Abstract
Objectives The oral cavity is a potential reservoir for respiratory pathogens which can predispose patients to bacterial super-infection. Several trials have correlated poor oral hygiene with hyper-inflammation. Similarly, COVID-19 severity has been linked to hyper-inflammatory responses. Hence, in this study, we assumed that increased COVID-19 severity may be linked to poor oral health status. This was achieved through assessing oral health status, severity of COVID-19 symptoms, C-reactive protein (CRP) levels and duration of recovery.
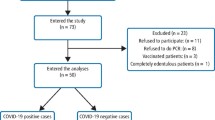
Methods Cross-sectional study based on a questionnaire; 308 Egyptian patients with confirmed positive polymerase chain reaction (PCR) tests were included in the study after exclusion criteria. The questionnaire was designed with two sections: the first section for oral health evaluation and the second section for COVID-19 severity evaluation. Assessment of the effect of oral health on COVID-19 severity was performed using an oral health score. The effect of oral health on CRP and recovery period were evaluated as secondary endpoints. Data of CRP levels and COVID-19 PCR tests were collected via the questionnaire and confirmed by reviewing medical records.
Results The correlation between oral health and COVID-19 severity showed a significant inverse correlation (p <0.001, r = -0.512). Moreover, the correlation between oral health with recovery period and CRP values also revealed a significant inverse correlation (p <0.001, -0.449 and p <0.001, -0.190, respectively), showing that poor oral health was correlated to increased values of CRP and delayed recovery period.
Conclusions Our study provided some evidence that oral health could have a potential impact on the severity of COVID-19. However, the correlation is limited by the study design. A more substantial research project is required to address this relation.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
World Health Organisation. Novel coronavirus (2019-nCoV) situation report 22. 2020. Available online at https://apps.who.int/iris/handle/10665/330991 (accessed April 2020).
World Health Organisation. Coronavirus disease (COVID-19) pandemic. 2020. Available at https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed April 2020).
World Health Organisation. Coronavirus Disease (COVID-19) Dashboard. 2020. Available online at https://covid19.who.int/ (accessed January 2021).
Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol 2020; 92: 568-576.
Sinha P, Matthay M A, Calfee C S. Is a "Cytokine Storm" Relevant to COVID-19? JAMA Intern Med 2020; 180: 1152-1154.
Tay M, Poh C, Rénia L, MacAry P, Ng L. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol 2020; 20: 363-374.
Lia Q, Dinga X, Xiab G et al. Eosinopenia and elevated C-reactive protein facilitate triage of COVID-19 patients in fever clinic: A retrospective case-control study. EClinicalMedicine 2020; DOI: 10.1016/j.eclinm.2020.100375.
Huang C, Wang Y, Li X et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497-506.
Centers for Disease Control and Prevention. CDC updates, expands list of people at risk of severe COVID-19 illness. 2020. Available at https://www.cdc.gov/media/releases/2020/p0625-update-expands-covid-19.html (accessed January 2021).
Olsen I, Yamazaki K. Can oral bacteria affect the microbiome of the gut? J Oral Microbiol 2019; DOI: 10.1080/20002297.2019.1586422.
Joshipura K, Ritchie C, Douglass C. Strength of Evidence Linking Oral Conditions and Systemic Disease. Compend Contin Educ Dent Suppl 2000; 30: 12-23; quiz 65.
Scannapieco F A. Role of Oral Bacteria in Respiratory Infection. J Periodontol 1999; 70: 793-802.
Imsand M, Janssens J P, Auckenthaler R, Mojon P, Budtz-Jørgensen E. Bronchopneumonia and oral health in hospitalised older patients. A pilot study. Gerodontology 2002; 19: 66-72.
Aas J A, Paster B J, Stokes L N, Olsen I, Dewhirst F E. Defining the normal bacterial flora of the oral cavity. J Clin Microbiol 2005; 43: 5721-5732.
Feng Y, Ling Y, Bai T et al. COVID-19 with different severities: a multi-centre study of clinical features. Am J Respir Crit Care Med 2020; 201: 1380-1388.
Fajnzylber J, Regan J, Coxen K et al. SARS-CoV-2 viral load is associated with increased disease severity and mortality. Nature Commun 2020; DOI: 10.1038/s41467-020-19057-5.
Liu Y, Yan L, Wan L et al. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect Dis 2020; 20: 656-657.
