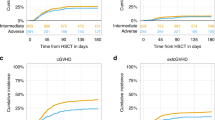
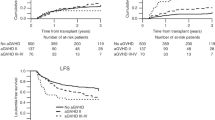
The interplay between graft-versus-host disease (aGVHD) and the graft-versus-leukemia (GVL) effect in children with acute myeloid leukemia (AML) undergoing allogeneic hematopoietic stem cell transplantation (HSCT) remains complex. This EBMT Pediatric Diseases Working Party (PDWP) retrospective analysis of 2374 pediatric AML patients evaluated the impact of aGVHD on relapse incidence (RI), non-relapse mortality (NRM), overall survival (OS), and leukemia-free survival (LFS). Grade III/IV aGVHD significantly reduced RI (HR: 0.61, p = 0.01) while significantly increasing NRM (HR: 4.51, p < 0.001), offsetting any benefits in OS and LFS. Grade II aGVHD increased NRM (HR: 2.07, p = 0.002) without affecting RI or OS, while grade I aGVHD had no significant impact on these outcomes. Patients with Grade II or higher aGVHD were at greater risk of both chronic (c)GvHD (HR: 1.98 for Grade II; HR: 4.33 for Grade III/IV, p < 0.001) and extensive cGVHD (HR: 2.52 for Grade II; HR: 4.91 for Grade III/IV, p < 0.001). These findings highlight the challenge of mitigating NRM while preserving the GVL effect to optimize disease control and long-term survival in pediatric AML. This study provides critical insights for refining post-transplant strategies in this population.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
In order to have access to the data, a request has to be made to the chair of the PDWP of EBMT and the study coordinator. The scientific boards of the PDWP of the EBMT approved this study. All the analyses were performed according to the EBMT guidelines. EBMT minimum essential data forms are submitted to the registry by transplant Center personnel following written informed consent from patients in accordance with the Centers’ ethical research guidelines.
References
Kaspers GJL, Zimmermann M, Reinhardt D, Gibson BES, Tamminga RYJ, Aleinikova O, et al. Improved outcome in pediatric relapsed acute myeloid leukemia: results of a randomized trial on liposomal daunorubicin by the International BFM Study Group. J Clin Oncol. 2013;31:599–607.
Alexander TB, Wang L, Inaba H, Triplett BM, Pounds S, Ribeiro RC, et al. Decreased relapsed rate and treatment-related mortality contribute to improved outcomes for pediatric acute myeloid leukemia in successive clinical trials. Cancer. 2017;123:3791–8.
Rasche M, Zimmermann M, Borschel L, Bourquin JP, Dworzak M, Klingebiel T, et al. Successes and challenges in the treatment of pediatric acute myeloid leukemia: a retrospective analysis of the AML-BFM trials from 1987 to 2012. Leukemia. 2018;32:2167–77.
Webb DKH, Wheatley K, Harrison G, Stevens RF, Hann IM. Outcome for children with relapsed acute myeloid leukaemia following initial therapy in the Medical Research Council (MRC) AML 10 trial. MRC Childhood Leukaemia Working Party. Leukemia. 1999;13:25–31.
Sander A, Zimmermann M, Dworzak M, Fleischhack G, von Neuhoff C, Reinhardt D, et al. Consequent and intensified relapse therapy improved survival in pediatric AML: results of relapse treatment in 379 patients of three consecutive AML-BFM trials. Leukemia. 2010;24:1422–8.
Gorman MF, Ji L, Ko RH, Barnette P, Bostrom B, Hutchinson R, et al. Outcome for children treated for relapsed or refractory acute myelogenous leukemia (rAML): a Therapeutic Advances in Childhood Leukemia (TACL) Consortium study. Pediatr Blood Cancer. 2010;55:421–9.
Abrahamsson J, Clausen N, Gustafsson G, Hovi L, Jonmundsson G, Zeller B, et al. Improved outcome after relapse in children with acute myeloid leukaemia. Br J Haematol. 2007;136:229–36.
Lund TC, Ahn KW, Tecca HR, Hilgers MV, Abdel-Azim H, Abraham A, et al. Outcomes after second hematopoietic cell transplantation in children and young adults with relapsed acute leukemia. Biol Blood Marrow Transpl. 2019;25:301–6.
O’Hare P, Lucchini G, Cummins M, Veys P, Potter M, Lawson S, et al. Allogeneic stem cell transplantation for refractory acute myeloid leukemia in pediatric patients: the UK experience. Bone Marrow Transpl. 2017;52:825–31.
