Abstract
Aims and objectives The aim of this Plan-Do-Study-Act cycle was to establish if undergraduate students believe they have a role to play in suicide risk assessment, and to discuss the implementation of suicide risk prevention into the undergraduate dental curriculum. Data gathered informed development of a subsequent suicide risk assessment educational workshop.
Methodology An online questionnaire was disseminated to undergraduate students as part of a quality improvement service evaluation within a UK dental hospital and school. This sought to gain information on attitudes to suicide prevention, previous suicide awareness training, and the appetite and potential barriers to future training.
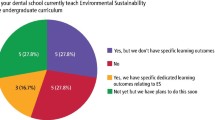
Results A response rate of 23% (n = 30) was achieved. In total, 87% of undergraduate students responding reported having no experience or training in the identification of suicidal patients, 97% of respondents expressed a desire for training, and 80% stated not knowing what to do if a patient disclosed suicidal thoughts during an appointment.
Conclusion The dental team have a role to play in suicide risk assessment and the signposting of at-risk patients to appropriate services. To embed this within daily practice, awareness and training must be introduced to undergraduate curricula.
Key points
-
Dental professionals have an increasingly important role to play in suicide awareness, risk assessment and signposting patients when needed to appropriate services.
-
Dental and dental therapist graduates have varying degrees of training surrounding suicide and mental health. Suicide education rarely appears to be embedded within undergraduate dental curricula.
-
Results in a UK dental school found further education and support in providing appropriate holistic care for dental patients would be welcomed by dental and dental therapist undergraduates.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Samaritans. Latest suicide data. 2021. Available at https://www.samaritans.org/about-samaritans/research-policy/suicide-facts-and-figures/latest-suicide-data/ (accessed March 2023).
Public Health Scotland. Suicide statistics for Scotland: Update of trends for the year 2021. 2022. Available at https://publichealthscotland.scot/publications/suicide-statistics-for-scotland/suicide-statistics-for-scotland-update-of-trends-for-the-year-2021/ (accessed March 2023).
O'Connor R C, Wetherall K, Cleare S et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry 2021;218: 326-333.
Scottish Government. Suicide prevention strategy and action plan drafts: consultation. 2022. Available at https://www.gov.scot/publications/consultation-new-suicide-prevention-strategy-action-plan-scotland/ (accessed March 2023).
Mental Health Wellness in Dentistry. Mental Health Wellness in Dentistry Framework 2021. Available at https://mhwd.org/download/mental-health-wellness-in-dentistry-framework/ (accessed March 2023).
Harmer B, Lee S, Duong T V H, Saadabadi A. Suicidal Ideation. Treasure Island: StatPearls Publishing, 2023.
University of Manchester. The National Confidential Inquiry into Suicide and Homicide by People with Mental Illness. Making Mental Health Care Safer: Annual Report and 20-year Review. 2016. Available at https://documents.manchester.ac.uk/display.aspx?DocID=37580 (accessed March 2023).
UK Government. Making Every Contact Count (MECC): Consensus Statement. 2016. Available at https://www.gov.uk/government/publications/making-every-contact-count-mecc-practical-resources (accessed March 2023).
NHS Digital. NHS Dental Statistics for England - 2020-21 Annual Report. 2021. Available at https://digital.nhs.uk/data-and-information/publications/statistical/nhs-dental-statistics/2020-21-annual-report (accessed March 2023).
Dental Nursing. Dental care for adults with mental health problems. 2012. Available at https://www.dental-nursing.co.uk/features/dental-care-for-adults-with-mental-health-problems (accessed March 2023).
Osazuwa-Peters N, Simpson M C, Zhao L et al. Suicide risk among cancer survivors: Head and neck versus other cancers. Cancer 2018; 124: 4072-4079.
Elliott E, Sharma S, Omar A et al. A multi-centre early evaluation of the effectiveness of workshop teaching to improve the confidence of UK and Irish dental students when addressing patient mental health. Br Dent J 2021; DOI: 10.1038/s41415-021-3613-8.
Mind. Mental Health in Primary Care: A briefing for Clinical Commissioning Groups June 2016. 2016. Available at https://www.mind.org.uk/media-a/4409/13296_primary-care-policy_web_op.pdf (accessed March 2023).
General Dental Council. Preparing for practice: Dental team learning outcomes for registration. 2015. Available at https://www.gdc-uk.org/docs/default-source/quality-assurance/preparing-for-practice-%28revised-2015%29.pdf (accessed March 2023).