World Health Organisation. Egypt releases results of epidemiological study on oral health status. 2014. Available at http://www.emro.who.int/egy/egypt-events/results-of-epidemiological-study-on-oral-health-status-released.html (accessed January 2021).
Levin L, Shpigel I, Peretz B. The use of a self-report questionnaire for dental health status assessment: a preliminary study. Br Dent J 2013; 214: E15.
Ruíz-López del Prado G, Blaya-Nováková V, Saz-Parkinson Z et al. Design and validation of an oral health questionnaire for preoperative anaesthetic evaluation. Braz J Anesthesiol 2017; 67: 6-14.
Verity R, Okell L, Dorigatti I et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis 2020; 20: 669-677.
Wang D, Hu B, Hu C et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020; 323: 1061-1069.
World Health Organisation. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). 2020. Available at https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf (accessed August 2020).
Worldometer. Coronavirus Symptoms (COVID-19). 2020. Available at https://www.worldometers.info/coronavirus/coronavirus-symptoms/?fbclid=IwAR19aftSD5oeads4bkyvmPfydVFhYjQLVUlAcgilCaJ7oFI4M (accessed April 2020).
Robert Koch Institut. Information and assistance for people with a higher risk of severe COVID-19 disease. 2020. Available at https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Risikogruppen.htm (accessed June 2020).
NICE. COVID-19 rapid guideline: managing suspected or confirmed pneumonia in adults in the community - Treatment and care planning. 2020. Available online at https://www.nice.org.uk/guidance/ng165/chapter/2-Treatment-and-care-planning (accessed August 2020).
Greenhalgh T, Koh G, Car J. Covid-19: a remote assessment in primary care. BMJ 2020; DOI: 10.1136/bmj.m1182.
The Centre for Evidence-Based Medicine. Are there any evidence-based ways of assessing dyspnoea (breathlessness) by telephone or video. 2020. Available at https://www.cebm.net/covid-19/are-there-any-evidence-based-ways-of-assessing-dyspnoea-breathlessness-by-telephone-or-video/ (accessed April 2020).
Chorin E, Padegimas A, Havakuk O et al. Assessment of Respiratory Distress by the Roth Score. Clin Cardiol 2016; 39: 636-639.
Loesche W J. Association of the oral flora with important medical diseases. Curr Opin Periodontol 1997; 4: 21-28.
Van Dyke T E, Dowell Jr V R, Offenbacher S, Snyder W, Hersh T. Potential role of microorganisms isolated from periodontal lesions in the pathogenesis of inflammatory bowel disease. Infect Immun 1986; 53: 671-677.
Page R C. The pathobiology of periodontal diseases may affect systemic diseases: inversion of a paradigm. Ann Periodontol 1998; 3: 108-120.
Genco R J. Periodontal disease and risk for myocardial infarction and cardiovascular disease. Cardiovasc Rev Rep 1998; 19: 34-37.
Wang S, Lin D, Yang X et al. Prognostic value of C-reactive protein in patients with COVID-19. Infect Dis 2020; 9: 2445-2453.
Chakraborty S. Metagenome of SARS-Cov2 patients in Shenzhen with travel to Wuhan shows a wide range of species - Lautropia, Cutibacterium, Haemophilus being most abundant - and Campylobacter explaining diarrhea. 2020. Available online at https://www.researchgate.net/publication/340152514_Metagenome_of_SARS-Cov2_patients_in_Shenzhen_with_travel_to_Wuhan_shows_a_wide_range_of_species_-_Lautropia_Cutibacterium_Haemophilus_being_most_abundant_-_and_Campylobacter_explaining_diarrhea (accessed January 2021).
Khan A A, Khan Z. COVID-2019 associated overexpressed Prevotella proteins mediated host-pathogen interactions and their role in coronavirus outbreak. Bioinformatics 2020; 36: 4065-4069.
Cox M, Loman N, Bogaert D, O'Grady J. Co-infections: potentially lethal and unexplored in COVID-19. Lancet Microbe 2020; DOI: 10.1016/S2666-5247(20)30009-4.
Zhang H, Zhang Y, Wu J et al. Risks and features of secondary infections in severe and critical ill COVID-19 patients. Emerg Microbes Infect 2020; 9: 1958-1964.
Paju S, Scannapieco F. Oral biofilms, periodontitis, and pulmonary infections. Oral Dis 2007; 13: 508-512.