Pession A, Masetti R, Rizzari C, Putti MC, Casale F, Fagioli F, et al. Results of the AIEOP AML 2002/01 multicenter prospective trial for the treatment of children with acute myeloid leukemia. Blood. 2013;122:170–8.
Mo XD, Xu LP, Zhang XH, Liu DH, Wang Y, Chen H, et al. Chronic GVHD induced GVL effect after unmanipulated haploidentical hematopoietic SCT for AML and myelodysplastic syndrome. Bone Marrow Transpl. 2015;50:127–33. https://doi.org/10.1038/bmt.2014.223.
Weisdorf D, Zhang MJ, Arora M, Horowitz MM, Rizzo JD, Eapen M. Graft-versus-host disease induced graft-versus-leukemia effect: greater impact on relapse and disease-free survival after reduced intensity conditioning. Biol Blood Marrow Transpl. 2012;18:1727–33.
Baron F, Labopin M, Niederwieser D, Vigouroux S, Cornelissen JJ, Malm C, et al. Impact of graft-versus-host disease after reduced-intensity conditioning allogeneic stem cell transplantation for acute myeloid leukemia: a report from the Acute Leukemia Working Party of the European group for blood and marrow transplantation. Leukemia. 2012;26:2462–8.
Storb R, Gyurkocza B, Storer BE, Sorror ML, Blume K, Niederwieser D, et al. Graft-versus-host disease and graft-versus-tumor effects after allogeneic hematopoietic cell transplantation. J Clin Oncol. 2013;31:1530–8.
Horowitz MM, Gale RP, Sondel PM, Goldman JM, Kersey J, Kolb HJ, et al. Graft-versus-leukemia reactions after bone marrow transplantation. Blood. 1990;75:555–62.
Sweeney C, Vyas P. The graft-versus-leukemia effect in AML. Front Oncol. 2019;9:1217. https://doi.org/10.3389/fonc.2019.01217.
Devillier R, Galimard JE, Labopin M, Blaise D, Raiola AM, Pavlu J, et al. Reduced intensity versus non-myeloablative conditioning regimen for haploidentical transplantation and post-transplantation cyclophosphamide in complete remission acute myeloid leukemia: a study from the ALWP of the EBMT. Bone Marrow Transpl. 2022;57:1421–7. https://doi.org/10.1038/s41409-022-01674-x.
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen, et al, National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: I. The 2014 Diagnosis and Staging Working Group report. Biol Blood Marrow Transpl. 2015;2:389–401.e1. https://doi.org/10.1016/j.bbmt.2014.12.001.
Weischendorff S, Kamari-Kany N, Kielsen K, Ifversen M, Müller K. Diagnosing Acute Graft-Versus-Host Disease in Children Undergoing Hematopoietic Stem Cell Transplantation-Comparison of the Modified Glucksberg Criteria Versus the MAGIC Criteria. Pediatr Blood Cancer. 2025;72:e31502. https://doi.org/10.1002/pbc.31502.
Kato M, Kurata M, Kanda J, Kato K, Tomizawa D, Kudo K, et al. Impact of graft-versus-host disease on relapse and survival after allogeneic stem cell transplantation for pediatric leukemia. Bone Marrow Transpl. 2019;54:68–75.
van Besien K. Allogeneic transplantation for AML and MDS: GVL versus GVHD and disease recurrence. Hematol Am Soc Hematol Educ Program. 2013;2013:56–62.
Benetton M, Merli P, Walter C, Hansen M, da Ros A, Polato K, et al. Molecular measurable residual disease assessment before hematopoietic stem cell transplantation in pediatric acute myeloid leukemia patients: a retrospective study by the I-BFM Study Group. Biomedicines. 2022;10.
Kayser S, Schlenk RF, Grimwade D, Yosuico VED, Walter RB. Minimal residual disease-directed therapy in acute myeloid leukemia. Blood. 2015;125:2331–5.
Kayser S, Benner A, Thiede C, Martens U, Huber J, Stadtherr P, et al. Pretransplant NPM1 MRD levels predict outcome after allogeneic hematopoietic stem cell transplantation in patients with acute myeloid leukemia. Blood Cancer J. 2016;6.
Molina B, Gonzalez Vicent M, Herrero B, Deltoro N, Ruiz J, Perez Martinez A, et al. Kinetics and risk factors of relapse after allogeneic stem cell transplantation in children with leukemia: a long-term follow-up single-center study. Biol Blood Marrow Transpl. 2019;25:100–6.
van Weelderen RE, Klein K, Harrison CJ, Jiang Y, Abrahamsson J, Arad-Cohen N, et al. Residual disease and fusion partner independently predict survival and relapse risk in childhood KMT2A-rearranged acute myeloid leukemia: A Study by the International Berlin-Frankfurt-Münster Study Group. J Clin Oncol. 2023;41:2963–74. https://doi.org/10.1200/JCO.22.02120.