Elliott E, Sharma S, Omar A, Hurst D. How confidently do students address patients with psychiatric conditions in the dental clinic? A service evaluation in a UK dental school. Br Dent J 2020; 228: 376-380.
McHarg J, Kay E J. Designing a dental curriculum for the twenty-first century. Br Dent J 2009; 207: 493-497.
Alexander R E. Stress-related suicide by dentists and other health care workers. Fact or folklore? J Am Dent Assoc 2001; 132: 786-794.
Galán F, Ríos-Santos J-V, Polo J, Rios-Carrasco B, Bullón P. Burnout, depression and suicidal ideation in dental students. Med Oral Patol Oral Cir Bucal 2014; 19: 206-211.
Takayama Y, Miura E, Miura K, Ono S, Ohkubo C. Condition of depressive symptoms among Japanese dental students. Odontology 2011; 99: 179-187.
Brondani M A, Ramanula D, Pattanaporn K. Tackling stress management, addiction, and suicide prevention in a predoctoral dental curriculum. J Dent Educ 2014: 78: 1286-1293.
Smith A R, Silva C, Covington D W, Joiner T J. An assessment of suicide-related knowledge and skills among health professionals. Health Psychol 2014; 33: 110-119.
NHS England and NHS Improvement. Plan, Do, Study, Act (PDSA) Cycles and the model for improvement. Available at https://www.england.nhs.uk/wp-content/uploads/2022/01/qsir-pdsa-cycles-model-for-improvement.pdf (accessed March 2023).
Herron J, Ticehurst H, Appleby L, Perry A, Cordingley L. Attitudes toward suicide prevention in front-line health staff. Suicide Life Threat Behav 2001; 31: 342-347.
Galliher J M, Bonham A J, Dickinson L M, Staton E W, Pace W D. Representativeness of PBRN physician practice patterns and related beliefs: the case of the AAFP National Research Network. Ann Fam Med 2009; 7: 547-554.
Holden R R. Face Validity. In Weiner I B, Craighead W E (eds) The Corsini Encyclopaedia of Psychology. New Jersey: John Wiley & Sons, 2010.
Freeman R, Knights J, Beaton L et al. Prediction of emotional exhaustion over the course of the COVID-19 pandemic in primary care dental staff: an intensive longitudinal study. BMJ Open 2021; DOI: 10.1136/bmjopen-2021-054827.
Booker Q, Austin J, Balasubramanian B. Survey strategies to increase participant response rates in primary care research studies. Fam Pract 2021; 38: 699-702.
Velupillai S, Hadlaczky G, Baca-Garcia E et al. Risk Assessment Tools and Data-Driven Approaches for Predicting and Preventing Suicidal Behaviour. Front Psychiatry 2019; 10: 36.
Acknowledgements
The authors wish to thank Dr Lindsay-Jo Sevier-Guy for gaining permission to use 'Attitudes to suicide prevention scale' and to thank Jane Herron, Louis Appleby and co-authors of the 'Attitudes to suicide prevention scale' (Herron et al., 2001) for the permission given. Thanks are also extended to the students who responded to the service evaluation.
Author information
Authors and Affiliations
Contributions
Niamh Kelly and Julie Kilgariff were responsible for drafting and revision of the manuscript, production of the questionnaire, and collection of results.
If you have been affected by the content of this piece, you can reach out to the following support lines: The Dentists' Health Support Trust via 020 7224 4671 and The Samaritans via 116 123.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
The Health Research Authority 2017 (hra-decisiontools.org.uk) define differences between research, service evaluation and audit. NHS ethical research committee review is not required for service evaluations or research which seeks to elicit the views, experiences, knowledge and contributions of healthcare professionals on a given subject area. Confirmation that this service evaluation project did not require ethical approval was sought and granted from the local Health Board's ethics contact and thereafter, the local NHS Clinical Research Governance Group.
All participants received information resources providing details of the project, advising that completion of the service evaluation questionnaire was deemed as valid consent to take part in the project, and that anonymous findings may be included in future publications.
Rights and permissions
About this article
Cite this article
Kelly, N., Kilgariff, J. Should suicide risk assessment be embedded in undergraduate dental curricula?. Br Dent J 234, 601–605 (2023). https://doi.org/10.1038/s41415-023-5736-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41415-023-5736-6
This article is cited by
-
‘It is relevant, it is useful and we won't be scared to ask': the response of undergraduate dental students to suicide awareness education
British Dental Journal (2025)
-
Autism spectrum condition: an update for dental practitioners - Part 1
British Dental Journal (2024)