Yang Y, Li W, Wang Z M, Sun G Y, Zhou P, Han X L. Clinical significance of interleukin-6 and-8 in patients with chronic periodontal disease and acute exacerbation of chronic obstructive pulmonary disease. Zhonghua Kou Qiang Yi Xue Za Zhi 2018; 53: 312-317.
Wölfel R, Corman V M, Guggemos W et al. Virological assessment of hospitalized patients with COVID-2019. Nature 2020; 581: 465-469.
Pujadas E, Chaudhry F, McBride R et al. SARS-CoV-2 viral load predicts COVID-19 mortality. Lancet Respir Med 2020; DOI: 10.1016/S2213-2600(20)30354-4.
Meister T, Brüggemann Y, Todt D et al. Virucidal Efficacy of Different Oral Rinses Against Severe Acute Respiratory Syndrome Coronavirus 2. J Infect Dis 2020; 222: 1289-1292.
Xu H, Zhong L, Deng J et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci 2020; 12: 8.
Parhar H S, Tasche K, Brody R M et al. Topical preparations to reduce SARS-CoV-2 aerosolization in head and neck mucosal surgery. Head Neck 2020; 42: 1268-1272.
Yoon J G, Yoon J, Song J Y et al. Clinical Significance of a High SARS-CoV-2 Viral Load in the Saliva. J Korean Med Sci 2020; DOI: 10.3346/jkms.2020.35.e195.
Gao Y, Li T, Han M et al. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J Med Virol 2020; 92: 791-796.
Wang L. C-reactive protein levels in the early stage of COVID-19. Med Mal Infect 2020; 50: 332-334.
Meselson M. Droplets and Aerosols in the Transmission of SARS-CoV-2. N Engl J Med 2020; 382: 2063.
Marnell L, Mold C, Du Clos T. C-reactive protein: Ligands, receptors and role in inflammation. Clin Immunol 2005; 117: 104-111.
Sahu B, Kampa R, Padhi A, Panda A. C-reactive protein: A promising biomarker for poor prognosis in COVID-19 infection. Clin Chim Acta 2020; 509: 91-94.
Wang G, Wu C, Zhang Q et al. C-Reactive Protein Level May Predict the Risk of COVID-19 Aggravation. Open Forum Infect Dis 2020; DOI: 10.1093/ofid/ofaa153.
Jones J F, Miller B D. The Postviral Asthenia Syndrome. In Kurstak E, Lipowski Z J, Morozov P V (eds) Viruses, Immunity, and Mental Disorders. pp 441-451. Boston, MA: Springer, 1986.
Meng L, Hua F, Bian Z. Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J Dent Res 2020; 99: 481-487.
da Costa C, Peralta F, Ferreira de Mello A. How Has Teledentistry Been Applied in Public Dental Health Services? An Integrative Review. Telemed J E Health 2020; 26: 945-954.
Acknowledgements
The authors thank the study participants for their contribution. We express our appreciation and supportiveness to all frontline healthcare workers during the COVID-19 pandemic.
Author information
Authors and Affiliations
Contributions
Amany Hany Mohamed Kamel: conceptualisation, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualisation, roles/writing - original draft, writing - review and editing. Ahmed Basuoni: conceptualisation, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualisation, roles/writing - original draft, writing - review and editing. Zeinab A. Salem: data curation, investigation, project administration, software, supervision, validation, visualisation, writing - review and editing. Nermeen AbuBakr: conceptualisation, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualisation, roles/writing - original draft, writing - review and editing.
Corresponding author
Ethics declarations
The authors declare that they have no conflict of interest. No financial aid or support was received.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Kamel, A., Basuoni, A., Salem, Z. et al. The impact of oral health status on COVID-19 severity, recovery period and C-reactive protein values. Br Dent J (2021). https://doi.org/10.1038/s41415-021-2656-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41415-021-2656-1
This article is cited by
-
The ROOT-CTRCD study: exploring the relationship of oral health to cancer therapy-related cardiac dysfunction in HER2-positive breast cancer patients
Cardio-Oncology (2026)
-
Oral hygiene influence on the incidence and severity of oral manifestations in Coronavirus Disease 2019
BMC Oral Health (2025)
-
The impact of COVID-19 on the oral health self-care practices of Australian adults
Journal of Public Health (2024)
-
The impact of periodontal disease on the clinical outcomes of COVID-19: A systematic review and meta-analysis
BMC Oral Health (2023)
-
Australian nursing students’ perception, knowledge, and attitude towards oral healthcare of older people and associated factors: a national cross-sectional survey
BMC Nursing (2023)