Bertaina A, Zecca M, Buldini B, Sacchi N, Algeri M, Saglio F, et al. Unrelated donor vs HLA-haploidentical α/β T-cell- and B-cell-depleted HSCT in children with acute leukemia. Blood. 2018;132:2594–607.
Locatelli F, Merli P, Pagliara D, Li Pira G, Falco M, Pende D, et al. Outcome of children with acute leukemia given HLA-haploidentical HSCT after αβ T-cell and B-cell depletion. Blood. 2017;130:677–85.
Tabata R, Chi S, Yuda J, Minami Y. Emerging Immunotherapy for Acute Myeloid Leukemia. Int J Mol Sci. 2021;22:1–20.
Aydin M, de Leeuw DC, Rutten CE, Visser OJ, Tang MW, van Roessel C, et al. ATG versus PTCy in matched unrelated donor haematopoietic stem cell transplantations with non-myeloablative conditioning. Br J Haematol. 2023;203:439–45. https://doi.org/10.1111/bjh.19031.
Heelan F, Mallick R, Bryant A, Radhwi O, Atkins H, Huebsch L, et al. Does Lymphocyte Count Impact Dosing of Anti-Thymocyte Globulin in Unrelated Donor Stem Cell Transplantation?. Biol Blood Marrow Transpl. 2020;26:1298–302. https://doi.org/10.1016/j.bbmt.2020.02.026.
Kennedy VE, Chen H, Savani BN, Greer J, Kassim AA, Engelhardt BG, et al. Optimizing antithymocyte globulin dosing for unrelated donor allogeneic hematopoietic cell transplantation based on recipient absolute lymphocyte count. Biol Blood Marrow Transpl. 2018;24:150–5. https://doi.org/10.1016/j.bbmt.2017.08.029.
Grasso AG, Simeone R, Maestro A, Zanon D, Maximova N. Pre-transplant total lymphocyte count determines anti-thymocyte globulin exposure, modifying graft-versus-host disease incidence and post-transplant thymic restoration: a single-center retrospective study. J Clin Med. 2023;12:730.
Zeiser R, von Bubnoff N, Butler J, Mohty M, Niederwieser D, Or R, et al. REACH2 Trial Group. Ruxolitinib for Glucocorticoid-Refractory Acute Graft-versus-Host Disease. N Engl J Med. 2020;382:1800–10. https://doi.org/10.1056/NEJMoa1917635.
Mozo Y, Bueno D, Sisinni L, Fernández-Arroyo A, Rosich B, Martínez AP, et al. Ruxolitinib for steroid-refractory graft versus host disease in pediatric HSCT: high response rate and manageable toxicity. Pediatr Hematol Oncol. 2021;38:331–45. https://doi.org/10.1080/08880018.2020.1868637.
Aureli A, Marziani B, Sconocchia T, del Principe MI, Buzzatti E, Pasqualone G, et al. Immunotherapy as a Turning Point in the Treatment of Acute Myeloid Leukemia. Cancers. 2021;13.
Daver N, Alotaibi AS, Bücklein V, Subklewe M. T-cell-based immunotherapy of acute myeloid leukemia: current concepts and future developments. Leukemia. 2021;35:1843–63.
Acknowledgements
The authors want to acknowledge all contributing Centers. The authors declare that they have no relevant conflict of interest and no competing financial interests.
Author information
Authors and Affiliations
Contributions
AB, MM, SC, KK, JEG, AD and GL designed the study and wrote the first version of the manuscript. MM completed the data interpretation and contributed to writing the final version of the manuscript. JEG performed all statistical analyses. KK (Kleinschmidt), MA, MB, OMD, DP, JHD, AAA, ES, CR, JS, RR, RF, AB, CJ, EG, MI, AL, BV, MA and PB provided clinical data and reviewed the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bertaina, A., Maffeis, M., Lucchini, G. et al. Interplay between acute graft-versus-host disease and graft-versus-leukemia effect in pediatric acute myeloid leukemia patients undergoing allogeneic hematopoietic stem cell transplantation: implications for relapse incidence and survival – an EBMT PDWP retrospective study. Bone Marrow Transplant (2025). https://doi.org/10.1038/s41409-025-02748-2
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41409-025-02748-2